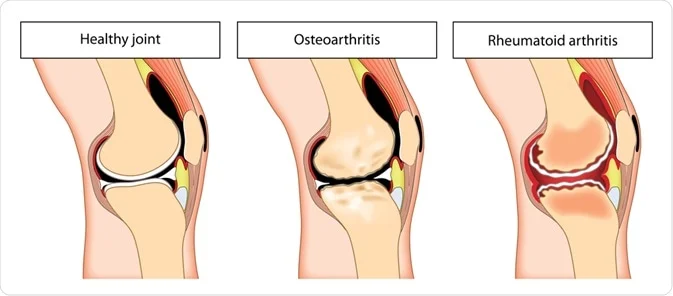
Rheumatoid Arthritis vs Osteoarthritis
Rheumatoid Arthritis vs Osteoarthritis: What Are They?
Rheumatoid arthritis (RA) and osteoarthritis (OA) are common forms of arthritis. Both leads to joint pain and joint degeneration, but they are unrelated disorders.
RA is an autoimmune disorder. It happens when your immune system does not function properly. When you’re healthy, your immune system Eliminates invaders like germs and viruses. When you have RA, your immune system perceives your joints as opponents and begins attacking them. These attacks specifically target the synovial membrane, which lubricates and protects joints.
OA is not an autoimmune disorder. It develops when the cartilage (spongy tissue) between your joints deteriorates, which is frequently caused by normal wear and strain. As a result, the bones on each side of the cartilage begin to shift and pain. It is far more prevalent than rheumatoid arthritis.
These may be the most significant distinctions between RA and OA. However, many others can help doctors determine which kind you have and how to treat it.
Causes of Rheumatoid Arthritis and Osteoarthritis:
Osteoarthritis is caused by wear and tear on joint cartilage by aging, injury, or misuse. Rheumatoid arthritis, on the other hand, is an autoimmune disorder in which the immune system wrongly assaults the joints, causing inflammation and damage.
Causes of Rheumatoid Arthritis:
Rheumatoid arthritis (RA) is an autoimmune condition in which the immune system incorrectly assaults the body’s joints. Environmental stimuli, such as infections, smoking, or hormonal changes, may stimulate the immune response in addition to genetic predisposition.
This causes inflammation in the synovium (joint lining), resulting in cartilage and bone loss. The precise etiology is complicated, involving a combination of genetic, environmental, and immunological variables that all contribute to the start and progression of RA.
Causes of osteoarthritis:
Osteoarthritis (OA) is largely caused by the deterioration of joint cartilage over time.
Aging gradually lowers cartilage’s capacity to heal itself, resulting in its steady degeneration. Joint injuries and overuse, which are frequent in occupations or activities that require repetitive motions, also contribute.
Genetic predisposition, obesity, and joint misalignment can all increase cartilage deterioration. These elements work together to gradually destroy the protecting cartilage, exposing bones and generating osteoarthritis symptoms such as pain, stiffness, and impaired joint function.
Signs and Symptoms of Rheumatoid Arthritis and Osteoarthritis:
Several symptoms may help you decide which of the two underlying diseases your family member is suffering from.
Rheumatoid arthritis symptoms:
- Rheumatoid arthritis (RA) frequently causes symmetrical joint pain and swelling on both sides of the body. The symmetrical pattern of inflammation distinguishes RA from other types of arthritis.
Fatigue
Fatigue is a typical symptom of rheumatoid arthritis (RA), which goes beyond joint pain. Chronic inflammation and the immunological response in RA can produce chronic weariness and weakness, limiting everyday activities. Fatigue is frequently disproportionate to activity levels and can have a substantial impact on RA patients’ quality of life.
Rheumatoid nodules and Skin Changes
Rheumatoid arthritis (RA) can cause rheumatoid nodules, which are solid lumps under the skin that usually form in pressure areas. Skin changes such as redness or inflammation surrounding these nodules might arise, exacerbating the symptoms of RA.
Fever and Weight Loss
Rheumatoid arthritis (RA) may be accompanied by fever and inexplicable weight loss, which are signs of systemic inflammation. The body’s immunological reaction to RA frequently results in persistent low-grade fevers and unintentional weight loss, which indicate extensive inflammation outside of the joints and affect general health and well-being.
