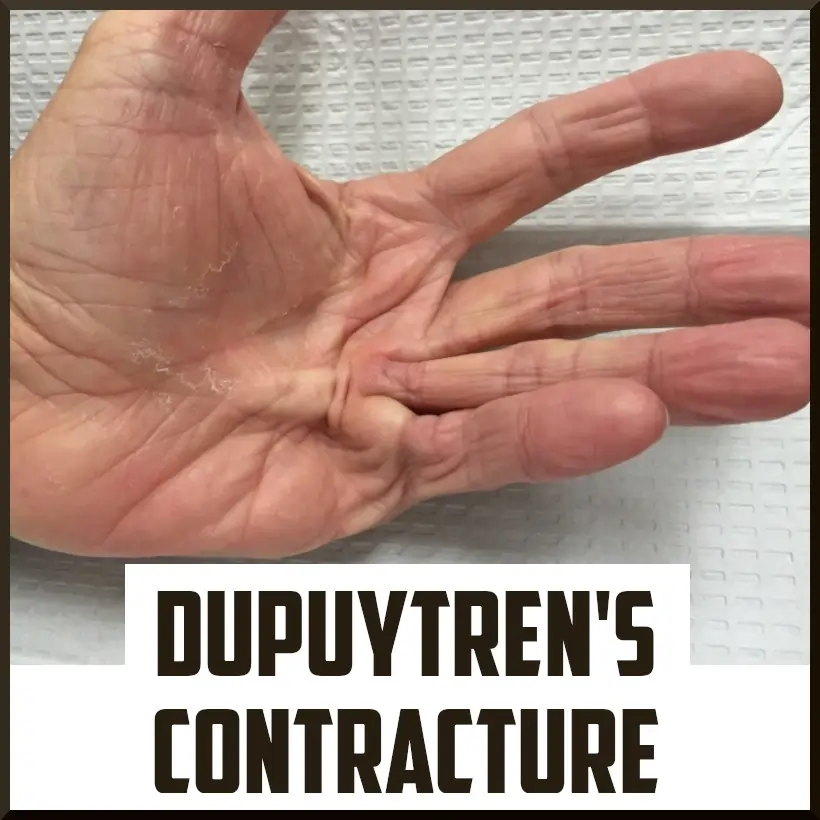
Dupuytren’s Contracture
Introduction
Dupuytren’s contracture is a condition in which the fascia (connective tissue) in the palm thickens and tightens, causing one or more fingers to bend toward the palm. It typically progresses slowly and can affect hand function over time.
In the case of Dupuytren contracture, one or more fingers bend toward the palm. The fingers that are affected cannot be straightened entirely. Tissue formations develop beneath the skin. Ultimately, they create a stable cord that can draw the fingers into a bent position. As time passes, the condition declines progressively.
The two fingers that are most distant from the thumb are the ones most commonly affected by Dupuytren contracture. This may make routine tasks like putting your hands in your pockets, donning gloves, or shaking hands more complicated.
Dupuytren contracture cannot be cured. Therapies can diminish symptoms and reduce the speed at which the condition declines. Dupuytren’s disease impacts the palmar fascia — a fibrous tissue layer beneath the skin and above the tendons, nerves, blood vessels, and bones in the palm and fingers.
For some individuals, the progression of Dupuytren’s contracture can disrupt hand function and complicate the execution of routine tasks. When this happens, both nonsurgical and surgical treatment options can help slow the progression (declines) of the disease and enhance movement in the affected fingers.
Anatomy
A layer of tissue known as the fascia serves to anchor and stabilize the skin on the palm side of the hand. The fascia keeps the skin on your palm stretched tight; without it, the skin there would be as loose and mobile as that on the back of your hand. This palmar fascia gradually becomes thicker and more contracted (shortened) in patients with Dupuytren’s disease.
The first signs of Dupuytren’s are usually the formation of tissue lumps or nodules in the palm beneath the skin. As the affected tissue pulls on the skin above it, this may result in pitting (deep dents) on the palm’s surface.
