Chondromalacia Patella (CMP)
What is a Chondromalacia Patella?
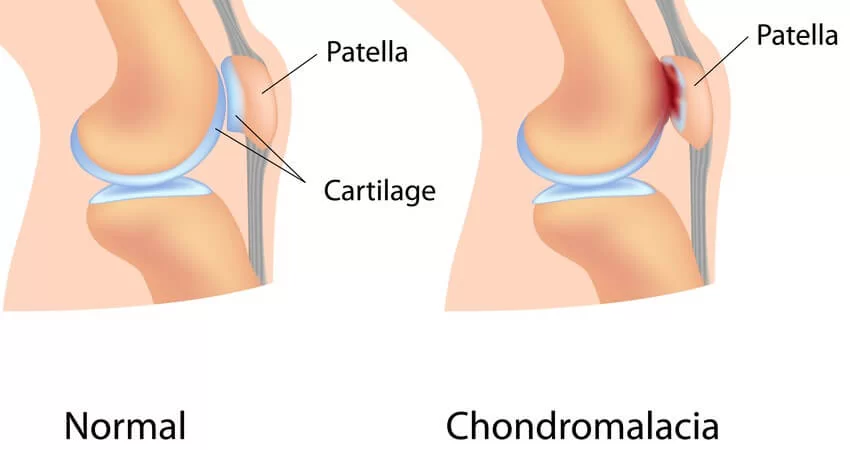
Chondromalacia patella (CMP) is a disorder characterized by the weakening and deterioration of the cartilage beneath the patella (kneecap). This cartilage normally allows smooth movement of the knee joint, but when it deteriorates, it can cause pain, discomfort, and a grinding sensation during movement. Often referred to as “runner’s knee,” Chondromalacia Patella is common in young athletes, but it can also affect older adults, especially those with arthritis.
The condition is typically aggravated by activities that place stress on the knee, such as climbing stairs, squatting, or sitting for prolonged periods. Early diagnosis and appropriate management can help alleviate symptoms and prevent further cartilage damage.
The hyaline cartilage below the patella is softening, swelling, fraying, and eroding, and the underlying bone is sclerosis as a result of degenerative changes in the articular cartilage of the posterior surface of the patella.
Anatomy related to Chondromalacia Patella
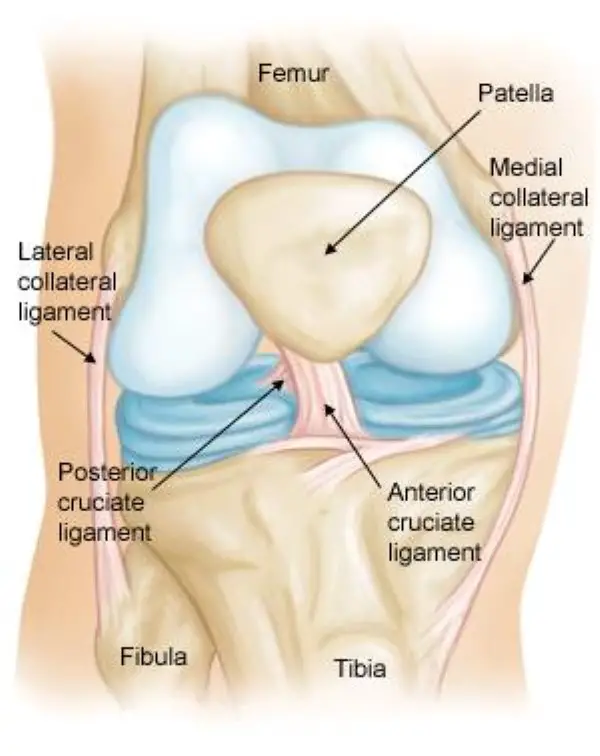
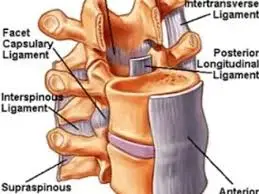
- The femur, tibia, fibula, and patella are the four main bones that make up the knee joint.
- For effective knee joint mobility, the patella must be able to slide along the femoral groove, which is made possible by articular cartilage on the underside of the patella.
