Arthritis
Arthritis is a broad term for conditions causing inflammation and pain in the joints. It affects people of all ages, with the most common types being osteoarthritis, which results from wear and tear, and rheumatoid arthritis, an autoimmune disorder.
Symptoms often include joint pain, stiffness, swelling, and reduced mobility. Management strategies vary depending on the type but may include medication, physical therapy, exercise, and lifestyle changes to reduce pain and improve joint function.
The hard, slick substance that surrounds the ends of vertebrae where they unite to create a joint, called cartilage, deteriorates due to osteoarthritis. The disease known as rheumatoid arthritis occurs when the immune system targets the joints starting with the joint lining.
A high blood level of uric acid can result in uric acid crystals, which can lead to gout. Infections or underlying conditions like lupus or psoriasis can induce different kinds of arthritis. Depending on the type of arthritis, different treatments are used. Reducing symptoms and enhancing quality of life are the primary objectives of arthritis therapy.
What is Arthritis?
One condition that damages your joints is arthritis. Where two bones unite in your body is called a joint. As you age, some joints deteriorate naturally. Following that typical, lifelong wear and tear, many people acquire arthritis. Certain forms of arthritis develop as a result of joint damage from injuries. Arthritis can also be caused by certain medical disorders.
Although arthritis can occur in any joint, it most frequently affects people:
- Hands and wrists.
- Knees.
- Hips.
- Feet and ankles.
- Shoulders.
- Lower back (lumbar spine).
A medical professional will assist you in managing pain and stiffness. Eventually, some patients with severe arthritis require surgery to replace the damaged joints.
If you feel like you can’t move or utilize your joints as well as normal, or if your joint pain is severe enough to interfere with your everyday activities, you should see a healthcare professional.
What is the function of a joint?
Where two or more bones touch, like in the fingers, knees, and shoulders, is called a joint. Bones can move freely within certain bounds and are held in place by joints.
The majority of our body’s joints are encased in a robust capsule. A viscous substance that aids in joint lubrication fills the capsule. Our bones are held in place by these capsules. Ligaments assist them in doing this. They resemble extremely durable elastic bands.
Cartilage lines the ends of the bones that make up a joint. As you move, the bones can slide over each other because of this resistant yet smooth layer of tissue. The muscle pulls a tendon that is connected to the bone when our brain signals the muscle to move the bone. As a result, muscles are crucial for maintaining a joint.
Types of arthritis
Arthritis comes in over a hundred varieties. Among the most prevalent kinds are:
Osteoarthritis

Osteoarthritis, the most prevalent kind of arthritis, is caused by wear and tear on the cartilage, which is the firm, slippery layer that covers the ends of bones where they unite to form a joint. The ends of the bones are cushioned by cartilage, which permits almost frictionless joint motion. However, if the cartilage is sufficiently damaged, the bone may grind against the bone, causing pain and limited mobility. A joint injury or infection may accelerate this wear and tear, or it may develop over many years.
The connective tissues that hold the joint together and connect muscle to bone deteriorate and the bones change as a result of osteoarthritis. The lining of a joint may swell and become inflamed if the cartilage is seriously injured. Osteoarthritis is the most prevalent kind of arthritis. In the UK, an estimated 8.75 million people have visited a doctor for osteoarthritis. Cartilage roughening is the first sign of osteoarthritis.
If this occurs, the body may attempt to compensate for the loss of this vital component by implementing a “repair” mechanism. Then, the following may occur:
- Osteophytes are tiny pieces of additional bone that can grow at the ends of bones in joints.
- The quantity of viscous fluid within the joint may rise.
- The joint may become deformed due to the stretching of the joint capsule.
Osteoarthritis can occasionally develop in its early stages with little pain or difficulty. Nevertheless, it may result in pain, stiffness, and internal joint injury. Osteoarthritis often affects adults over 45 and is more common in women. The knees, hands, hips, and back are the body parts most frequently impacted.
Maintaining an active lifestyle will help you keep your weight in check, which will ease the strain on your joints. Regular exercise will maintain the strength of the muscles surrounding a joint, which will support and stabilize an osteoarthritis-affected joint. Being overweight can exacerbate osteoarthritis and increase your risk of developing it.
You can keep active and lessen your symptoms by using non-steroidal anti-inflammatory medicines (NSAIDs) like ibuprofen and painkillers like paracetamol. Additionally, being active will lessen edema, stiffness, and pain. You might apply NSAID creams topically to the affected area. Trying these first would be a good idea.