With the progression of Dupuytren’s, the fascia bands in the palm transform into thick cords that can saddle (lock) one or more fingers and the thumb in a bent position. This condition is referred to as a “Dupuytren’s contracture.” The cords in the palm may resemble tendons, but the tendons are not affected by Dupuytren’s.
In numerous instances, Dupuytren’s contracture advances (declines) at a progressive speed over several years and can remain mild enough that treatment is unnecessary. Nonetheless, in cases of moderate severity or worse, the condition complicates the process of straightening the affected fingers.
In such cases, treatment might be necessary to lessen the contracture and enhance movement in the fingers involved. As a contracture typically worsens, the involvement of the fascia enhances, and treatments are less likely to achieve a complete correction.
What does Dupuytren’s contracture refer to?
Also referred to as Dupuytren’s disease, Dupuytren’s contracture is a progressive condition characterized by the formation of collagen contracture and abnormal thickening of the fascia. Fascia is a layer of connective tissue composed of fibers that lie beneath the skin. Healthy fascia is robust, elastic, and adaptable, facilitating effortless movement. The thickening of the fascia can restrict movement and limit flexibility.
The ring and pinky fingers of the hand are usually affected by Dupuytren’s contracture. Other fingers may also be affected, and Dupuytren’s contracture can, in rare instances, develop in the feet. It is possible to have a Dupuytren contracture in both hands simultaneously. With the advancement of this condition, the thickened fascia develops into a cord that draws the fingers either sideways or toward the palm.
Many routine tasks, like shaking hands or typing, can be restricted by a Dupuytren’s contracture. Even though this condition cannot be cured, treatments exist to assist in managing the symptoms.
Causes
While the precise cause of Dupuytren’s disease remains unclear, the majority of evidence suggests that genetics plays a crucial role.
Dupuytren’s may develop or worsen after an individual sustains an injury or open wound (including surgery) to their hand; yet, reliable evidence to back this up is lacking. Additionally, there are no credible indications that it results from excessive use of the hand.
Additional elements that increase the probability of acquiring Dupuytren’s contract include:
- Smoking.
- Drinking.
- Diabetes.
- High cholesterol.
- A lower body mass index.
- Thyroid conditions.
- Liver disease.
- Metabolic conditions.
- Taking seizure medications long term.
- Taking antiretroviral medications long term.
- Having poor blood circulation in the hand.
Symptoms
The worsening of Dupuytren contracture occurs gradually over an amplitude of years. It starts with a solid lump in the palm. This lump may cause pain or not. With time, the lump may develop into a hard cord beneath the skin and extend into the finger. This cord constricts and draws the finger toward the palm, occasionally with great intensity.
It is possible that Dupuytren contracture does not have any noticeable effects on your body. With mild symptoms, you might not even realize you have it. Even if symptoms are present, they typically develop over a long period (months or years). In advanced stages, you may find it difficult or even impossible to straighten your affected fingers.
Any of your fingers, including the thumb, can be affected by Dupuytren contracture. It is most commonly found in people’s fingers, in the following order:
- Ring (fourth finger).
- Pinkie (fifth finger).
- Middle (third finger).
- Index (second finger).
- Thumb (first finger).
The two fingers that are the furthest from the thumb are the ones most often affected by Dupuytren contracture. The condition frequently manifests in both hands. Over several years, a Dupuytren’s contracture usually develops (and worsens) at a progressive speed. Manifestations and indications of the condition might include:
- Nodule. You can develop one or more small lumps or nodules in your palm. These nodules are generally attached to the skin above them. At first, the nodules might feel sensitive to the touch. Usually, this tenderness disappears over time. In certain instances, the skin around the nodules may exhibit “pitting” or deep incisions.
- Cord. The nodules can become thicker and contract, aiding in the development of dense, tough cords of tissue beneath the skin. The fingers and thumb may not be able to straighten or spread apart because of these cords.