Effect on Daily Functioning and Mobility
Mobility and day-to-day functioning can be significantly impacted by rheumatoid arthritis (RA). Stiffness, edema, and joint pain limit movement and make daily responsibilities difficult. The progressive nature of RA can severely impair a person’s capacity to carry out daily tasks on their own.
Symptoms of osteoarthritis:
- Osteoarthritis (OA) causes joint pain and stiffness as a result of cartilage degradation. Friction between bones occurs as a result of deterioration, producing pain and restricted movement. Pain often intensifies during or after exercise and may improve with rest. Stiffness, particularly after periods of inactivity or upon awakening, arises as a result of decreased joint lubrication, making movement difficult until the joint warms up.
Pain and stiffness around joints
Pain and stiffness around joints are more common in osteoarthritis.
Reduced Range of Motion
The breakdown of cartilage and bone spurs in osteoarthritis (OA) can hamper joint mobility, resulting in stiffness and a reduced range of motion. This limitation mostly affects weight-bearing joints, limiting everyday activity and flexibility.
Joint Noise During Movement (Crepitus)
Joint noise, commonly characterized as a grating or popping feeling known as crepitus, comes as a result of roughened or uneven joint surfaces caused by cartilage degeneration. This audible sound may come with movement restriction and indicate OA-related changes within the joint.
Joint deformities and bone spurs.
Long-term cartilage deterioration in osteoarthritis (OA) can result in joint abnormalities and bone spurs. These bony projections can occur around damaged joints, resulting in apparent abnormalities and perhaps restricting joint mobility.
Rheumatoid arthritis vs osteoarthritis in the hands:
Hand symptoms can be caused by both RA and OA, although they are not the same.
Hand RA is prevalent and typically affects both hands. It usually affects the knuckles and wrists.
Swollen joints in RA can make your fingers appear sausage-like. Your fingers’ positions may also shift with time. Even the tendons that enable your fingers to flex and straighten can be harmed and broken by RA. You may occasionally have tingling and numbness in your fingertips.
While it may first affect both hands, OA is more likely to initially affect one. That’s because OA affects the joints you use the most. The base of your thumb and the finger joints closest to your fingernails are the most likely to be affected by OA. It can also affect the wrist.
Osteoarthritis can develop bony lumps over finger joints.
Affected Areas: Osteoarthritis vs Rheumatoid Arthritis:
Osteoarthritis (OA) is typically associated with weight-bearing joints such as the knees, hips, and spine owing to wear and tear. In contrast, rheumatoid arthritis (RA) is systemic, affecting smaller joints symmetrically, particularly the hands, wrists, and feet.
However, RA can also affect bigger joints as the shoulders and knees. Unlike OA, which is localized, RA’s inflammatory process can affect several joints at the same time, resulting in broad and frequently symmetric joint pain, edema, and stiffness across the body.
Diagnosis of Rheumatoid Arthritis and Osteoarthritis :
Rheumatoid arthritis (RA) is diagnosed by imaging, blood testing for certain antibodies, symptom assessment, and occasionally joint fluid study. The American College of Rheumatology’s criteria, which evaluate joint involvement, blood tests, and symptom duration to distinguish RA from other forms of arthritis, such as OA, are also used to diagnose RA. Osteoarthritis (OA) is frequently diagnosed by physical examination, imaging (MRIs, X-rays), and symptom assessment.
Treatments for Rheumatoid Arthritis and Osteoarthritis:
Both RA and OA have no known treatment, and joint damage cannot be undone. The goal of treatment for both conditions is to lessen pain and improve joint function. However, slowing or stopping disease activity—making your body stop attacking itself—is the primary objective of treatment for RA.
With both RA and OA, you may work with occupational therapists to learn strategies that improve your everyday functioning and with physical therapists to learn beneficial exercises. To relieve aching joints, you might use heat and cold. Treatment may sometimes involve surgeries, such as joint replacements.
However, an essential component of treatment for both illnesses is medicine.
Drugs for RA
- NSAIDs, or nonsteroidal anti-inflammatory medicines, are medications that lessen inflammation and discomfort.
- Strong anti-inflammatory drugs called corticosteroids can also aid in immune system regulation.
- Disease-modifying medications that delay the progression of the illness, such as biological medications and conventional disease-modifying antirheumatic medications, or DMARDs.
- Pain is lessened by paracetamol, but inflammation is not.
Drugs for OA
- Pain-relieving creams and gels.
