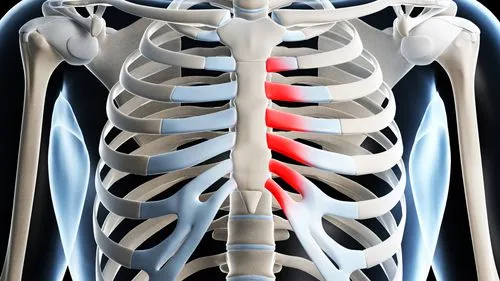
Costochondritis
What is a Costochondritis?
Costochondritis is the inflammation of the cartilage connecting the ribs to the breastbone (sternum), causing chest pain that may worsen with movement or deep breathing. It is often benign and self-limiting but can mimic heart-related pain. Causes may include strain, injury, or infections, and treatment typically involves pain relief with rest, anti-inflammatory medications, and heat or ice therapy.
Costochondritis can produce mild to severe chest pain. In mild cases, pushing on the area may simply cause a small tenderness or soreness in your chest. Deep breathing and specific movements can exacerbate more severe cases. Though some individuals may need treatment, the ailment usually goes away in a few weeks or months.
Definition
The self-limiting ailment known as costochondritis is characterized by excruciating, persistent inflammation of the anterior chest wall’s costochondral junctions of the ribs.
- In the absence of accompanying cardiopulmonary symptoms or risk factors, it is a clinical diagnosis and does not necessitate particular diagnostic testing.
- Tietze syndrome and costochondritis are frequently mistaken.
- The affected cartilage segments may extend out into the chest wall, and palpating the affected chondrosternal joints of the chest wall causes soreness and pain.
The upper ribs on the left side of the body are the most frequently affected by costochondritis. Although pain can occur where the cartilage joins to the rib, it is usually most severe where it attaches to the breastbone (sternum).
Other names for costochondritis include costosternal syndrome, cost sternal chondrodynia, and chest wall pain syndrome. Pain can occasionally be accompanied by swelling (Tietze syndrome).
It’s uncertain what causes costochondritis. The goal of treatment is to reduce pain while allowing the illness to heal itself, which may take weeks or longer.
Relevant Anatomy
The components of the thoracic wall are the:
- The sternum in front, 12 paired ribs and related costal cartilages in the back, and 12 thoracic vertebrae in the back.
- Bone and cartilage make up ribs, with cartilage acting as an elastic link between the sternum and the bony part of the rib.
- The ribs are divided into three categories based on how they adhere to the sternum: true, false, and floating ribs.
- The ribs 1–7 that directly articulate with the sternum through their costal cartilages are considered true ribs. Their articulation with the sternum is made possible by the sternocostal joints. An exception to this rule is the first rib, which has synarthrosis and can articulate with the clavicle only through the costoclavicular joint.
- Since their costal cartilages link the seventh costal cartilage through the costochondral joint, the false ribs (8,9,10) are the ribs that articulate with the sternum indirectly.
- The sternum does not articulate with the floating ribs (11,12) in any way (distal two ribs).
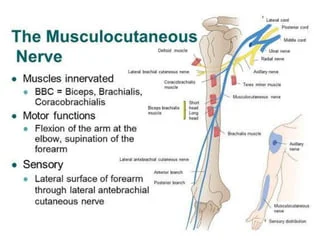
In addition to truncal motion, or movement of the upper extremities, the ribs move during breathing.
Epidemiology
Costochondritis epidemiology is not well understood.
- According to a short 1994 study, Hispanics and females were more likely to have costochondritis.
- 36 individuals (30%) out of 122 who arrived at the emergency room with chest pain that wasn’t caused by a fever, trauma, or cancer were diagnosed with costochondritis.
- Can have an impact on both adults and children. Thirteen percent of adolescents with chest pain had musculoskeletal reasons, with costochondritis accounting for fourteen percent of these cases, according to a study conducted in an outpatient adolescent clinic.
Signs and Symptoms
Which symptoms are present?