- Contractures. As the tissue beneath the skin tightens, one or more fingers may be drawn toward your palm, making it difficult to spread them apart. Although the ring and little (pinky) fingers are usually affected, any combination of fingers and the thumb can be involved.
In the case of a finger being affected by Dupuytren’s contracture:
- The joint that is most frequently affected is the metacarpophalangeal (MCP) joint. This is the knuckle, the joint connecting the hand and finger.
- The proximal interphalangeal (PIP) joint is the next most commonly affected joint. After the MCP joint, this is the next joint located at the center of the finger.
Additional symptoms
- Inflammation or swelling.
- Tenderness.
- Pain or burning.
- Itching.
These symptoms rarely happen. Only about 25% of individuals with Dupuytren contracture will have these experiences. If you have Dupuytren contracture and experience these symptoms, consult your provider, as they can indicate other issues that may affect your skin or fascia.
Diagnosis
Your hand will be examined by your healthcare provider. Your thumb and fingers will be tested for flexibility and sensation. Your grip strength and pinch strength may also be evaluated.
Your healthcare provider will assess and document the positions of nodules and bands on your palm. They will use a special tool to assess the degree of curling or contracting of your fingers. The extent of movement in your fingers can also be assessed. Later measurements will be compared to these to determine if the disease worsens. Additionally, they can be utilized to determine whether the treatment is effective.
Examination
Your physician will probably discuss your overall health and medical history with you, as well as inquire about your symptoms. Since Dupuytren’s can be hereditary, your doctor may inquire whether you know of any family members who have the condition.
Your doctor will subsequently assess your hand and fingers. During the test, they will probably:
Note where nodules and cords are situated on your palm, assess the motion range of your thumb and fingers and examine sensation in your thumb and fingers. If necessary, take clinical photos to record how your hand looks. These measurements can be compared with others taken during your treatment to assess whether the condition is progressing (worsening) over time.
Treatment
At present, Dupuytren’s cannot be cured; nonetheless, the condition does not threaten life or limbs. Dupuytren’s is a non-cancerous condition that does not metastasize to the heart, lungs, brain, or other organs.
Dupuytren generally progresses slowly and may not cause problems for many years, although its effects differ among patients. For certain patients, the condition may not advance beyond the formation of lumps in the palm. Should the condition worsen, your doctor might initially suggest nonsurgical treatments to help slow the progression of the disease.
Nonsurgical Treatment
Physical therapy.
- Finger and hand exercises

Patients need to continue gentle stretching and strengthening exercises for up to 6 months after surgery, even after they have regained full use of the hand. The therapist will suggest stretching and straightening movements for each finger. These include finger spreading, straightening and flexing each finger, full-finger bending, and hook-finger bending.
For the hand, workouts consist of creating repeated fists of various dimensions. To form a fist, a pen or marker can also be used to roll the fingers. These exercises are performed approximately every 2 hours on average. The therapist will determine how often and how many times this is done according to the patient’s capabilities.
- Tendon gliding exercises
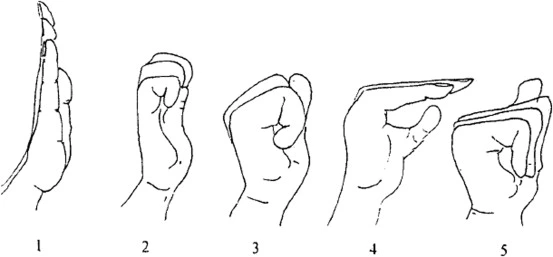
Among the activities most frequently advised to aid in recovery are tendon gliding exercises. The tendons must regain smooth motion after the thick fascia restricts movement. The objective of the physical therapy exercises is to activate 2 flexor tendons in the fingers. Gliding these flexor tendons facilitates free finger movement and the ability to grip firmly while minimizing swelling.
