Brachial Plexus Injury
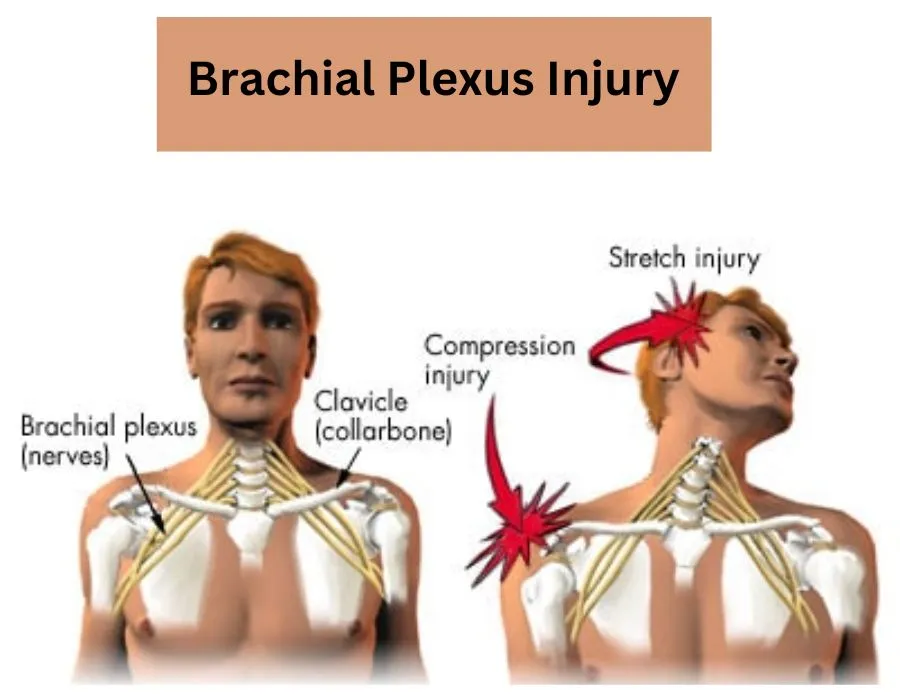
Brachial plexus injury refers to damage to the network of nerves that runs from the spinal cord to the hand, arm, and shoulder. The brachial plexus is the network of nerves that runs from the spinal cord to the hand, arm, and shoulder. The brachial plexus is harmed when these nerves are strained, compressed, or in the worst cases, torn apart or separated from the spinal cord.
Brachial plexus injuries, often known as stingers or burners, are common in contact sports such as football. In neonates, birth trauma can occasionally result in brachial plexus injury. Two additional conditions that can affect the brachial plexus are tumors and inflammation.
Motorcycle or car accidents typically cause the most severe brachial plexus injuries. Even though severe brachial plexus injuries may cause paralysis, the arm may be able to function again after surgery.
What is Brachial Plexus Injury?
- Brachial plexus injury is the term used to describe damage to the network of nerves that extends from the spinal cord to the shoulder, arm, and hand. From its placement near the top of the spine, this network spreads towards the armpit. These nerves are suddenly destroyed after a brachial plexus injury, which can cause pain, weakness, or loss of feeling in your hand, arm, or shoulder in addition to limiting movement.
- The brachial plexus begins in your neck, crosses your upper chest, and finishes beneath your armpit. This network of nerves is often harmed when you pull or push hard on your arm, or when your head and neck are dragged away from your shoulder.
- Brachial plexus injuries can result in discomfort, weakness, and numbness in the arm and hand and are usually caused by trauma to the neck.
- Brachial plexus injuries that are not serious usually heal well. 90%–100% of the normal function of the arms is recovered in many cases of mild brachial plexus injuries. In cases of more severe brachial plexus injuries, function is frequently restored with surgery.
- Brachial plexus injuries can occur in the uterus or during childbirth. Neonatal brachial plexus palsy is the name given to this injury (NBPP).
- You should contact your healthcare physician to determine the cause of your symptoms if you have had an injury to your neck or shoulder and are unable to move or feel your hand or arm.
What is Brachial Plexus? Its Structure and Function
The brachial plexus is a network of nerves that connects the spinal cord to the hand, arm, and shoulder, carrying messages. This network starts near the top of the spine and extends towards the armpit.