The upper and middle ribs on each side of the breastbone are frequently the site of chest pain in people with costochondritis. This pain may start slowly and get worse over time, or it may start quickly.
Other signs and symptoms may include:
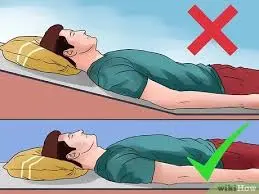
- The pain worsens when lying down.
- Pain that worsens with pressure on the chest, such as when wearing a seatbelt, and that gets worse when you cough or take heavy breaths.
- It’s crucial to remember that symptoms like radiating pain and stiffness in the chest might be signs of other illnesses, such as a heart attack. If you have severe, ongoing chest pain, get medical help right once.
- Occurs on the opposite side of your breastbone, which faces left.
- Impacts several ribs.
- May transfer to the arms and shoulders.
- It gets worse when you Deep breathing, cough, sneeze, or move your chest wall in any way.
If you have severe chest pain or difficulty breathing, you should see your doctor immediately. Anytime you experience unusual and incapacitating chest pain, you should always get emergency care right once. It may be a sign of a heart attack or something more serious.
The likelihood of problems is reduced by seeking treatment as soon as possible, particularly if your costochondritis is the result of an underlying condition.
Risk factors and causes
For the majority of persons, the cause of costochondritis is unknown. However, the following circumstances could lead to it:
- Chest injuries from falls or harsh impacts from auto accidents, as well as physical strain from heavy lifting and intense activity
- Some infections or respiratory diseases, such as tuberculosis, can lead to inflammation in the joints.
- The cause of costochondritis is mostly unknown. Costochondritis, on the other hand, may be linked to physical strain, such as intense coughing, illness, or trauma.
- Coughing.
According to some studies, women are more likely than males to develop costochondritis, particularly if they are athletes. Additionally, you can be more susceptible to this illness if you:
- Engage in activities that have a significant impact.
- Have allergies and are regularly exposed to irritants; recently experienced physical trauma or fall that impacted the chest area.
Diagnosis
Before diagnosing costochondritis, look into alternative explanations of chest pain including One excluding the diagnosis is costochondritis. It will be necessary to rule out respiratory and cardiac reasons. Radiating pain, dizziness, fever, shortness of breath, exertional chest pain, and productive cough are symptoms that could point to more serious and distinct causes of chest pain. An occult rib fracture should also be taken into consideration if there has been trauma. Following the exclusion of trauma and cardiac causes, the following results should be present in varying degrees.
Among the possible findings are:
- The patient will describe how the pain gets worse as they move and in particular postures. Additionally, when the sufferer inhales deeply, the pain usually gets worse.
- Although the intensity of the pain varies, it can be characterized as either dull or intense.
- Patients complain of pain and swelling in the upper costal cartilage adjacent to the costochondral junction that might develop gradually or quickly.
Palpation
- Palpation of mild to moderate pain is typically reproducible. There is frequent point tenderness where one or two ribs meet the sternum (pain from acute coronary syndrome can also be described as repeatable, which is a drawback of the usual physical exam findings).
- Symptoms can arise gradually and go away on their own in a few days, but they can also take years to go away. The symptoms could reappear at the same spot or at a different rib level even after they have subsided.
- The lateral ribs, costovertebral joints, and upper thoracic spine may all be hypermobile.
It is important to differentiate costochondritis from other, more severe causes of chest pain because it is typically benign and self-limiting.
- Three to six percent of adult patients with palpable chest pain and chest wall soreness have coronary artery disease.
- To make the diagnosis in children, adolescents, and young adults, a history and physical examination of the chest that records reproducible pain by palpating over the costal cartilage are typically sufficient.
- An ECG and maybe a chest radiograph should be performed on patients over 35, those with a history or risk of coronary artery disease, and any patient exhibiting cardiopulmonary symptoms.
- If clinically indicated by age or cardiac risk status, take into consideration additional testing to rule out cardiac reasons.