A tendon gliding example begins with the fingers being straightened first. Then, create a hook shape with the tips of your fingers, followed by the large knuckles, and form a straight fist while keeping the end joints straight. Finally, create a complete fist by bending all the joints. Additional tendon exercises will enhance flexibility and strength.
- Steroid injection.

Corticosteroids, potent anti-inflammatory drugs, can be injected into a painful nodule to reduce symptoms. However, there are individual differences in how effective a steroid injection is. Corticosteroids may relieve symptoms, but they are unlikely to prevent the disease from worsening; as a result, they constitute a treatment rather than a cure.
- Splinting.

Although numerous patients inquire about splints to avert the advancement of Dupuytren’s, there is no evidence that splinting can prevent the progression of a finger contracture. It is not beneficial to stretch the contracted finger forcefully; rather, this could lead to an injury of the finger or hand.
After surgery for Dupuytren’s contracture, splinting may be applied to preserve the surgical area; it remains unclear, however, whether the use of a splint lowers the chances of the healing wound developing contracture or tightening again.
- Collagenase injection.
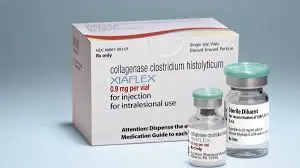
The collagen (a kind of protein) that comprises a Dupuytren’s cord differs from the collagen found in other structures of the hand (such as tendons, nerves, blood vessels, and bones). A medication that can be injected has been created to utilize these differences.
Collagenases are enzymes responsible for the decomposition of collagen. A specialized collagenase was developed to selectively break down the collagen in Dupuytren’s cords, preserving the integrity of the collagen in other vital structures of the hand.
To address Dupuytren contracture, your provider may administer collagenase injections into the nodules or cords. Collagenase is an enzyme that assists in loosening and decomposing the growths present on your fascia. Your provider will first administer an injection of collagenase into the cords or nodules directly. The next day, you will return, and they will numb your hand and extend your affected fingers to restore their normal range of motion.
This collagenase can aid in rupturing a Dupuytren’s cord, thereby enhancing the motion of the digit (thumb or finger), when injected into the cord correctly. The cord is not fully removed by the collagenase, but treatment can still reduce symptoms.
The treatment of Dupuytren’s with collagenase involves two steps.
- The medication is injected into the cord first. It is then permitted for the medicine to take effect over 2–3 days.
- At a later appointment, the doctor moves the finger in a controlled manner until the cord breaks.
This is a good non-operative alternative to surgery, but it should be noted that the recurrence (return) of the disease is higher with this treatment than with surgery. The injection of collagenase usually leads to reduced pain and swelling compared to major surgery. Therefore, it may be a viable option for patients with various medical problems who are not suitable candidates for surgery.
The injection may cause an allergic reaction or flexor tendon rupture, although this is rare. Other possible complications are identical to those associated with surgery: infection, damage to nerves or blood vessels, pain, and stiffness.
- Radiation Therapy
Your provider might refer you to a radiation expert to assist in treating Dupuytren contracture or to prevent your symptoms from worsening. Radiation therapy, which is a painless procedure, uses X-rays or other beams directed at the nodules or cords to soften them. Certain cancer types are treated with radiation therapy. However, Dupuytren contracture is not a form of cancer, and having it does not imply that you currently have (or will develop) cancer.
- Needle aponeurotomy.
Local anesthesia (an injection of a numbing medication) can often be used to perform needle aponeurotomy in the office. If conservative treatments haven’t led to symptom improvement after a few months, your provider may suggest a needle aponeurotomy. Sometimes, this procedure is referred to as a percutaneous needle fasciotomy. Your provider can perform needle aponeurotomy in their office as an outpatient procedure.
Your provider will use a local anesthetic to numb your hand, then make small punctures in the fascia of your hand with a needle to relieve tension and align your fingers.