Numerous options are available for pain alleviation. A doctor or physiotherapist can offer you particular assistance if you’re having trouble managing the pain associated with osteoarthritis.
Your doctor may talk to you about having surgery if your osteoarthritis worsens, especially in your knees and hips. This is typically only taken into consideration after every other therapeutic option has been exhausted. These days, joint replacements are highly effective and advanced.
Rheumatoid arthritis.
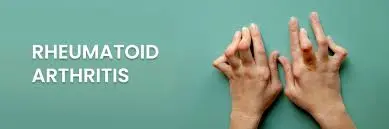
The lining of the joint capsule, a strong membrane that surrounds every joint component, is attacked by the body’s immune system in rheumatoid arthritis. The synovial membrane, the lining, swells and becomes inflammatory. Eventually, the disease process may cause the joint’s bone and cartilage to be destroyed.
One kind of inflammatory arthritis is rheumatoid arthritis. It’s referred to as an auto-immune disease. The body’s natural defense mechanism, the immune system, keeps us safe from diseases and illnesses. In an autoimmune disease, the body’s immune system unintentionally targets healthy tissues, like the joints, resulting in inflammation.
Normally, inflammation is a useful immune system tool. It happens when the body fights an infection by directing more blood and fluid to that location. This is what happens, for instance, when a cut becomes infected and the surrounding skin swells and changes color.
But with rheumatoid arthritis, the excess fluid and inflammation in a joint might lead to the following issues:
- It may cause pain and difficulty when moving the joint.
- The fluid’s chemicals have the potential to harm joints and bones.
- The joint capsule may get stretched by the excess fluid. A joint capsule never fully returns to its initial position after being extended.
- The fluid’s chemicals have the potential to cause pain by irritating nerve endings.
Inflammation can harm a joint permanently in addition to producing pain and stiffness. Early initiation of successful treatment can help minimize damage.
Rheumatoid arthritis symptoms can include:
- Swollen joints.
- Joint edema and stiffness in the morning that persists for more than 30 minutes; extreme exhaustion, sometimes known as fatigue; and a general sense of being ill.
In addition to affecting the same joints on both sides of the body simultaneously, rheumatoid arthritis frequently begins in the little joints of the hands and feet. It may begin more forcefully or more slowly and then progressively worsen.
Adults of any age can develop rheumatoid arthritis. People between the ages of 40 and 60 are most likely to experience its onset. Women are more likely than men to have it.
Some medications can lessen joint pain and swelling by slowing down an overactive immune system. These include biological therapy and are referred to as disease-modifying anti-rheumatic medications (DMARDs). Conventional DMARDs are the first line of treatment for rheumatoid arthritis. When your immune system is overactive and harming your body, these can have the overall effect of lowering its activity.
Doctors will consider considering the more recent biological therapies if these medications have been tried and have failed. The immune system is more specifically affected by biological treatments.
Gout

Gout arthritis causes sharp uric acid crystals to form in your joints. One form of inflammatory arthritis that can cause excruciating joint swelling is gout. Although the big toe is usually affected, other joints in the body may also be impacted.
Gout-affected joints may turn red and heated. Additionally, the skin may peel and seem glossy. It is caused by an excess of urate, also referred to as uric acid, in the body. Everybody has some urate in their bodies.
However, some people may have higher levels of urate in their bodies due to being overweight or consuming excessive amounts of certain foods and alcoholic beverages. Your inherited genes may increase your risk of developing gout.
Urate can crystallize into substances that stay in and around the joint if it reaches a high enough quantity. They can remain there for some time without posing any issues or even letting the person know they’re there. The crystals may fall into the soft area of the joint as a result of a knock on one part of the body or a fever. Swelling and pain will result from this.
Gout attacks can be avoided by taking medications that lower the body’s urate levels. Febuxostat and allopurinol are two examples. Also, you will want temporary pain treatment if you are experiencing a gout attack. Paracetamol and non-steroidal anti-inflammatory medicines (NSAIDs) can be good first-line medications.
Gout is more frequent in women after menopause, but it can strike men as early as their mid-20s. Gout risk may be increased by taking water tablets. Calcium crystals can also form in and around joints as a result of certain situations.
Calcium is necessary for healthy bones and teeth in all of us. On the other hand, excessive calcium levels in some persons might result in the formation of crystals around joints. This may result in excruciating edema.