- The articular cartilage’s nutrition may be negatively impacted by excessive and persistent twisting forces on the lateral side of the knee, particularly in the medial and central regions of the patella, where degenerative change is more likely to develop.
- During knee extension, these muscles particularly the VL on the lateral side and the VMO on the medial side act as active stabilizers. Its job is to maintain the patella’s center of gravity within the trochlea.
- The quadriceps have an impact on the knee’s passive components in addition to the patella position. The majority of the lateral retinaculum originates from the iliotibial band (ITB), and these passive structures are stronger and more extensive on the lateral side than the medial side.
- Excessive lateral tracking and/or lateral patellar tilt may result from an overly taut ITB. The ITB is a non-contractile structure, therefore this could be the result of the tensor fasciae lata being tight.
- Other significant anatomical structures:
- The disorder known as femoral anteversion, or medial torsion of the femur, affects how the bones align at the knee. This may result in femur misalignment with respect to the patella and tibia, which could cause overuse problems to the knee.
- It represents the geometric relationship between the pelvis, tibia, patella, and femur.
- The Q-angle will rise in response to increasing hip adduction and/or internal rotation, which will also raise the lower extremity’s relative valgus. The contact pressure on the lateral side of the patellofemoral joint—which is also raised by the tibia’s external rotation—will rise as a result of the higher Q-angle and valgus.
Epidemiology
- Young individuals who are physically active and participate in running activities or who work in jobs that require frequent stair climbing and/or kneeling are more likely to develop chondromalacia.
Causes of Chondromalacia patella
The articular cartilage may also become softer due to instability or maltracking of the patella.
Principal causes of malalignment of the patella:
- Q-angle: One of the most important causes of patellar malalignment is an aberrant Q-angle. For men, a normal Q-angle is 14°, and for women, it is 17°.
- Tightness in the Rectus femoris muscle: impairs patellar mobility during knee flexion.
- Tensa Fascia late; influences the ITB Hamstrings: Tight hamstrings during running cause the knee to flex more, which increases the dorsiflexion of the ankle. The talocrural joint has compensatory pronation as a result.
- Gastrocnemius: a tight muscle will causes the subtalar joint to compensate by pronating.
- Excessive pronation: The patella will become misaligned as a result of this internal rotation.
- A condition known as patella alta occurs when the patella is positioned unusually superior. When the patellar tendon’s length is 20% longer than the patella’s height, it is present.
- It’s critical to maintain a muscular balance between the VM and VL. Degenerative disease may result from the patella being dragged too far laterally in areas where VM is weaker, increasing contact with the condylus lateralis.
- Trauma can result in degenerative changes in the articular cartilage, such as instability brought on by prior trauma or overuse during the healing process.
- Microtrauma repetition and inflammatory disorders
- Postural distortion: results in the patella being misplaced or dislocated within the trochlear groove.
- Patellofemoral pain syndrome prevalence is related to hip posture and strength. Exercises for hip stability and strengthening may therefore be helpful in the treatment of patellofemoral pain syndrome.
Stages of Chondromalacia patella
Oedema may also result from this, which is linked to the cartilage’s increasing thickness. A more uneven surface with localized thinning that can expand to reveal the subchondral bone will be present in the later stages.
- Stage 1: articular cartilage swells and softens as a result of broken vertical collagenous fibers. Upon arthroscopy, the cartilage seems spongy.
- Stage 2: the separation of the deep and superficial cartilaginous layers causes blisters to form in the articular cartilage.
- Stage 3: less than 50% of the patellar articular surface is affected by fissures, ulcerations, fragmentation, and fibrillation of cartilage that extend to the subchondral bone.
- Stage 4: sclerosis and erosions of the subchondral bone, together with crater development and eburnation of the exposed subchondral bone, exposing more than 50% of the patellar articular surface. At this stage, osteophyte formation also takes place.
Rather, it is a pathological or surgical finding that denotes areas of divergent loading or articular cartilage trauma.
Clinical features of Chondromalacia patella
- The primary sign of chondromalacia patellae is anterior knee pain, which is made worse by routine movements including running, stair climbing, squatting, kneeling, and getting up from a sitting to a standing posture that puts stress on the patellofemoral joint.