During this procedure, a small needle is inserted into the Dupuytren’s cord to break it up. The needle is then moved with precision until it fully severs the cord. This does not eliminate the cord, but interrupting it facilitates enhanced finger movement. Similar to collagenase injection, this treatment may carry a higher risk of disease recurrence (return) compared to surgery. Although complications from needle aponeurotomy are uncommon, they can include infection, injury to nerves or blood vessels, pain, and stiffness.
Surgical Treatment
- Your doctor may suggest surgery if the contracture affects hand function. Surgery aims to lessen the contracture and enhance motion in the fingers affected.
- Dupuytren’s contracture has no known cure; the aim of surgery, however, is to reduce the limiting effect of the cords by disrupting or removing them to “set back the clock.” Unfortunately, the tissues that repair will have the same potential to develop cords in the future — but improvements in hand function can still be considerable.
The surgical procedures that are most frequently carried out for Dupuytren’s contracture include:
- Fasciotomy
- Needle fasciotomy
- Dermofasciectomy
- Partial palmar fasciectomy
Your physician will discuss with you which procedure is most suitable for your situation.
- Fasciotomy.
Your physician will cut open your palm and then separate the thickened cord(s) of tissue in this procedure. Even though the cord is not taken out, cutting it helps to reduce contracture and improve movement of the affected finger.
Fasciotomy is generally done with a local anesthetic that numbs only your hand, allowing you to remain awake. Your wound is often left open after the procedure, allowing for gradual healing. Wearing a splint will usually be necessary while you recover.
The fact that the tissue affected by the disease is not excised means that, in comparison with the partial palmar fasciectomy (which will be detailed below), this procedure may have a higher likelihood of contracture recurrence.
- Needle fasciotomy
To loosen and straighten your palm and finger, a needle is inserted at multiple points along them.
Local anesthetic (your hand is made numb) you can go home the same day recovery duration: as much as 2 weeks contracture has a higher chance of returning compared to surgery risks involve a cut reopening on your skin, pain, and numbness.
- Dermofasciectomy
Like a fasciectomy, but also involves the removal of an extra area of skin; removed skin is replaced with a graft taken from another area of the body.
- General anesthetic (you are unconscious) or local anesthetic (your hand is numbed)
- Two procedures are necessary: one to align the fingers and another to apply the skin graft. While contractures are less likely to recur compared to a standard fasciectomy, recovery may take longer. Risks include bleeding, numbness, and infection.
- Partial palmar fasciectomy.
Your physician will cut into the skin and then excise as much of the abnormal tissue and cord(s) as possible to align your finger(s). Various types of cuts can be employed in a fasciectomy; Nevertheless, “zig-zag” cuts are usually employed. The skin can heal without causing further contracture due to these incisions.
After a fasciectomy, some wounds will be left open to heal on their own gradually. In some instances, a skin graft will be necessary to assist in the healing of the wound. Your doctor will usually take healthy skin from another part of your body and use it to seal the wound for the skin graft. It may be necessary for you to wear a splint while you recover.
Fasciotomy is a less extensive (smaller) procedure than partial palmar fasciectomy. It usually entails increased wound care and physical therapy, an extended healing duration, and a greater effort from the patient throughout recovery. The advantage, however, lies in taking out as much of the diseased tissue as possible, which can aid in averting a recurrence (return) of the disease.
It is important to mention that, in certain cases of great severity, your physician might suggest the use of a Digit on the finger impacted by the condition before surgery. This instrument, which is usually used in surgery, slowly extends the finger and cord(s) over roughly 6 weeks. This can ease the execution of Dupuytren’s surgery, enhance its safety, and possibly improve its efficacy. It is possible to take out the device during the partial palmar fasciectomy.
Lifestyle and home remedies
For individuals with a mild case of Dupuytren contracture, hand protection can be achieved by:
- Preventing a strong hold on tools by adding thickness to the handles using pipe insulation or cushion tape.
- Wearing gloves that are heavily padded while performing tasks that involve a strong grip.