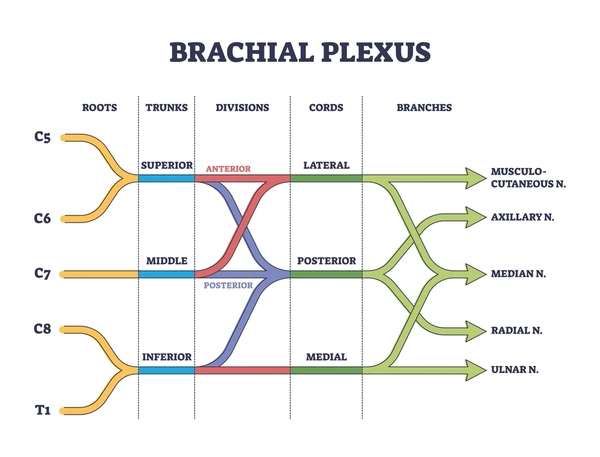
The brachial plexus is a network of nerve roots, connections, and branches that perform related duties. On each side of the body, there is one brachial plexus that contains the nerves supplying each arm. The anatomy, while initially complex, can be made simpler by breaking it down into five separate sections.
The structure
The brachial plexus is made up of the nerve cells that make up its several portions. Nerves are made up of axon fibers, which transport information to and from the brain. The supporting cells that surround nerve cells are called neuroglia. These cells secrete a substance known as myelin, which coats neurons and enables quick message transmission to and from the brain.
The brachial plexus is made up of nerve roots that leave the spinal cord, pass via the cervicoaxillary canal in the neck, cross the first rib, and enter the armpit. It is located in what is known as the posterior triangle of the neck. The brachial plexus is divided into five separate anatomical divisions that differ in both location and composition.
Roots (5):
Five nerves leave the lower cervical and upper thoracic spinal cord (via the ventral rami), marking the beginning of the brachial plexus.
- Four nerve roots (C5–C8) emerge from the cervical spinal cord’s lower region.
- The first nerve to leave the thoracic spinal cord is called T1.
The brachial plexus’s roots arise from the spinal cord and go behind the scalenus anterior. Following that, they emerge alongside the subclavian artery between the anterior and middle scalene muscles.
Trunks (3):
The five nerves combine to form three nerve trunks shortly after they leave the spinal cord.
- Superior (created when C5 and C6 combined)
- Middle (from C7)
- inferior (C8 and T1 branches)
The inferior, or lower, portion of the posterior triangle of the neck is traversed by the nerve trunks. At this point, they cross the first rib and continue laterally around the subclavian artery.
Divisions (6):
- There are six divisions formed by the separation of the three trunks into an anterior (sensory division) and posterior (motor) division.
- These divisions are situated in the back of the collarbone, or clavicle. Above the collarbone are the roots and trunk (supraclavicular), while below are the cords and branches (infraclavicular).
Cords (3):
After that, the six divisions combine to form three cords. These cords, which are lateral, medial, or posterior regarding the axillary artery, are named thus because they are located close to it.
- Lateral cord: The anterior branches of the superior and medial trunks combine to form the lateral cord.
- Medial cord: The inferior trunk’s anterior branch continues as the medial cord.
- Posterior cord: The posterior cord is created when the posterior branches of the three trunks combine.
Terminal Branches:
The three cords then give rise to the five primary upper extremity nerves (the remaining nerves originate via distinct brachial plexus points and are covered below). The location of a potential brachial plexus injury can be determined with great assistance if one is aware of the origins of these nerves as well as their purpose.
- The musculocutaneous nerve: Comes from nerve roots C5–C7 and flexes the upper arm muscles at the elbow and shoulder.
- The axillary nerve: Originating from C5 and C6 nerve roots, it facilitates shoulder rotation and allows the arm to elevate off the body. This nerve passes through the surgical neck of the humerus after emerging from the brachial plexus.
- The radial nerve: Originates at nerve roots C5–T1 and regulates several muscles in the hand, elbow, forearm, and upper arm. The brachial plexus’s main branch is located here. It leaves the brachial plexus and follows the humerus’s radial groove.