Examination
Individuals who have costochondritis will exhibit:
- Palpation of the affected area reveals reproducible chest pain, primarily in ribs 2 to 5.
- Exercise and slouching can be aggravating factors.
- It usually has a unilateral origin and frequently happens after a recent illness that includes coughing or vigorous exercise.
- On examination, the concomitant costotransverse and costovertebral restrictions might be related.
- Loss of normal spinal motion is linked to the pain in the chest.
- One digit should be used to palpate the clavicle, cervical, thoracic, and anterior, posterior, and lateral sides of the chest. When applied to the affected location, repeatable pain may indicate costochondritis, however, this cannot be confirmed.
- A joint is manually moved into its maximum end range of motion during motion palpation, and then it is tested with a mild springing movement. This joint movement endpoint serves as the foundation for identifying whether a joint movement is normal or pathological. A joint is deemed fixated or hypokinetic when motion palpation is diminished.
In patients with a high risk, cardiac reasons should be ruled out.
Diagnostic tests
Although there isn’t a test to identify costochondritis, your doctor will probably conduct several tests and ask you several questions to find out what’s causing your chest pain.
Laboratory tests
Costochondritis may usually be diagnosed without laboratory testing, but your doctor may order certain tests based on your medical history to rule out other conditions like pneumonia or coronary heart disease as the cause of your chest pain.
ECGs and X-rays
To ensure that nothing strange is wrong with your lungs, your doctor could advise you to have an X-ray. Your X-ray should appear normal if you have costochondritis.
Differential Diagnosis
The three main categories of intrathoracic and chest wall pain syndromes, as well as systemic illnesses that can induce chest wall pain, can all be used to differentiate between costochondritis.
Chronic pain
- When a patient presents with any kind of chest pain, consider acute coronary syndrome. Age, family history, and lifestyle variables such as tobacco use, preexisting diabetes, hypertension, and coronary artery disease are important differentiating risk factors for this condition.
- Patients with acute onset positional chest pain that gets better when they sit forward and gets worse when they lie supine should be evaluated for pericarditis. Pericarditis can be idiopathic, linked to an underlying connective tissue disease like lupus, or preceded by a recent respiratory infection or postcardiac surgery.
- Patients who have acute distress, shortness of oxygen, and chest pain should be evaluated for pneumothorax. Antecedent trauma, a history of pneumothorax, collagen vascular diseases such as Ehlers-Danlos syndrome, lung disease, and recent chest surgeries are risk factors.
- Patients who have fever, coughing, dyspnea, and chest pain should be evaluated for pneumonia. Immunosuppressive conditions such as diabetes, chronic kidney disease, dialysis reliance, immunosuppressive medication use, drug or alcohol abuse, and malnourishment are risk factors, as is senior age.
- Patients who have asymmetric limb blood pressure and chest pain that radiates to the arm or back may have an aortic dissection. Coronary artery disease and high blood pressure are risk factors. If a dissection is suspected based on the patient’s history, examination results, or the evidence of a dilated mediastinum on a chest x-ray, a chest computed tomography angiography (CTA) may be ordered.
- Consider pulmonary embolism in patients who experience dyspnea and chest pain. A history of cancer, recent travel, recent surgery or trauma, a history of deep vein thrombosis or pulmonary embolism, tobacco use, and the use of oral contraceptives are risk factors. When a pulmonary embolism is suspected in low-risk patients, the Wells score with a d-dimer may be used. For high-risk people, imaging studies such as a chest CTA or ventilation-perfusion scan are recommended.
- Patients experiencing severe or sudden chest pain should be evaluated for esophageal perforation. Acute prolonged vomiting, alcohol use problems, thoracic disorders like lung cancer, and recent gastrointestinal procedures like endoscopies are risk factors.
- Patients who experience chest pain that gets worse after eating or when lying down should be evaluated for gastroesophageal reflux disease. Hoarseness, Globus feeling, bloating, and regurgitation are other symptoms. Antacid consumption may result in an instant improvement in symptoms.