- Healthy Diet: A diet abundant in fresh produce can aid in lowering inflammation.
- Stop Smoking: As smoking can aggravate Dupuytren’s contracture, quitting is advantageous.
- Reduce Alcohol Use: Drinking too much alcohol may also have a detrimental effect on the condition.
- Consider Supplements: Vitamin E and magnesium might assist in lowering inflammation.
- Turmeric, zinc, and vitamin E: These dietary supplements might also offer advantages.
How long after treatment will it take for me to feel better?
The duration until you feel better varies depending on the treatment method used for your Dupuytren contracture:
- It can take months for conservative treatments to improve your symptoms.
- Your contracture should improve immediately with needle aponeurotomy.
- Your symptoms should improve after surgery; however, it may take as long as two months post-recovery for you to notice the full benefit. Post-operation, your hand will need time to heal. Additionally, you will require physical or occupational therapy for a minimum of several months to assist in restoring your hand’s strength and range of motion.
- Consult with your provider before returning to any of your usual activities during your recovery.
Prevalence
In the U.S., individuals of Northern European descent are more frequently affected by Dupuytren’s contracture. However, a study assessing more than 6.6 million people with Dupuytren’s disease revealed that the highest prevalence occurred in Africa, where this condition affected 17.2% of the population, compared to the global average of 8.2%.
Certain studies have suggested that your risk of developing Dupuytren’s contracture is higher if your job involves the use of vibrating tools. Having experienced hand trauma in the past raises the chances of developing this condition. According to one study, approximately 20% of patients had an injury-induced case of Dupuytren’s contracture. It appeared that hand and wrist injuries led to an earlier manifestation of the condition, although its overall progression was slower in these instances.
Risk factors
Risk factors associated with Dupuytren contracture include:
- Age. Most cases of Dupuytren contracture arise in people over the age of 50.
- Sex. The likelihood of men developing Dupuytren is significantly higher than that of women. Men might experience more severe symptoms that advance at a faster rate.
- Ancestry. Individuals with Northern European ancestry are more susceptible to the disease.
- Family history. There is often a familial link for Dupuytren contracture.
- Occupation. Certain research indicates a link between Dupuytren contracture and laborers who utilize vibrating instruments.
- Diabetes. The risk of developing Dupuytren contracture is higher for individuals with diabetes.
- Tobacco and alcohol use. The risk of Dupuytren contracture is increased by both tobacco smoking and alcohol consumption.
Complication.
There are risks linked to surgery for Dupuytren’s contracture, just as there are with any surgical procedure. The probability of complications rises with the following:
- The seriousness of the contracture, The number of contractures dealt with in one operation, and The existence of additional health issues. Your physician will go over each risk with you and will implement particular measures to prevent possible.
Potential complications and risks of Dupuytren’s surgery include:
- Pain
- Scarring
- Injury to nerves and/or blood vessels
- Wound infection
- Joint Stiffness
- Loss of feeling; stretching nerves that have been contracted for a long time may cause temporary loss of sensation
- Loss of viability (ability to live) of a finger/loss of a finger (rare)
Prognosis
Since it develops over months or years, it can be more helpful to consider Dupuytren contracture as a progression of symptoms you may or may not have yet, rather than as a disease with a specific timeframe.
In the future, it is possible for you to re-develop Dupuytren contracture after treatment. However, even if you do, your provider can address it using the same methods they employed during the initial instance.
Dupuytren contracture has a positive outlook. It is very manageable and progresses slowly, the Dupuytren contracture. Although a cure does not exist, various treatment options are available to reduce your symptoms. Moreover, it is always benign; thus, Dupuytren contracture is never a symptom or cause of cancer.
Summary
Generally speaking, Dupuytren’s disease can be treated with considerable success. Although many patients do not achieve a complete return to pre-disease digit motion, their symptoms are often significantly reduced after treatment, facilitating a return to effective hand function.