Diseases caused by calcium crystals usually resolve on their own. The pain and swelling can be reduced by using an ice pack covered with a moist cloth and using NSAIDs and medications.
Spondylarthritis
The term “spondylarthritis” refers to a group of disorders that mostly affect the joints of the spine and produce pain and swelling.
Entheses, which are tiny fragments of connective tissue, become inflamed in these situations. These are strong, tiny cords that connect tendons or ligaments to bones.
Ankylosing spondylitis
Arthritis that affects joints near your lower back. Ankylosing spondylitis is a form of spondylarthritis that mostly affects the joints of the spine and produces pain and swelling.
The body may produce extra calcium in this condition as a result of inflammation surrounding the spine. The body often uses this mineral to strengthen bones. Nevertheless, in ankylosing spondylitis, the excess calcium may induce new bone fragments to form in the spine, resulting in stiffness and pain.
Usually, this problem results in back pain in the second half of the night and swelling that lasts longer than 30 minutes in the morning.
This process can be slowed down by certain medications. Being active can assist in reducing spinal stiffness, and having proper posture will help to prevent the spine from becoming more curved. Typically, ankylosing spondylitis strikes people in their 20s to 30s. Men are more likely to have it.
Psoriatic arthritis

Arthritis affects people who have psoriasis. An autoimmune disease is psoriatic arthritis. It is a form of spondylarthritis as well.
The immune system of the body might result in psoriasis, a red, scaly skin rash, as well as excruciating joint swelling and stiffness. The elbows, knees, back, buttocks, and scalp are among the body parts that may be impacted by the rash. Fatigue, another name for extreme exhaustion, is also frequent.
Biological treatments and disease-modifying anti-rheumatic medications (DMARDs) can address the underlying cause of joint inflammation. Psoriasis can also be treated with a range of products, including pills and lotions.
People who already have psoriasis are typically affected by psoriatic arthritis. Some people, nevertheless, get arthritis before psoriasis. One may have arthritis without any psoriasis at all. Although it tends to affect adults, this illness can affect persons of any age.
Juvenile arthritis
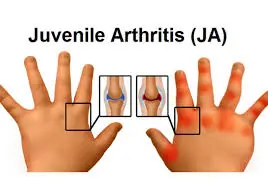
Arthritis in kids and teens younger than 16. Juvenile idiopathic arthritis is the term used to describe inflammatory arthritis diagnosed in a person before the age of sixteen.
Different kinds of JIA exist. These are autoimmune diseases, and joint pain and swelling can be caused by the immune system. The sooner a person receives a JIA diagnosis, the better. This is to minimize any harm to the body and begin an effective treatment.
Non-steroidal anti-inflammatory medicines (NSAIDs) and painkillers are two medications that can help with the symptoms. Biological treatments and disease-modifying anti-rheumatic medications (DMARDs) can reduce or even eliminate the arthritis that is causing the body to swell.
Depending on the kind of arthritis you have, it may result in inflammation (swelling) or degeneration (breakdown) of the natural tissue in your joint. Degeneration results from inflammation caused by certain kinds.
- Other illnesses with symptoms resembling those of arthritis. Different disorders can cause joint pain and even edema.
Lupus
- Lupus An auto-immune disease is lupus. The body’s healthy tissues are mistakenly attacked by the immune system.
- Lupus can have a wide range of symptoms. It may have an impact on the heart, lungs, and other body organs.
- Lupus frequently causes joint pain and swelling, especially in the little joints of the hands and feet. In lupus, joint pain may shift from one joint to another.
- Since lupus can present a wide range of symptoms that frequently mimic those of other conditions, it can be challenging to diagnose.
Fibromyalgia
- A chronic illness that can produce pain and soreness throughout the body is fibromyalgia.
- The symptoms may resemble those of arthritis. But rather than the joints, the muscles are where the symptoms are most noticeable.
The following are the most typical signs of fibromyalgia:
- Widespread pain
- Sleep can be unrefreshing when it does occur.
- Fatigue
- Headaches
- Amnesia
- You’re most likely extremely sensitive to pressure or pain if you have fibromyalgia.
Polymyalgia rheumatic (PMR)
- The disorder known as polymyalgia rheumatica (PMR) causes stiff and aching muscles. Thighs, shoulders, and hips are frequently impacted.