Chest Wall Disorder
Destructive costal cartilage lesions caused by an infection or tumor, or sternoclavicular, stern manubrial, or shoulder arthritis: These conditions may be accompanied by obvious edema, redness, or warmth, and they typically produce regional pain. When the xiphoid process is palpated, painful xiphoid syndrome results in localized pain.
- Herpes zoster: A skin examination may show vesicular lesions or erythema on the chest wall in a dermatomal pattern. Severe neuropathic pain is common.
- Slipping rib syndrome: This condition manifests as pain when palpating the lower chest wall or abdomen, as well as soreness along the costal border.
- Tietze’s syndrome: Usually affecting the region between the second and third ribs, Tietze’s syndrome frequently results in localized edema of the cost sternal, sternoclavicular, or costochondral joints.
Overuse myalgia and traumatic muscle pain are conditions caused by severe upper extremity exercise during work or athletic activities. Patients may have experienced trauma in the region in the past.
Systemic Disorders
- Patients with fibromyalgia may have chest pain, but they also frequently have persistent, chronic pain in several different parts of their bodies. Mood disorders, sleep disturbances, and fatigue may also be observed.
- Inflammation of the costovertebral, costotransverse, and thoracic apophyseal joints are symptoms of ankylosing spondylitis. On pelvic X-rays, patients may exhibit symptoms of fusion or inflammation in the sacroiliac joint, stiffness in the morning, and impaired spinal mobility.
- Psoriatic arthritis: Painful inflammation that may affect the chest. Typically, there are distinctive skin lesions and swelling in the extremity joints.
- The symptoms of synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome include sterile osteomyelitis, palmoplantar pustulosis, acne, peripheral or axial arthritis, and arthritis of the anterior chest wall.
- Systemic lupus erythematosus: Individuals with lupus may experience chest pain as a result of costochondritis, myocardial infarction, pulmonary embolism, fibromyalgia, or pleural or pericardial inflammation.
Patients with chest pain and nonspecific symptoms, such as arm and leg pain or other unusual sensations, disorientation, a sense of impending doom, palpitations, and dyspnea, may be diagnosed with panic disorder. It is possible to elicit a history of anxiety. There may or may not be a precipitating event for the syndrome.
Costochondritis can be differentiated from these illnesses with a thorough clinical evaluation and pertinent diagnostic testing. Before starting treatment, life-threatening conditions must be ruled out.
The majority of costochondritis cases are managed with over-the-counter drugs. Your doctor would most likely suggest nonsteroidal anti-inflammatory medicines (NSAIDs) like naproxen (Aleve) or ibuprofen (Advil) if your pain is mild to severe.
Over time, costochondritis typically resolves on its own. A few weeks to many months may pass during that time. Ibuprofen and other painkillers that reduce inflammation might be suggested to relieve the pain. If the intense pain continues to not go away with time, you may be administered an injection of steroid to help reduce inflammation or a topical anesthetic to soothe the agony.
Treatment of Costochondritis
Among the aspects of management are:
- Refer patients for outpatient follow-up if they have severe or refractory costochondritis. The treatment for refractory costochondritis may involve physical therapy.
- Ice, acupuncture, manual therapy, exercise, and other drugs like sulfasalazine are examples of alternative treatments that may also be beneficial in the long run for managing costochondritis.
- Rest, physical rehabilitation, and hot or cold therapy with ice and a heating pad
- Usually, costochondritis improves in a few weeks. It is frequently described as a self-limiting illness. This implies that it can improve on its own over time. Pain relievers and self-help techniques can help you control your symptoms.
- Any action that puts stress on your chest, such as intense exercise or repeated motions, might exacerbate costochondritis.
- You should adjust any movement that exacerbates your chest pain until the cartilage and rib inflammation have subsided.
Here are a few instances of changed activities:
- Taking regular pauses.
- Holding items close to your body when lifting them, shifting positions frequently. While sitting or lying down, and cuddling with a pillow while coughing.