- NSAIDs.
- Pain relievers such as paracetamol.
- The antidepressant medication duloxetine (Cymbalta), can help with chronic pain.
- Corticosteroids and lubricants are injected into the joints.
- You may have noticed that opioids, often known as narcotics, are not on either list. They are rarely given for RA and OA because of the danger of long-term adverse effects such as excessive weariness, constipation, and dependence.
Physiotherapy Treatment for Rheumatoid Arthritis and Osteoarthritis:
The goal of Physical Therapy:
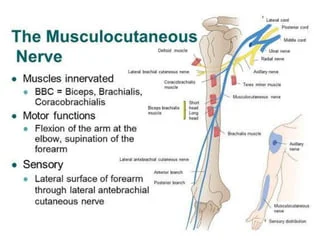
- Reduce pain and inflammation: Physiotherapists utilise a variety of techniques to reduce pain and inflammation, including manual treatment, exercise, and modalities such as heat, cold, and electrical stimulation.
- Improve joint mobility and function: arthritis can cause stiffness and loss of motion in the joints. Physiotherapy helps improve joint range of motion and flexibility, making moving about and doing daily chores easier.
- Strengthen your muscles: Weak muscles might result in joint discomfort and instability. Physiotherapy can help to strengthen the muscles around the joints, relieve pain, and improve function and balance.
- Maintain or enhance physical fitness: Regular exercise benefits both general health and well-being, as well as the management of arthritis. Physiotherapists can help you build a safe and successful exercise regimen that is tailored to your unique needs.
- Education about disease: Physiotherapists may educate patients about arthritis, how to manage their symptoms, and how to avoid future complications. This education may empower patients to take an active part in their treatment, enhancing their overall quality of life.
- Balance issues: Arthritis may increase the risk of falling. Physiotherapy can enhance your balance and reduce your risk of falling.
- Gait abnormalities: arthritis can change the way you walk. Physiotherapy can help you improve and optimize your gait.
- Painful activities: arthritis may make it difficult to do some jobs. Physiotherapy can help you modify your activities so that you can continue doing what you like.
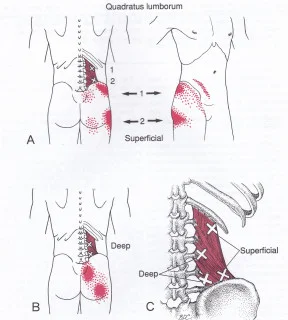
Physiotherapy for RA focuses on managing pain and improving joint function:
- Exercise programs that emphasize range of motion and strength training are tailored to suit joint inflammation and restrictions.
- Heat and cold therapy can help relieve pain and inflammation in affected joints.
- Splinting or bracing can help support and protect inflamed joints, reducing pain during activity.
Physiotherapy for OA requires to enhance joint function and manage pain using several approaches:
- Exercise regimens emphasize flexibility, strength, and low-impact activities to improve joint mobility.
- Heat and ice packs can help to alleviate pain and swelling while also relaxing the muscles around damaged joints.
- Manual therapy techniques like joint mobilization or manipulation can help decrease stiffness and enhance the range of motion.
- Education on optimal posture, movement mechanics, and assistive equipment for relieving stress on damaged joints.
8 Best Exercises for Knee Arthritis:
Ankle Circles:
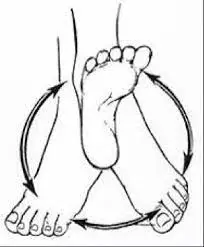
Keep your legs out in front of you, and slowly turn your ankles in a clockwise and anticlockwise direction.