- Having both arms raised above your head can be challenging and painful. Usually, the stiffness and soreness are greatest in the morning. Fatigue and a general sense of being ill are additional symptoms.
- The majority of those affected are above 70.
- A disorder known as giant cell arteritis (GCA) can strike some individuals with polymyalgia rheumatica. This might cause pain and tenderness around the side of the head because it affects the blood vessels in the head.
- In rare instances, giant cell arteritis can result in visual issues or even blindness. It can also cause pain in the jaw or tongue during chewing. You should see a doctor immediately if you encounter any of these symptoms. Giant cell arteritis can cause irreversible vision loss, including blindness if treatment is not received.
- Steroids, usually in the form of pills, are an effective treatment for both giant cell arteritis and polymyalgia rheumatica.
Back pain
- Many of us suffer from back pain, which is a typical issue. It is typically not the result of a significant issue, but rather of a simple strain of a muscle or ligament. Perhaps there isn’t even a cause.
- In most cases, back pain goes gone in a few weeks.
- The greatest course of action when taking painkillers is frequently to stay active.
Tendinopathy
- Tendons, the robust cords that connect muscles to bones, can become painful when a person has tendinopathy.
- The affected area may be red, swollen, and heated. This may make it challenging to move that bodily part. Additionally, you may experience a grating feeling.
- Overuse of that bodily part may be the cause of this. The first step to rehabilitation can be to stop or change the activity that created the issue.
- Taking pain medication and staying generally active can also be beneficial.
- Pain and swelling can also be decreased by applying an ice pack, such as a tea towel wrapped around a bag of frozen peas.
Signs and symptoms
The joints are the site of the most prevalent arthritic symptoms. The following signs and symptoms may be present, depending on the type of arthritis:
- Joint pain.
- Stiffness or decreased range of motion (the amount of movement a joint can produce).
- Swelling (inflammation).
- Skin discoloration.
- Sensitivity or tenderness to touch in the surroundings of a joint.
- A sensation of warmth or heat close to your joints.
Swelling and pain in any number of joints are symptoms of arthritis. Joint stiffness and pain are the primary signs of arthritis, and they usually get worse with age. The two most prevalent forms of arthritis are rheumatoid arthritis and osteoarthritis.
The type of arthritis you have and the joints it affects will determine where your symptoms appear. Flares or flare-ups are the sporadic waves of symptoms associated with some kinds of arthritis. Others cause constant pain or stiffness in your joints, especially after physical activity.
Causes
The causes of arthritis differ based on the type you have:
- As you age, osteoarthritis develops naturally because continuous use of your joints can wear down the cartilage that cushions them.
- If you have hyperuricemia or too much uric acid in your blood, you may have gout.
- When your immune system accidentally destroys your joints, it can result in arthritis, particularly rheumatoid arthritis.
- COVID-19 is one of the viral diseases that can cause viral arthritis.
- Arthritis can occasionally occur without a known cause or trigger. Physicians refer to the condition as idiopathic arthritis.
Rheumatoid arthritis and osteoarthritis, the two primary forms of arthritis, cause various kinds of joint damage.
Risk Factor
Among the risk factors for arthritis are:
- Family background. Since some forms of arthritis are inherited, having parents or siblings with the condition may increase your risk of getting it yourself.
- Age. As people age, their risk of developing various forms of arthritis, such as gout, rheumatoid arthritis, and osteoarthritis, rises.
- Sex. Rheumatoid arthritis is more common in women than in men, whereas gout, another form of arthritis, is more common in males.
- Prior joint damage. Individuals who have had a joint injury, possibly during athletic activities, are at an increased risk of developing arthritis in that joint in the future.
- Overweight. Being overweight strains your joints, especially your spine, hips, and knees. Arthritis is more likely to occur in obese people.
- Use of tobacco: Using tobacco products, including smoking, raises your risk.
- Activity level: If you don’t engage in regular physical activity, you may be at a higher risk of developing arthritis.
- Additional medical conditions: Your risk of developing arthritis is increased if you have autoimmune illnesses, obesity, or any other condition that affects your joints.
Some individuals are more likely to get arthritis, such as:
- Individuals above 50.
- Women.
- Sportsmen, particularly those who participate in contact sports.
- Those who work in physically demanding occupations or perform tasks that strain their joints, such as standing, squatting, spending a lot of time on their hands and knees, etc.