- The median nerve: Which originates in the C6–T1 nerve roots, permits movement in the forearm and certain hand regions. The median travel passes anterior to the elbow as it descends the arm from the brachial plexus.
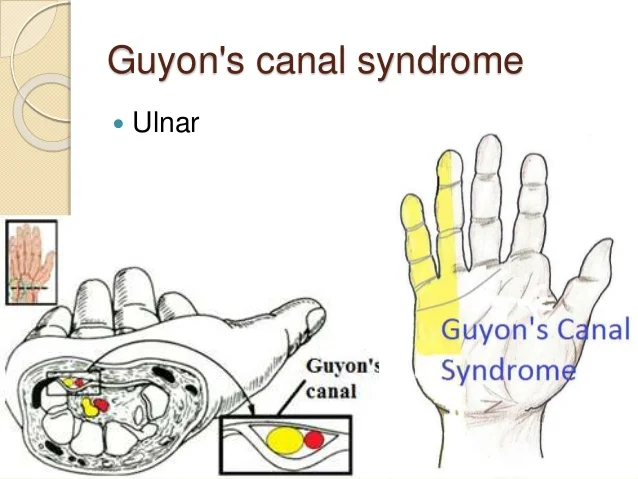
- The ulnar nerve: Originating in C8-T1, this nerve permits the fingers’ fine motor control. The ulnar nerve passes posterior to the medial epicondyle of the humerus after emerging from the brachial plexus.
The musculocutaneous nerve arises from the lateral cord. The radial and axillary nerves originate from the posterior chord. The ulnar nerve originates in the medial chord. The median nerve is produced by the union of the medial and lateral trunks.
Other Branches:
Numerous other “pre-terminal” nerves arise at different locations along the brachial plexus.
Branches from the roots:
- Dorsal scapular nerve
- Long thoracic nerve
- A branch to the phrenic nerve
Branches from the trunks:
- Suprascapular nerve
- Nerve to the subclavius
Branches from the cords:
- Upper subscapular nerve
- Lower subscapular nerve
- Thoracodorsal nerve
Function
- With two exceptions, the brachial plexus innervates the entire upper extremity (the arms and hands) and is responsible for sensation and movement in the forearms, hands, fingers, and upper arms.
- The spinal accessory nerve innervates the trapezius muscle, which is used to shrug your shoulder.
sensitivity to a region close to the armpit that receives innervation from the intercostobrachial nerve instead of the other nerve (this nerve can be injured when breast cancer surgery removes lymph nodes from the armpit).
Motor Function
The following motor functions are performed by the brachial plexus’s five terminal branches:
- The musculocutaneous nerve: The muscles that flex the forearm are supplied by the musculocutaneous nerve.
- Axillary nerve: This nerve controls several arm movements that circle the shoulder joint and innervates the teres minor and deltoid muscle (shoulder anterior flexors). An elbow injury would prevent someone from bending their elbow.
- The ulnar nerve innervates all of the interosseus muscles as well as the medial flexors of the hand, wrist, and thumb muscles. A person may exhibit an “ulnar claw hand,” meaning they are unable to extend their fourth and fifth fingers if they are hurt.
- Median nerve: The thumb and the majority of the forearm flexor muscles are innervated by the median nerve.
- Radial nerve: This nerve supplies innervation to the brachioradialis, extensor muscles of the forearm, and triceps muscle.
When one follows the nerves back to the cords, one finds that the lateral and medial cords give rise to the terminal branches, which in turn innervate the anterior side of the body’s flexor muscles. The extensors are then innervated as a result of the posterior cord.
Sensory Function
All of the upper extremities’ sensation, except a tiny patch under the armpit, is provided by the five terminal branches:
- Musculocutaneous nerve: This nerve is in charge of the forearm’s lateral side sensation.
- The axillary nerve is in charge of feeling in the area surrounding the shoulder.
- Ulnar nerve: The lateral half of the ring finger and the pinky finger are sensed by the ulnar nerve.
- Median nerve: The thumb, index finger, middle finger, medial half of the ring finger, palmer surface of the hand, and upper dorsal surface of the hand all send sensory information to the median nerve.
- Radial nerve: This nerve receives sensory information from the posterior forearm and arm, as well as the back of the hand on the thumb side.