It is crucial to note that as Dupuytren progresses (declines), treatment becomes more difficult and outcomes decline. As a result, if you have Dupuytren’s or are worried that you might have it, consulting a hand surgeon sooner rather than later is advisable for the best possible outcome.
FAQs
What leads to Dupuytren’s contracture?
The origin of Dupuytren’s contracture is not known, but factors that increase the risk include getting older, having Scandinavian or Celtic ancestry, and having certain conditions like epilepsy, alcoholism, and diabetes. Options for treatment include surgical procedures and injections of corticosteroids into the palm.
Which treatment for Dupuytren’s contracture is the most effective?
Collagenase enzyme. By injecting a specific enzyme known as collagenase into the hardened lumps and cords, it is possible to soften and weaken them. During a second appointment in the following week, your hand is manipulated to break the cords and align your finger. This can diminish or even eradicate the contracture for multiple years.
What are the three phases of Dupuytren’s?
Many cytokines, such as interleukin-1, transforming growth factor beta-1 and beta-2, epidermal growth factor, platelet-derived growth factor, and connective tissue growth factor, are included. There are three phases of progression for Dupuytren contracture: proliferative, involution, and residual.
What is the latest therapy for Dupuytren’s?
Another method of treatment is to inject an enzyme known as collagenase clostridium histolyticum (collagenase) into the cord, which reduces its strength by degrading collagen; a few days post-injection, the weakened cord is adjusted to break it and align the contracted joint.
How does Type 3 Dupuytren’s disease manifest?
Stages of Dupuytren’s disease. Grade 1 manifests as a thickened nodule and a band within the palmar aponeurosis, which can advance to skin saddle, puckering, or pitting. A peritendinous band that restricts the extension of the affected finger characterizes grade 2. Grade 3 manifests as a flexion contracture.
How long does it take to recover from Dupuytren’s contract?
Your job determines how soon you can return to work. If your work can be done without using the hand, a return in 1 to 2 weeks may be possible. If your job involves making repeated finger motions, exerting pressure on your hand, or lifting objects, you might need to take a break from work for 6 to 12 weeks.
How do Dupuytren’s and arthritis differ from each other?
At the base of the thumb, arthritis frequently occurs, which can hinder individuals from performing everyday tasks such as twisting a doorknob or uncapping a bottle. The cause of Dupuytren’s contracture is the thickening of the connective tissue linking the skin on the palm side and the bones in the hand.
How successful is surgery for Dupuytren’s disease?
This technique aims to excise the diseased fascia that is affected macroscopically. Our study involved only regional selective fasciectomy, with 90% of patients achieving excellent or good results; except in the two cases that developed a recurrence.
Which nerve is implicated in the trigger finger?
The radial digital nerve of the thumb is said to be the most at-risk digital nerve during trigger finger release surgery, yet some studies have reported that digital nerve injury as a complication was not observed at all. Nonetheless, when it does happen, it leads to considerable morbidity.
Reference
- Dupuytren contracture – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/dupuytrens-contracture/symptoms-causes/syc-20371943
- Dupuytren’s Disease – Dupuytren’s contracture – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/dupuytrens-disease/
- Dupuytren contracture. (2025, February 8). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16941-dupuytrens-contracture
- Dupuytren’s contracture. (2024, April 29). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/dupuytrens-contracture
- Dupuytren’s Contracture: What is it? Symptoms, Causes & Treatment | The Hand Society. (n.d.). https://www.assh.org/handcare/condition/dupuytrens-contracture
- Dupuytren contracture – Diagnosis and treatment – Mayo Clinic. (n.d.). https://www.mayoclinic.org/diseases-conditions/dupuytrens-contracture/diagnosis-treatment/drc-20371949
- Knight, J. (2023, October 25). Dupuytren contracture: Signs, symptoms, & treatments. Hand and Wrist Institute. https://handandwristinstitute.com/dupuytren-contracture-signs-symptoms-treatments/