Medical Treatment
Pain can be lessened by doing the following:
- Strength of prescription drugs NSAIDs, oral steroids, or steroid injections entailed transcutaneous electrical nerve stimulation (TENS), which uses a tiny, battery-operated device to apply a modest electric current to the affected area.
- Local steroid injections into the tendon sheath, joint, or surrounding nerve increase mobility by reducing pain, edema, and inflammation.
- Either oral or topical analgesics.
- Painkillers can make it easier for you to move, which will aid in the healing process.
Physical therapy treatment
- Education: Explain the condition to the patient to reassure them.
- Minimizing symptoms-inducing activities (e.g., lowering the frequency or intensity of work or exercise activities)
- A course of pain-relieving trigger point therapy, such as cross-fiber friction massage
- Conservative pain management techniques include applying heat or cold treatments.
- Retrain good posture in functional positions with postural exercises (neuro-muscular control). The main goal of functional training is to maintain proper posture during regular tasks by engaging the appropriate muscles at the appropriate times. To guarantee proper technique and muscle engagement, simple exercises like sitting to stand, walking up stairs, and proper standing posture must be addressed.

To reduce strain on inflammatory rib cartilage, physical therapy for costochondritis focuses on improving movement, reducing inflammation, and assisting you in managing your pain. Working with a musculoskeletal physical therapist, who specializes in treating musculoskeletal disorders, is beneficial for the majority of persons with costochondritis.
You can use several modalities and movements to enhance your movement. These could consist of:
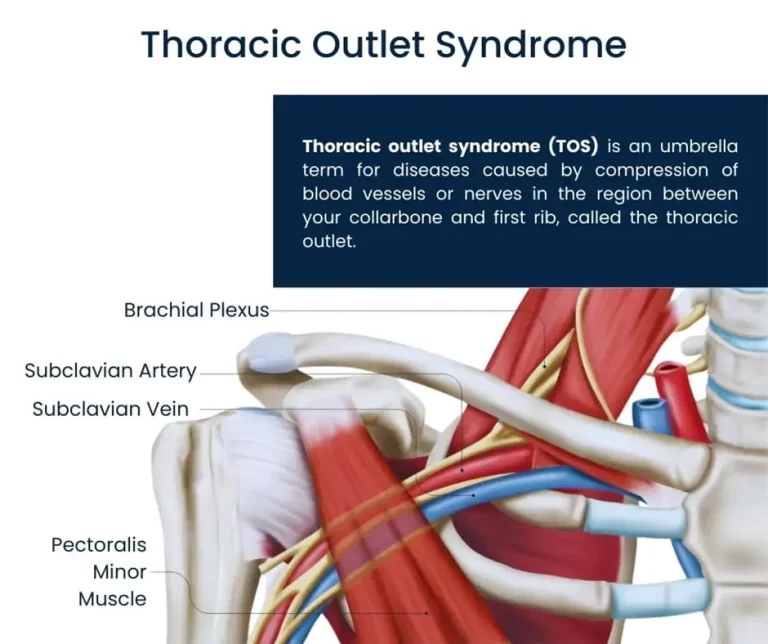
- Strengthen the way your ribs slide up and down after regular breathing with these rib mobilizations.
- Using spinal joint mobilizations can help your thoracic outlet spinal joints move and slide more smoothly.
- Stretching and range-of-motion activities might relieve the strain on irritated rib cartilage and enhance mobility.
- Exercises for postural strengthening to help you stay in the right positions and relieve pressure on your rib cartilage.
- Breathing techniques that enhance the movement of your ribs during deep breathing
- Pain and inflammation can be reduced with the use of additional therapies. These could include ice to reduce pain and edema around inflammatory tissues and heat to increase circulation. Because the affected cartilage is near the heart, other popular physical therapy procedures like ultrasonic or electrical stimulation are not used. It is not advised to do these treatments close to your heart structures.
Participating actively in your treatment is essential. Your therapist will probably recommend exercises to improve the movement of your thorax (chest) and
Exercises
- The goal of costochondritis exercises is to increase the general mobility of the ribs and chest wall. This can enhance the movement of your thorax and ribs and lessen pain. Inflamed cartilage might be relieved by postural exercises.