- discomfort coming from the patella’s back side. The pain is taken on by the patella pressing against the femoral condyle. Pain frequently results in handicaps that limit short-term engagement in daily tasks and physical activity.
- pain when the patella is palpated beneath its medial or lateral border; crepitation felt during movement; mild edema; and a high Q-angle.
Risk Factors of Chondromalacia Patella:
There are numerous variables that could make you more susceptible to chondromalacia patellae.
- Age: Young adults and adolescents are more susceptible to this disease. Rapid bone and muscle development occurs during growth spurts, which may be a factor in temporary muscular imbalances.
- Sex: Both improper knee posture and increased lateral (side) pressure on the kneecap may result from this.
- Flat feet: Compared to people with higher arches, people with flat feet may experience greater strain on their knee joints.
- Previous injury
- High activity level: You run a higher chance of developing knee issues if you exercise frequently or have a high activity level that puts strain on your knee joints.
- Arthritis: Another disorder that can cause inflammation in the joint and tissue is arthritis, which can also manifest as a runner’s knee. A kneecap that is inflamed may not operate as intended.
Differential Diagnosis
- Chondromalacia patellae
- Osteochondritis desiccant
- Patellofemoral osteoarthritis
- Patellofemoral pain syndrome
- Lateral patellar compression syndrome
- Plica syndrome
- Quadriceps tendonitis/tendinopathy
- Patellar tendonitis/ tendinopathy
- Saphenous neuroma
- Postoperative neuroma
- Patellar fat pad inflammation
- Hoffa disease
- Patella Alta
- Patella Baja
- Patella instability
- Bi-partite patella
Diagnosis of Chondromalacia patella
Examination
A knee examination consists of four components: mobility, feel, X-ray, and observation.
Effusion test:
- Patellar tap test: The patient has one leg outstretched while they are supine.
On the other hand, the therapist applies pressure to the medial and lateral recesses, pressing the fluid beneath the patella while preserving the pressure on the suprapatellar pouch.
Since the test may yield a false positive, we must always compare results from both sides. - Patellar grind test or Clarke’s sign.
- Compression test.
- Extension-resistance test.
- The critical test: involves the patient sitting up straight and contracting their quadriceps isometrically at five various angles (0°, 30°, 60°, 90°, and 120°) while rotating their femur externally and holding the contractions for ten seconds. The leg is extended to its maximum length if pain is experienced. Keep this glide going as you repeat the isometric contractions. There is a good possibility of a successful outcome if this lessens the discomfort and originates from the patellofemoral region.
- Feel: If the patella is crushed against the femur in either a vertical or horizontal direction when the knee is fully extended, pain and crepitus will be experienced.
Generally, a sharp ache under the patella will occur when you resist a static quadriceps contraction. Both knees may exhibit this, with the affected side experiencing more severe symptoms. - X-ray: Except in the most severe cases, there is no discernible radiological alteration. The patellofemoral joint space narrows and osteoarthritic abnormalities start to show in the latter stages.
Treatment:
Medical Treatment of Chondromalacia patella:
- Education and exercise are two crucial components of a therapeutic plan. Education aids in the patient’s comprehension of the ailment and the best course of action for managing it.
- There are several potential surgical techniques in case the conservative methods prove ineffective.
- Chondrectomy is a term that can be shaved. As part of this procedure, the damaged cartilage is shaved away to reveal the healthy cartilage underlying.
- Another technique that’s widely utilized to repair damaged cartilage is drilling. Perforating tiny holes through the injured cartilage may be more effective in treating more localized tissue deterioration. This makes it easier for healthy tissue to develop through the gaps left by the layers below.
- Complete palate excision: This is the most invasive surgical procedure. The quadriceps will weaken as a result of this approach, which is only employed when no other treatments are helpful.
- There are two other treatments that might work.
- Replacement of the injured cartilage: Although the opposing articular surface will eventually wear down, the early outcomes have been positive.
- implantation of autologous chondrocytes beneath a tibial periosteal patch.
- Chondromalacia patellae cannot be cured by merely removing the cartilage. There are several treatments to help manage the biomechanical weaknesses that need to be addressed.
- The medial capsule (MC) becomes taut: Pulling the patella back into the proper position will tighten the MC if it is slack.