Diagnosis
A medical professional will use a physical examination to diagnose arthritis. They will interview you about your symptoms and inspect the affected joints. Inform your healthcare physician about the onset of symptoms such as pain and stiffness and whether certain activities or times of day exacerbate them.
Your range of motion, or how far a joint can move, will most likely be assessed by your healthcare professional. The range of motion of one joint might be compared to that of other, comparable joints (your other knee, ankle, or fingers, for instance).
Investigation
Your doctor may capture images of your joints using imaging tests, such as:
- X-ray.
- Ultrasound.
- Magnetic resonance imaging (MRI).
- A computed tomography (CT) scan.
Your doctor can detect joint deterioration with the use of these tests. They can also assist your healthcare professional in ruling out other conditions or traumas, such as bone fractures, that may be causing similar symptoms.
If your doctor believes you have gout, they may perform blood tests to measure your uric acid levels. Additionally, blood testing may reveal indications of autoimmune disorders or infections.
Treatment for arthritis
What is the treatment for arthritis?
Although there isn’t a cure for arthritis, your doctor can help you find ways to manage your symptoms. The cause of your arthritis, its type, and the joints it affects will determine the treatments you require.
The most popular therapies for arthritis include:
Anti-inflammatory medications, such as acetaminophen or NSAIDs. Prescription anti-inflammatory drugs, such as cortisone injections, are known as corticosteroids.
Medications are known as disease-modifying antirheumatics (DMARDs) if you suffer from psoriatic or rheumatoid arthritis. You can increase your strength, range of motion, and self-assurance when moving with the use of physical therapy or occupational therapy.
Exercise for arthritis
- Low-impact exercise is typically the most effective for people. Exercises like yoga, Pilates, Tai Chi, swimming, cycling, and brisk walking have all been beneficial for those with arthritis. Finding something you enjoy will help you stick with it.
- When you work out, you could experience some pain. This sensation is common and should subside a few minutes after you’re done. It doesn’t mean you’re harming yourself. Exercise can help you better manage your arthritis and lessen pain.
- You can exert yourself and engage in intense exercise, but it’s crucial to avoid going beyond. If you experience unbearable pain during or after your activity, you will have to Another crucial component of keeping a healthy weight is regular exercise. Relieving joint pressure will alleviate your pain. Inflammation is more prone to occur in those who are overweight.
- Eating a balanced, healthy diet that is low in fat and sugar is the greatest method to reduce weight. Make sure you consume a lot of fresh produce, stay hydrated, and get regular exercise. You will lose weight if your daily caloric expenditure exceeds your daily caloric intake.
- See a doctor or physiotherapist if you are ever having trouble staying active and need encouragement or support.
- Another choice, if you have the funds, would be to regularly work out with a personal fitness trainer at a gym. Someone who is certified as a level two or higher personal trainer will be able to track your progress and offer you advice on the exercises that will work best for you. Be sure to explain your problem to them.
- Surgery (typically only if your symptoms are not relieved by nonsurgical therapy).
Surgery for arthritis
- If various therapies are ineffective for your severe arthritis, surgery may be necessary. Joint replacement and joint fusion are the two most popular forms of arthritis surgery. The process of surgically connecting bones is known as joint fusion. It most frequently affects the bones in your ankle (ankle fusion) or spine (spinal fusion).
- You may require an arthroplasty (joint replacement) if your joints are damaged or you have lost bone. Your damaged natural joint will be removed by your surgeon and replaced with an artificial joint, or prosthesis. A partial or complete joint replacement may be necessary.
- You will learn what to anticipate and what kind of surgery you will require from your physician or surgeon.
There is not always a way to prevent arthritis because some types develop naturally or as a result of uncontrollable medical disorders. Nonetheless, you can reduce your risk of arthritis.
Complication
It might be challenging to perform daily duties if you have severe arthritis, especially if it affects your hands or arms. Weight-bearing joint arthritis might make it difficult to sit up straight or walk comfortably. Joints may occasionally progressively lose their form and alignment.
Prevalence
Arthritis is very prevalent. According to experts, about one-third of Americans suffer from some form of joint arthritis. The most prevalent kind is osteoarthritis. According to studies, approximately 50% of adults will eventually get osteoarthritis.
- Staying away from tobacco products.
- Maintaining a healthy diet and exercise regimen.
- Engaging in low-impact workouts.
- When engaging in any activity that could harm your joints, always wear the appropriate protective gear.