The Autonomic Function
- Additionally, the brachial plexus is linked to nerves that perform autonomic tasks including regulating the arm’s blood vessel diameter.
Types of the Brachial Plexus Injury
The type of damage and the amount of force involved determine how severe a brachial plexus injury is. The same incident might cause injuries to numerous separate brachial plexus nerves, ranging in severity.
Among the most common types of brachial plexus injuries are:
- Stretch (neuropraxia): This condition results from a brachial plexus nerve that has slightly stretched, damaging the nerve’s protective sheath. Though the underlying nerve may not always sustain damage as a result, this impairs the conduction of nerve signals. It might heal itself or need straightforward, non-surgical care to get back to normal, such as physical therapy.
- Rupture: This occurs when a brachial plexus nerve is stretched more forcefully, causing it to rupture entirely or partially. Surgery is frequently an option for healing these kinds of wounds.
- Avulsion: The most serious kind of injury to the brachial plexus. It occurs when your spinal cord is torn apart by the nerve root. Surgery is necessary for certain injuries to restore function.
Causes of the Brachial Plexus Injury
There are several possible causes of brachial plexus injuries, including:
- Forceful trauma.
- Tumors.
- inflammation.
- birth injuries.
Forceful trauma
When your neck is driven up and away from your shoulder and your shoulder is forced down, damage to the upper part of your brachial plexus frequently results. If your arm is suddenly thrust above your head, there is a greater chance that damage will occur to the lower region of your brachial nerves. The following are some causes of trauma that can harm your brachial plexus:
- High-speed accidents involving motor vehicles, particularly those involving motorcycles.
- Falls
- Forceful punches are delivered directly.
- Collisions in contact sports (sometimes referred to as “burners” or “stingers”) are often more modest injuries to the brachial plexus.
- Penetration injuries such as those caused by a knife or a gunshot (violent trauma).
Tumors
- Brachial plexus tumors can press against or grow in the brachial plexus.
- The most prevalent tumors involving the brachial plexus are lung and breast cancers.
- Tumors that can move to your axillary (underarm) lymph nodes and impact your brachial plexus include malignant mesotheliomas, squamous cell carcinomas, melanoma, and lymphomas that start in your head and neck.
Inflammatory reaction
- Your body triggers its immune system when it comes into contact with pathogens (such as viruses, bacteria, or poisonous substances) or sustains an injury. Inflammatory cells and cytokines substances that encourage the production of more inflammatory cells are the first reactions your immune system releases.
- To either start repairing damaged tissue or to trap germs and other harmful agents, these cells initiate an inflammatory reaction. Although in many situations this inflammatory reaction is required, occasionally your immune system will target healthy tissue without any apparent cause. Alternatively, your body may experience a too-strong inflammatory reaction to an offending agent, which could harm bodily tissues.
- Brachial plexus inflammation is caused by a rare disease known as Parsonage-Turner disease (brachial neuritis), which manifests as inflammation without a visible shoulder injury. The symptoms may start as an excruciating arm or shoulder pain and progress to weakening and numbness. Cervical radiculopathy is a common misdiagnosis for this disease.
Birth injuries
Babies may sustain brachial plexus injuries as a result of compression within the uterus of their giving parent or during a challenging delivery. Neonatal brachial plexus palsy is the name given to this injury (NBPP). The following circumstances have the potential to cause harm:
- As the baby’s shoulders go through the birth canal, its head and neck pull to one side.
- Stretching the baby’s shoulders when giving birth head-first.
- Applying pressure on the raised arms of the breech (feet-first) baby during birth.
Symptoms of the Brachial Plexus Injury
Brachial plexus injuries can present with a variety of symptoms, depending on the type of damage and the nerve or nerves involved. If you have more injuries, you can also be experiencing additional symptoms at the same time.
The following are the most typical signs of a brachial plexus injury in both adults and children:
- An extremity that is limp.
- Paralysis of the hand or arm.
- Reduced ability to operate your wrist, hand, or arm muscles.
- Your arm or hand is numb, meaning you cannot feel or sense anything.
- Ache in your wrist, hand, or arm.
- A baby with brachial plexus damage may not be able to move their hands, arms, or lower extremities.
- Absence of the startle reaction, or Moro reflex, on the side which is affected.