- Lateral release: The patella will be pulled laterally by an extremely tight lateral capsule. The patella can properly track into the femoral groove after the lateral patellar retinaculum is released.
- The tibial tubercle’s medial shift: The quadriceps can pull the patella more directly if the tendon’s insertion is moved medially at the tibial tubercle. Additionally, it lessens the amount of patellar wear on the underside.
- partial patellar excision
- While opinions on how to treat chondromalacia vary, non-surgical methods are generally seen to be the most effective.
Physical therapy Treatment of Chondromalacia patella
Pain-relieving modality
- Transcutaneous electrical nerve stimulation, or TENS, is an electrical technique that reduces pain by modulating it.TENS shuts down the spinal cord’s anterior grey horn gate mechanism.
- Short wave diathermy, or SWD for short, is a deep heating technique that employs heat to reduce pain, enhance blood flow to specific muscles, and eliminate waste.
- IFC: Interferential current therapy generates a low-frequency effect at the targeted tissue, enhances blood flow, decreases edema, stimulates the endogenous opioid system, and blocks the transmission of pain signals. It also eliminates waste products.
- Cold therapy: a method of reducing pain and inflammation Ice massage: Apply ice to the irritated area to reduce inflammation. To prevent frostbite, use ice in a paper or Styrofoam cup that has been pulled away for five to seven minutes.
- Initially, the knee is immobilized in a pop cylinder cast if it is too painful.
- The training regimen consists of passive or active knee swinging that is relaxed to preserve a broad range of motion and single-leg exercises supported by a mild isometric quadriceps contraction to increase strong hip ankle-foot movements.
- Tensor fascia lata, gastrocnemius, hamstring, and rectus femoris muscles should all be stretched.
- strengthening activities for the oblique vastus medialis muscle.
Patellar taping:

Taping the patella to change its movement may offer some temporary comfort, but the data is conflicting.
Knee braces:
- Supporting the patella and knee joint with bracing is an additional method of pain relief, but it will also change patella tracking and lessen the quadriceps’ active activity.
- In the short term, bracing may be helpful in providing patients with pain relief and support to assist them avoid antalgic motions and return as close to normal gait as feasible.
- When patients with chondromalacia patellae follow physical treatment, wearing a patellar realignment brace has a synergistic impact.
Foot orthoses:
- Another alternative for pain management is to wear foot orthoses, but only if it is determined that the knee discomfort is caused by abnormalities in the lower limb mechanics. These abnormalities may be caused by:
- Inadequate control over-pronation, excessive internal rotation of the lower limbs when carrying weight
- An elevated Q-angle
Foam Roller:
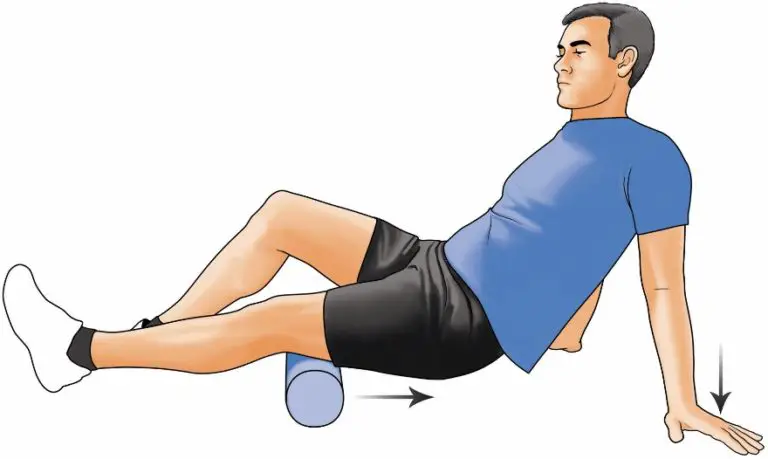
- One helpful technique for releasing tight muscles and lowering pressure over the patella is to use a foam roller.
- Hamstring muscle exercise using a foam roller
- Glute muscle training with foam rollers
- Tensor fascia lata and iliotibial band exercises with foam rollers.
Prognosis
- Knee pain associated with chondromalacia patella often resolves entirely in affected individuals.