Prognosis
You will likely need to manage your arthritis symptoms for the remainder of your life. Your doctor will assist you in locating therapies that lessen the frequency and severity of arthritis’s effects on your day-to-day activities.
As they get older, some arthritis sufferers have worsening symptoms. Find out from your doctor how frequently you should schedule follow-up appointments to monitor any changes in your joints.
What age does arthritis usually start to manifest?
Any age can be affected by arthritis. The type you have and the cause will determine when it begins. Adults over 50 are typically affected by osteoarthritis. Adults between the ages of 30 and 60 are typically affected with rheumatoid arthritis.
Near that particular trigger is typically where other sorts that have an improved direct cause begin. Gout doesn’t appear until after high uric acid levels have been present for at least a few months, and patients with post-traumatic arthritis don’t get it until after their joints have been harmed.
Discuss your risk for arthritis and when to begin looking for symptoms or changes in your joints with your healthcare professional.
How can arthritic pain be relieved the quickest?
- No one solution works for everyone because every person’s body reacts differently to various therapies. To alleviate your arthritis pain, your healthcare practitioner will assist you in identifying a mix of treatments. When you notice that your arthritis symptoms are getting worse, you may be able to start taking prescription or over-the-counter medication. To prevent pain before it becomes severe enough to interfere with daily activities, some people take arthritis medication regularly.
- One of the best strategies to reduce the symptoms of arthritis is to continue being active. Stretching and exercising your body can help ease pain and stiffness and keep them from getting worse, but avoid forcing yourself to do anything that hurts a lot.
- Being an Olympic weightlifter or ultramarathon runner is not necessary. Stretching or yoga, swimming, biking, and walking are all excellent ways to develop your muscles and support your joints.
- Consult your healthcare physician or physical therapist about healthy exercise options. They will provide ways for you to be active in a safe manner.
FAQs
What is arthritis’s primary cause?
Overuse or gradual joint wear and tear are the two main causes of osteoarthritis. The body’s immune system attacking its tissues is the cause of rheumatoid arthritis, lupus, and scleroderma. Gout is caused by crystal buildup in the joints. Genes may play a role in some types of arthritis.
How can arthritis be treated?
Self-care: Reduce weight if necessary; substitute low-impact exercises like swimming or walking for high-impact ones like running; and stay away from exercises that could exacerbate the problem, such as squats and lunges. For pain, use heat or ice, and discuss using NSAIDs with a physician.
Can someone with arthritis lead a normal life?
Your arthritis won’t worsen as long as you exercise at the appropriate level and kind for your condition. Regular exercise will help you lose weight and ease the strain on your joints when combined with a nutritious, well-balanced diet. The kind and intensity of exercise that is best for you can be suggested by your doctor.
Why does arthritis hurt?
The ends of the bones are cushioned by cartilage, which permits almost frictionless joint motion. However, if the cartilage is sufficiently damaged, bone may grind against bone, causing pain and limited mobility. A joint injury or infection may accelerate this wear and tear, or it may develop over many years.
How does arthritis begin?
Arthritis comes in more than 150 varieties. Some types of arthritis have no known origin, while others might be caused by illness, infection, genetic flaw, trauma, or overuse. Over 50 million persons in the US suffer from arthritis, which is the leading cause of disability in the country.
Can we completely cure arthritis?
Even while there isn’t a cure for arthritis, recent years have seen significant advancements in treatment, and early intervention is beneficial for many types of arthritis, especially inflammatory arthritis. It could be hard to pinpoint the source of your arthritis.
Which five vegetables should people with arthritis avoid?
Some arthritis sufferers claim that nightshade vegetables, like peppers, eggplants, tomatoes, and potatoes, trigger flare-ups in their condition. Tomatoes might be an exception to the general rule that there is no evidence linking arthritis pain to nightshades. That’s because they cause uric acid levels to rise.
Is arthritis a serious condition?
Certain forms of arthritis need to be treated right away. Receiving treatment as soon as possible can assist in maintaining joint function and avert other major health issues if you have a form of arthritis that can result in irreversible joint damage.
Reference
- Arthritis – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/arthritis/symptoms-causes/syc-20350772
- Arthritis. (2025, February 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12061-arthritis
- Branch, N. S. C. a. O. (2025, January 8). NIAMS health information on arthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/arthritis
- Arthritis. (n.d.). Versus Arthritis. https://versusarthritis.org/about-arthritis/conditions/arthritis/







45 Comments