- They extend (straight) their arm at the elbow and hold it against their body.
- Reduced force on the injured side.
What differentiates a brachial plexus injury from cervical radiculopathy?
Although they are different illnesses, brachial plexus injuries, and cervical radiculopathy share several symptoms.
- A disorder called cervical radiculopathy, sometimes referred to as “pinched nerve,” causes compression and inflammation of any of the nerve roots in your cervical spine, or neck, leading to neurological impairment. Muscle weakness, numbness, and/or radiating pain are examples of neurological dysfunction.
- In contrast to cervical radiculopathy, which is caused by compression and inflammation, a brachial plexus injury is typically caused by tearing or overstretching the plexus’s nerves.
- Unlike cervical radiculopathy, brachial plexus injuries typically involve several nerve roots and are not associated with neck symptoms like pain or spasms.
Risk Factors of the Brachial Plexus Injury
The risk of brachial plexus injury is increased by involvement in contact sports, especially football and wrestling, as well as high-speed motor vehicle accidents.
Risks Associated with Brachial Plexus Birth Trauma
- Shoulder dystocia, (restriction of the baby’s shoulder on the mother’s pelvis)
- Diabetes in mothers
- large size during gestation
- Challenging delivery requiring outside support
- Prolonged labor
- Breech presentation at delivery
There are no recognized risk factors for more than 50% of brachial plexus injuries.
Diagnosis of the Brachial Plexus Injury
- It is normal for forceful incidents to result in brachial plexus injuries, so if your healthcare practitioner suspects you have one, they will do a thorough examination to diagnose the injury and rule out any additional problems.
- The exact location and extent of the nerve injury will be determined by your provider by looking at every group of nerves connected to the brachial plexus. Your healthcare practitioner will be able to identify possible nerve injury sites with the assistance of the pattern by which nerves from the brachial plexus govern various muscles in your arm and hand.
- Your infant’s doctor will do a physical examination to see whether your baby can move their upper or lower arm or hand if they exhibit symptoms of brachial plexus damage. When their provider rolls them from side to side, their affected arm can fall. The side of the damage also lacks the startle reaction or Moro reflex.
To rule out other potential injuries and assist in the diagnosis of a brachial plexus injury, your healthcare professional may order several tests. Among these tests are:
- X-rays: This imaging procedure uses very small, safe doses of radiation to provide clear images of solid objects, such as bone. To rule out related bone fractures, you’ll probably have X-rays taken of your neck, chest, shoulder, and arm. This is because brachial plexus injuries frequently result from traumatic accidents.
- Computed tomography (CT) myelogram: A CT myelogram uses X-rays and computers to create images around your spinal nerves using a particular dye injection. This allows the physician to see internal body components. According to providers, this imaging technique is the most accurate way to identify injuries caused by spinal nerve avulsions. Additionally, certain medical professionals might employ magnetic resonance imaging (MRI) in addition to or instead of a CT scan.
- Electrodiagnostic exams: These examinations examine muscle signals and nerve conduction. They include electromyograms and nerve conduction investigations. They can find the nerve injury, identify its severity, and assist in determining how quickly the nerve will heal from a brachial plexus injury. After your injury, your doctor will probably do a baseline electrodiagnostic examination three to four weeks later. This makes it possible to identify any potential nerve degeneration.
To determine whether the nerves are regaining their strength, your provider will retake the assessment two to three months following the first one and then on an ongoing basis.
In case your baby exhibits symptoms of a brachial plexus injury, the doctor could ask for an X-ray to check for any fractures in the collarbone. Injury to the brachial plexus in a newborn might mimic pseudoparalysis. This occurs when a baby breaks their arm and becomes immobile due to pain rather than nerve damage.
Differential Diagnosis of the Brachial Plexus Injury
Damage to the brachial plexus might resemble other illnesses’ symptoms. Therefore, to establish an accurate diagnosis, a comprehensive medical evaluation is essential. The differential diagnosis for an injury to the brachial plexus has been simplified as follows:
Disorders of the cervical spine:
- Cervical Radiculopathy: This is brought on by irritation or compression of the cervical spine’s nerve roots. Like a brachial plexus injury, it can result in discomfort, weakness, numbness, and tingling in the arm and shoulder.