- Consult your healthcare professional to be sure exercise is acceptable for you before beginning any costochondritis exercise regimen.
Pectoral Stretching

Your pectoral or chest muscles will become more flexible if you perform the pectoral corner stretch. To carry out the stretch:
- Position yourself two feet from the wall, facing a corner.
- With the forearms resting upon the wall on either side of the corner, raise both of your arms. Make sure your elbows, hands, and forearms touch the wall.
- Stretch the muscles at the highest point of your chest by slowly leaning into the corner.
- After holding the contraction for 15 to 30 seconds, let go.
- Three to five times, repeat the stretch.
Doorway Pectoral Stretching
Additionally, you can use a doorway opening to stretch your pecs. To carry out this stretch:
- Place your forearms and elbows up against the doorjamb on the opposite side of you as you stand in a doorway.
- Stretch the muscles at the front of your chest by slowly bending forward while maintaining your elbows against the doorjamb.
- Hold
- Then Relax.
- Do this three or five times.
Scapular Squeeze
Squeezing your scapula can help you manage your thoracic muscles and posture. To carry out this exercise:
- Press both of your shoulders together softly in the back while seated comfortably in a chair.
- Hold the pose for three seconds while feigning that you are attempting to squeeze a pencil through your shoulder blades.
- Return to the starting position after releasing slowly.
- Ten to fifteen times, repeat.
- With a resistance band, the top of the scapula squeeze exercise may be more difficult:
- Hold either end of the band as you loop it around a sturdy object.
- Pinch your scapulae together and bend your elbows back like you’re rowing a boat.
- Then let go gradually.
- Ten to fifteen times, repeat the workout.
Stretching the Chest with a Stability Ball
Using a stability ball is another excellent method to stretch your pectorals and chest muscles and loosen up your chest wall. To perform this stretch:
- Over a 25-inch stability ball, lie on your back.
- Raise both arms in front of you, then slowly spread them apart as though you were going to embrace someone.
- As you open your arms, let your back relax and let your arms fall toward the floor, exposing your chest.
- As you perform the exercise, you should get a mild tugging feeling in your chest.
- Return your arms to the midline after holding the stretch for 15 to 30 seconds.
- Do this three or five times.
Stop exercising and consult your physical therapist if you get persistent pain in your ribs or chest. You can often modify your exercises to make them more pleasant.
Home care Advice
Here are some costochondritis home remedies that are beneficial in costochondritis treatment-
- Rest
- Ice or heat
- Gentle stretching costochondritis exercises like chest stretch, shoulder roll, and neck stretch
- Epsom salts in a warm bath
- Maintain good posture
- Avoid smoking
- Manage stress
- Get enough sleep
Lifestyle Changes
If you have chronic or persistent costochondritis, your doctor may advise you to adjust your lifestyle permanently. Certain forms of activity, such as weightlifting and rowing, can make this disease worse. Negative effects can also result from manual labor.
Prevention
Learning to prevent future issues with your illness is a crucial part of any successful physical therapy program. Some ways to prevent costochondritis include:
- Developing and preserving proper posture.
- Stretching frequently, a few times a week, and strengthening the muscles in your abdomen and back.
- Exercising regularly.
- Following your at-home stretching, breathing, and postural exercise regimen may help manage your costochondritis symptoms if you start to notice them reoccurring.
Complication
What are the complications of costochondritis?
- Usually, there are no complications from costochondritis. It might not recur very often or the symptoms might not get better. Your doctor could recommend a rheumatologist—a specialist in conditions affecting the joints, muscles, and bones—if this occurs.
- If your symptoms don’t get better, your rheumatologist might suggest corticosteroid injections.
Conclusion
- Inflammation is the source of costochondritis, which usually manifests as chest pain that worsens with pressure or specific movements. Usually, this situation doesn’t last. Costochondritis often resolves on its own.