- Depending on the situation, recovery could take a month or several years. Teenagers often heal for a long time because their bones are still growing and their symptoms normally get better with age.
Complications
- Patients with chondromalacia patella may have secondary issues from bracing a reaction in which the skin occasionally responds to the brace material or from using NSAIDs (e.g., gastrointestinal complaints).
- Therapeutic exercises almost seldom make problems worse.
- In the event that the activity is linked to worsening symptoms, the patient, the physician, and the therapist should work together to modify it. This could entail adjusting the exercise’s duration, frequency, or intensity or, if necessary, temporarily ceasing it altogether.
Patient Education
Patient education emphasizes taking medications as directed, recovering from surgery, performing therapeutic exercises, and minimizing pain when engaging in any activity or movement.
Conclusion
- The prognosis is determined by the severity and response to therapy. Conservative methods, such as physical therapy, rest, and modifying one’s activities, are frequently successful.
- In some cases, surgical options may be investigated. For a customized plan, speaking with a healthcare professional is essential.
FAQs
With chondromalacia patella, how should one sit?
Try the following to lessen chondromalacia symptoms and hasten your recovery: Raising the injured knee: While seated, elevate your leg by placing a pillow beneath the leg that is injured.
What is chondromalacia patella stage 1?
Grade 1, the least severe, denotes some cartilage deterioration. Grade 2 is characterized by softness and irregular surface features, which most likely signal the onset of tissue deterioration. In Grade 3, the tissue is actively deteriorating and the cartilage is thinned.
How may chondromalacia be naturally healed?
Low-impact exercises like swimming can assist an athlete in maintaining their fitness during this period; jogging and other knee-stressing sports should be avoided.
Does chondromalacia patella require surgery?
Many times, the issue becomes worse with activity and gets better with rest since the kneecap has been misaligned for the entirety of the patient’s life. A lot of folks choose to have this issue surgically fixed. With arthroscopic surgery, this issue can be surgically corrected really easily.
Is chondromalacia ever completely gone?
However, one may be able to make it become asymptomatic with the use of an exercise regimen, injections, weight loss, and/or avoiding behaviors that exacerbate the condition.
Is there a complete recovery from chondromalacia?
Because articular cartilage heals slowly, chondromalacia usually lasts a lifetime. Nonsurgical therapy, however, can often eliminate knee stiffness within a few months.
Is it beneficial for chondromalacia patella to walk?
Low-impact workouts, such as walking on flat ground or swimming, are the best.
What is the most efficient method for chondromalacia to heal?
Non-operative therapy is the standard of care for this problem. You may need to see a physical therapist for four to six weeks in order to treat your chondromalacia patella. After that, you will likely need to spend many more months performing strengthening and stretching exercises at home. The initial step is to control the soreness and inflammation.
At what age is patella chondromalacia common?
Between the ages of 15 and 35, patients with chondromalacia patella are frequently young and enjoy active lives. The symptoms of the illness can be extremely crippling and include recurrent knee effusion, knee instability, and crepitus.
Does chondromalacia have a non-surgical cure?
For chondromalacia, nonsteroidal anti-inflammatory drugs (NSAIDs) and rest are the most often used over-the-counter pain medications. Surgery is indicated less commonly; physical treatment is advised occasionally.
Is patella chondromalacia serious?
Chondromalacia patella is not usually a significant ailment. In reality, most people can manage it with rest, elevation, ice, and stretching. However, in some people, the illness can worsen to the point that over-the-counter painkillers and complementary home remedies are insufficient to relieve symptoms.
References
- Dhameliya, N. (2024, May 30). Chondromalacia Patellae: Physical therapy Management. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/chondromalacia-patella/
- Prajapati, D. (2023, May 28). chondromalacia patella physical therapy protocol Archives – Samarpan Physiotherapy Clinic. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/tag/chondromalacia-patella-physical-therapy-protocol/
- Physiotherapist, B. (2023, December 13). Chondromalacia Patella: Causes, Symptoms, Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/chondromalacia-patella-and-physiotherapy-management/
- Dhameliya, N. (2024b, September 13). Chondromalacia Patellae (CMP). Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/chondromalacia-patellae/