- Cervical spondylosis: Brachial plexus injuries might resemble the symptoms of degenerative changes in the cervical spine.
Shoulder difficulties:
- Rotator cuff tear: This condition, which can be misdiagnosed as a brachial plexus injury, results in shoulder pain and weakness due to a tear in the tendons of the rotator cuff muscles.
- Shoulder impingement: Pain and weakness that resemble those of a brachial plexus injury can result from compression of the tendons in the shoulder joint.
Other disorders of the nervous system:
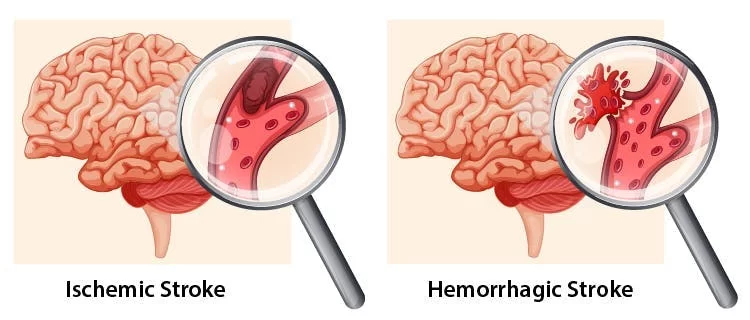
- Stroke: Similar symptoms to those of a brachial plexus injury can result from a stroke that affects the area of the brain responsible for controlling the arm and hand.
- Multiple sclerosis: This neurological condition can affect the arm and hand as well as other regions of the body, causing numbness, weakness, and other symptoms.
- Guillain-Barre syndrome: This autoimmune disease affects the peripheral nerves, causing tingling, weakness, and numbness in the hands and arms as well as throughout the body.
Vascular conditions:
- Thoracic outlet syndrome: Pain, weakness, and numbness in the arm and hand might result from compression of the blood vessels and nerves in the upper chest.
Conditions affecting the muscles:
- Polymyositis: Muscle inflammation that mimics a brachial plexus injury can result in discomfort and paralysis.
Psychological conditions :
- Conversion disorder: Rarely, a psychological disorder can cause symptoms that resemble brachial plexus injuries, such as weakness and numbness.
It’s crucial to remember that this is not a complete list, and a medical expert should do a thorough assessment to rule out any further possible reasons for your symptoms. A physical examination, neurological testing, imaging studies (MRIs, X-rays), and electrodiagnostic testing to evaluate nerve function may be part of this.
Treatment and Management of the Brachial Plexus Injury
Many patients suffer further injuries because brachial plexus injuries are usually the result of acute, powerful events. These could consist of:
- Vein or artery injuries.
- Fractures to the arm, spine, shoulder, or ribs.
- A lung that collapsed.
- spinal cord damage.
- Brain trauma.
This means that before beginning treatment for the brachial plexus injury, your healthcare team may need to attend to these more serious problems. The best care for a brachial plexus injury is provided by a group of medical specialists, which may include
- Neurologist.
- Neurosurgeon.
- surgical hand specialist.
- A physical therapist.
- Occupational Therapist.
- primary supplier of healthcare.
- For brachial plexus injuries, there are two primary treatment options: nonsurgical and surgical.
Conservative Treatment
When it comes to Brachial Plexus injuries, conservative treatment is the best course of action, particularly in mild to moderate cases. Its main goals are to maximize function recovery, reduce problems, and promote nerve repair.
Your physician can decide to wait to do surgery until after your injury recovers if they believe there is a good chance it will heal without surgery. The following are some typical conservative treatment approaches:
Medication
Medication can help control the pain and discomfort brought on by Brachial Plexus injuries, but it cannot heal the underlying injury. This may entail:
- Painkillers are available over-the-counter: Ibuprofen is one example of a nonsteroidal anti-inflammatory drug (NSAID) that can help lessen pain and inflammation.
- Prescription medications: Stronger medications, such as opioids, may occasionally be administered for the acute phase of pain relief to provide short-term pain relief. However, a doctor should continuously monitor their use due to potential dependence and negative effects.
Targeting particular symptoms:
Some drugs can target other symptoms that brachial plexus injuries may cause.