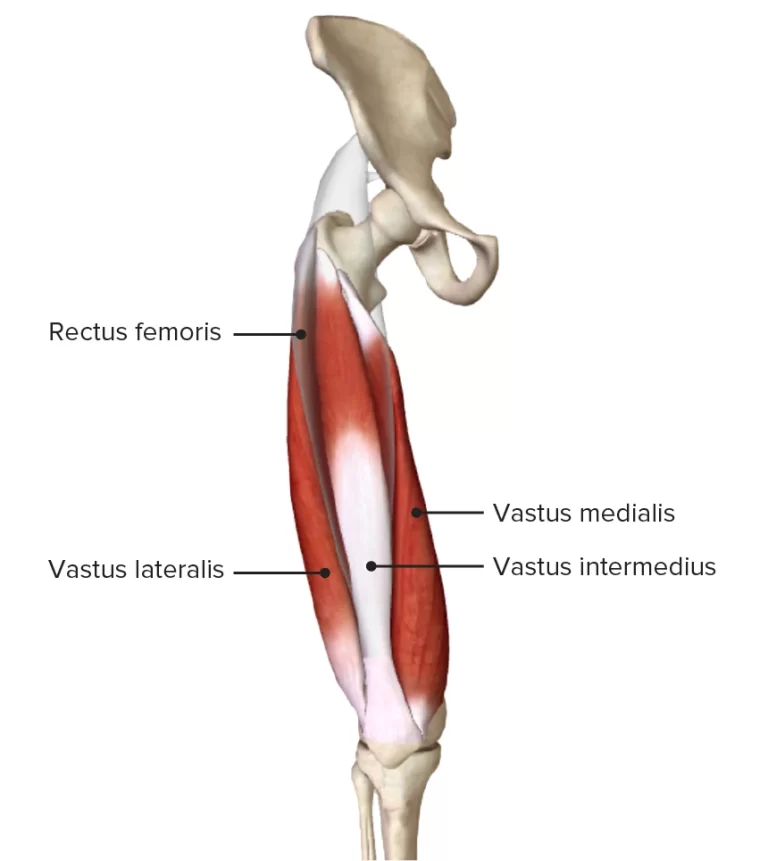
Quad Set

Both legs should be straight out in front of you while you sit.
Push your knee in the direction of the bed.
The muscles in the front of your thigh should start to tighten.
For ten seconds, tighten your muscles. Do this ten times. Do it once every day.
Straight-Leg Lift Exercise

Begin by bending your left leg upward while resting on your back. Make sure your right leg is straight out and fully stretched. Maintaining your right leg locked straight, slowly elevate it to a 45-degree angle. After five seconds of holding, gradually return to the flat, resting position. Since the first two feet off the ground are the most challenging, it is not required to raise the leg straight up to 90 degrees. Twenty times over, repeat. Change to the left leg.
Knee Full Extension Exercise

To begin, sit in a chair high enough to allow the knee to bend to a 90-degree angle. Raise the leg gradually until it is horizontal. After five seconds of holding it, carefully let it go to the floor. Continue with the opposite leg. If you can, perform twenty repetitions.
Hip Abduction (Side-Lying)

Place a pillow under your head and lie on your unaffected side.
Maintaining your body perpendicular to the bed and the affected leg straight, bend the bottom (unaffected) leg.
Raise the affected leg off the bed.
Your buttock muscles need to be active.
For ten seconds, hold your leg up. Do this ten times. Do it once every day.
Double Knee To Chest
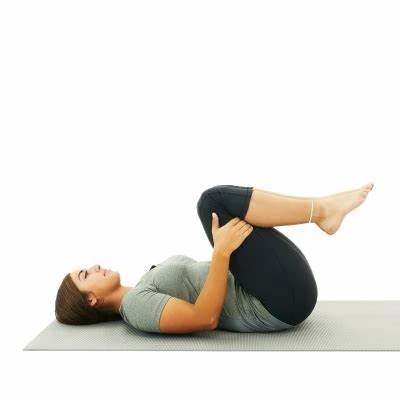
To begin, lie on your back and stretch your legs. Place your hands on the top of the shin, beneath the knee area, and bring both knees up together. You can also lay your hands on the backs of your thighs. Bring your knees slowly up to your chest, hold them there for 10 seconds, and then return to the starting position.
Sit-To-Stand Exercise
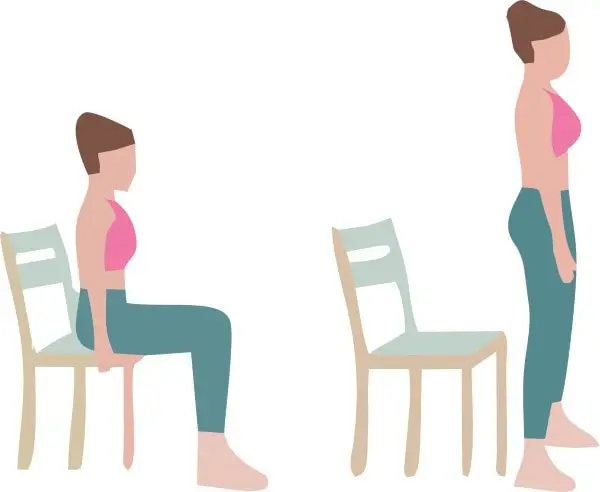
Stand from a chair at a suitable height with your arms crossed; a taller chair might facilitate the task.