- After a few days, mild cases of costochondritis could go away. Most cases don’t persist for more than a year, while chronic cases might linger for weeks or more.
- Use caution when lifting and carrying large objects to reduce your risk of acquiring chronic costochondritis. If at all feasible, try to limit your physical labor and high-impact exercise.
- If you have chest pain while engaging in any of these activities, get medical help right once.
- Labs, an ECG, and a chest x-ray should all be within normal ranges, and a scan or bone scintigraphy and a physical examination of the affected costal cartilage are used to confirm the diagnosis. Conservative management is the usual course of treatment for costochondritis, which is typically symptomatic. If the condition does not improve, physiotherapy is frequently prescribed.
FAQs
Which foods shield against costochondritis?
The signs, causes, cost, treatment, and side effects of costochondritis…
Dietary anti-inflammatory: Inflammation is the primary cause of pain areas associated with costochondritis, and it can be decreased by eating a diet rich in anti-inflammatory vegetables and herbs. Green leafy vegetables, ginger, turmeric, cherries, and so forth may be included in the diet.
How can someone who has costochondritis sleep?
To reduce rib pain, use an ice pack or heating pad on the affected area, stretch your chest gently, and take over-the-counter pain medicines. Which sleeping posture is best for those with costochondritis? Do not lie on the side of your chest that hurts. For people with costochondritis, lying on your back is the ideal position.
Which type of exercise is beneficial for those with costochondritis?
Stretch of the doorway Facing an open doorway, stand. Bend your elbows to a 90-degree angle and raise your hands to the sides. To stretch your chest muscles, bend backward through the open doorway while keeping your elbow at the level of your shoulder and your forearm resting against the wall. Before you relax, hold the stretch for 30 to 60 seconds.
What is costochondritis first aid?
Applying a moist compress or warming pad to your chest at a low temperature may be beneficial. Switching heat and ice is another option. Apply a cold pack of ice to the area for ten to twenty minutes at a time.
Does costochondritis benefit from drinking water?
Decreased Lubrication: Sustaining the lubrication of cartilage and joints requires enough hydration. Dehydration may aggravate the inflammation linked to costochondritis by reducing lubrication and increasing friction between the ribs and the sternum.
How should costochondritis be treated?
The most popular treatment for costochondritis is to rest your ribs and chest. The best treatment for costochondritis is to give your irritated costochondral joints time to heal. Pain can be managed using over-the-counter (OTC) medications such as acetaminophen or NSAIDs (nonsteroidal anti-inflammatory drugs).
Costochondritis is caused by what deficiency?
Children with hypertrophy costochondral junctions and adults with osteocalcin who have sternal pain are known to be affected by vitamin D deficiency. We suggest that the chest pain linked to costochondritis may be caused by a vitamin D deficiency.
Can someone with costochondritis benefit from massage therapy?
Pain may be lessened with neuromuscular massage because it may enhance blood flow, reduce tissue stiffness, and moderate inflammation. It should be mentioned that while some cases of costochondritis are quite chronic, others are transient and may resolve with time.
Reference
- Stoltzfus, S. (2023, February 1). What is costochondritis? Healthline. https://www.healthline.com/health/costochondritis#takeaway
- Costochondritis – Symptoms & causes – Mayo Clinic. (2022, May 11). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/costochondritis/symptoms-causes/syc-20371175
- Website, N. (2022, August 1). Costochondritis. Nhs.uk. https://www.nhs.uk/conditions/costochondritis/#:~:text=Costochondritis%20is%20inflammation%20where%20your,on%20its%20own%20over%20time.
- NHS inform. (2025, February 6). Costochondritis | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints/chest-and-rib-problems-and-conditions/costochondritis/#:~:text=About%20costochondritis,Diagnosing%20costochondritis
- Pt, B. S. (2024, May 2). Costochondritis and what to expect from physical therapy. Verywell Health. https://www.verywellhealth.com/costochondritis-physical-therapy-exercises-5199284#:~:text=Common%20Assessment%20Tests,Pulmonary%20function%20and%20breathing%20assessment