- Anticonvulsants: Drugs such as Pregabalin or Gabapentin can be used to treat neuropathic pain, which is characterized by a tingling or burning feeling that frequently occurs in these situations.
- Tricyclic antidepressants: These are sometimes prescribed to treat brachial plexus injuries together with chronic pain and sleep difficulties.
Physical Therapy
- Physical therapy is a fundamental component of conservative treatment plans. It helps prevent contractures, minimize stiffness, maintain and enhance range of motion, and strengthen muscles.
- Immobilization: Slings or splints may occasionally be used to immobilize the arm and aid in the healing process, particularly in the early phases of an injury.
- Electrical Stimulation: This method helps keep muscles from atrophying and can help with muscle function.
- Nerve Blocks: Local anesthetic or steroid injections can be used to temporarily relieve pain.
- Bracing: Braces can increase joint stability and provide arm support.
Here are some other points to consider:
- Early Intervention: To maximize recovery, physiotherapy must be started as soon as possible.
- Pain Management: Improving the patient’s quality of life and enabling physiotherapy require effective pain management.
- Patient education: Individuals recognize the possibility of long-term healing and actively engage in their rehabilitation program.
- It is noteworthy that conservative measures may not always yield positive results, particularly in cases of serious injuries. To restore function or heal nerve damage, surgery can be required.
When brachial plexus injuries occur, medical professionals usually advise surgery if the nerves are injured and cannot heal sufficiently to regain the necessary function in your arm and hand. It’s crucial to understand that surgery might not be able to restore your arm or hand to its pre-injury state, depending on how severe the injury was.
Depending on the nature and extent of the injury as well as the length of time that has passed since the incident, neurosurgeons treat nerve injuries using a variety of procedures.
Surgical Treatment
- Nerve repair: It involves the attachment of a severed nerve’s two torn edges by your surgeon. Surgeons often tend to you immediately if you suffer a knife wound or other sharp lacerations to your nerves.
- Nerve graft: In this surgery, the ends of a severed (lacerated) nerve are sewn together with a healthy nerve from another area of your body. As your damaged nerve endings grow back together, your healthy transplanted nerve serves as a support system.
- Nerve transfer: When there are no viable nerve stumps in your neck that can be attached to nerve grafts, surgeons will perform nerve transfer surgery. Using this approach, the surgeon cuts the injured nerve and reattaches a healthy donor nerve to give a signal to the paralyzed muscle.
Treatment for brachial plexus injuries in newborns
- Your baby’s doctor may suggest range-of-motion exercises and gentle arm massages as treatments for a moderate brachial plexus injury.
- Your child could require the care of a pediatric neurosurgeon if the damage is extensive or if it does not get better in the first few weeks. If, by the time your infant is three to nine months old, their strength hasn’t improved, they might think about surgery.
Anesthesia-related problems are one of the hazards associated with any surgery
- Infection.
- Significant blood loss.
- Furthermore, you might have extra risk factors if you already have medical disorders that could increase the likelihood of the following complications:
- Persistent discomfort.
- blood clots
- Heart attack
- A stroke.
Complications of the Brachial Plexus Injury
Many brachial plexus injuries in adults and children heal with little to no lasting harm if given adequate time. However, some wounds might result in either short-term or long-term issues, like:
- Joint stiffness. The joints may stiffen if you develop paralysis in your hand or arm. If you finally regain use of the limb, this may make movement challenging. Because of this, your doctor may advise continuing physical therapy as you heal.
- Pain. This is caused by injury to the nerves and could become chronic.
- Numbness. You run the danger of burning or hurting yourself without realizing it if you lose feeling in your arm or hand.
- Atrophy of muscles. After an injury, nerves regenerate slowly and may take years to mend. Muscle breakdown in the affected muscles may occur during that period if they are not used.
- Irreversible impairment. Several variables, such as your age and the kind, location, and severity of the damage, affect how effectively you heal from a significant brachial plexus injury. Some persons have lifelong paralysis or muscle weakness even after surgery.
Living with the Brachial Plexus Injury
If you have sustained a brachial plexus injury, you will require follow-up visits with your medical team at regular intervals to track the healing process and nerve function.
If you have a rehabilitation plan, you will also need to see your physical therapist regularly. To get the finest results possible, you must dedicate yourself to these therapies.
Prevention of the Brachial Plexus Injury
Even though brachial plexus damage is frequently unavoidable, there are things you may do to lessen the likelihood of problems after an injury has happened:
- For itself. Physical therapy together with daily range-of-motion exercises can help prevent joint stiffness if you are temporarily unable to use your hand or arm. Steer clear of wounds and burns since you might not feel them if you’re numb. Your physician might advise you to use special padding to protect the brachial plexus area when playing sports if you’re an athlete who has had brachial plexus injuries.
- For your children. Parenting a kid with brachial plexus palsy requires you to start exercising your child’s joints and functional muscles as early as a few weeks of age. This keeps the working muscles in your child strong and healthy and helps prevent the joints from becoming permanently stiff.
Summary
Nerves recover gradually. After a brachial plexus injury, particularly following surgery, the healing time is frequently prolonged and necessitates a strong dedication to a rehabilitation program to restore physical capacities.
Even though a lengthy rehabilitation can be intimidating, it’s critical to keep an optimistic mindset. Seek assistance from your friends and relatives. Additionally, your healthcare specialists are here to give thorough treatment programs and assistance.
FAQs
What signs and symptoms indicate damage to the brachial plexus nerve?
The arm, wrist, and hand are impacted if there is damage to the nerves that originate lower in the brachial plexus. Typical signs of damage to the brachial plexus include tingling or loss of sensation in the arm or hand. incapacity to move or control the hand, wrist, arm, or shoulder.
How is a brachial plexus injury treated?
To maintain range of motion, avoid stiff joints, and keep the muscles and joints functioning properly, your physician could suggest physical therapy. Generally speaking, brachial plexus nerve restoration surgery needs to happen six months following the damage. Success rates are lower for surgeries performed after that.
Is an injury to the brachial plexus permanent?
Many brachial plexus injuries in adults and children heal with little to no lasting harm if given adequate time. However, some wounds might result in either short-term or long-term issues, like stiff joints. The joints may stiffen if you develop paralysis in your hand or arm.
Which medication benefits brachial plexus patients?
Your range of motion may be restricted by brachial plexus injuries, which can also result in pain in your wrist, hand, arm, neck, or shoulder. For pain treatment, your doctor can suggest an over-the-counter pain reliever such as ibuprofen or acetaminophen. For one or two weeks, a stronger pain reliever may be recommended if necessary.
How is an injury to the brachial plexus diagnosed?
Examining the Brachial Plexus for Injuries your doctor will inquire about your symptoms and conduct a comprehensive physical examination of your neck, shoulders, arms, and hands to identify a brachial plexus injury.
Imaging tests: MRI scans, X-rays, electromyography, a study of Nerve Conduction, etc.
What is the most frequent cause of injuries to the brachial plexus?
The majority of traumatic brachial plexus injuries result from pulling or stretching the arm violently. Numerous incidents, such as falls, car crashes, gunshot and knife wounds, and most frequently, motorbike crashes, can result in injuries.
Does a brachial plexus injury require surgery?
Brachial plexus injuries that are severe enough to require surgery cannot heal on their own. If surgery is necessary, it should be done no later than six months after the accident. The likelihood that a particular muscle can ever function normally again decreases with the amount of time you spend without a nerve activating it.
References
- Brachial plexus injury. (2022, December 22). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/brachial-plexus-injuries
- Brachial plexus injury – Symptoms and causes – Mayo Clinic. (2022, June 3). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/brachial-plexus-injury/symptoms-causes/syc-20350235
- Brachial Plexus. (n.d.). Physiopedia. https://www.physio-pedia.com/Brachial_Plexus
- Brachial Plexus Injury | Symptoms, Diagnosis & treatment. (n.d.). https://www.cincinnatichildrens.org/health/b/brachial-plexus
- Brachial plexus injuries – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/brachial-plexus-injuries/
- Professional, C. C. M. (n.d.-a). Brachial plexus injury. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22822-brachial-plexus-injury
- Eldridge, L., MD. (2023, July 14). The anatomy of the brachial plexus. Verywell Health. https://www.verywellhealth.com/brachial-plexus-anatomy-4777639