By bending one knee a little more than the other, you can put more weight on the leg you want to strengthen the most.
Return to your seated position gradually.
Do this ten to fifteen times, or as often as you can.
Hamstring Stretch

As indicated, sit on the floor with your right leg bent and your left leg extended. Reach for your left foot’s toes with both outstretched hands. Don’t bounce, simply stretch slowly. Return to the starting position after attempting to maintain the stretch for ten seconds. Before switching legs, complete 10 repetitions.
Self-Care for Rheumatoid Arthritis and Osteoarthritis:
Rheumatoid Arthritis:
Working with your doctor to ensure that you receive adequate medical therapy is critical, but you may also make efforts to manage your RA and decrease pain and tiredness. Diet, exercise, smoking cessation, and mental well-being are all critical components of maintaining good health and controlling RA.
Our pain resources can assist you in setting health goals and managing your suffering.
Healthy Eating. A balanced, nutritious diet that contains enough amounts of each food type enhances health and makes it easier to maintain a healthy weight.
Daily movement. Even if you don’t have time to exercise, try to include movement into your everyday routine. Use the stairs rather than the lift. Park in an area where you will need to walk a short distance to reach a building. Travel bigger distances to your workplace meeting.
Balancing activity and relaxation. it is critical to maintain physical activity even during a illness, but rest is especially vital when RA is active and joints are painful, swollen, or stiff. Rest helps to reduce the inflammation and exhaustion associated with a illness. Taking pauses during the day preserves joints and conserves energy.
Treatment options include both hot and cold. Heat treatments, such as heat pads or warm baths, are very beneficial in treating tight joints and weak muscles. Cold is good for relieving acute pain and swelling in joints. It may reduce pain and inflammation.
Topical products. Creams, gels, and stick-on patches can help alleviate joint or muscle discomfort. Some products contain medicine, while others uses nerve-irritating ingredients to relieve pain.
Lowering stress and using supplementary therapy. You may relax and divert your attention from discomfort in several ways. Examples include deep breathing, visualizations of joy, and meditation. Stress and anxiety can be decreased, stiff muscles can be relaxed, and pain can be relieved by massage. To alleviate pain, acupuncture involves inserting tiny needles into certain bodily locations. Acupressure uses strong pressure if you don’t like needles. Acupressure uses strong pressure if you don’t like needles.
Supplements. Studies have demonstrated that omega-3 fish oil supplements and curcumin/turmeric can reduce morning stiffness and rheumatoid arthritis symptoms. But before you take any supplements, talk to your doctor about any possible negative effects and how they could affect other prescriptions you are taking.
A supportive network and a positive outlook. Make a network of family, friends, and coworkers that are willing to assist you emotionally. To lift your spirits and ease your discomfort, spend some time doing the activities you like.
Osteoarthritis:
The greatest technique to avoid osteoarthritis is to maintain good general health, including:
- Avoiding tobacco products.
- Engaging in low-impact physical activity.
- Adhering to a healthy diet.
- Wear a seatbelt at all times.
- Wear the appropriate safety gear for the sport, activity, or work you are doing.
- As soon as you observe any changes in your joints, you should see a doctor.
Keep your weight within a healthy range. Being overweight increases the load on your joints and increases your chance of developing osteoarthritis.
Continue to be active. Frequent exercise helps to protect your joints by strengthening the muscles that surround them.
Choose low-impact pursuits. Compared to sprinting and leaping, swimming, walking, and bicycling are all lower-impact activities. Before working out, warm up.
Cool down once your workout is over. Reducing body temperature helps prevent stiffness and pain in the muscles.
Use proper form when exercising. Avoiding excessive strain on your joints can be achieved by using the proper forms.
Put on supportive footwear. Your joints can be protected and shock can be lessened with supportive footwear.
Consume a healthy diet. Eating a healthy diet can help keep joints healthy and reduce inflammation.
Don’t smoke. You run a higher chance of getting osteoarthritis if you smoke.
Make routine appointments with your physician. Frequent exams might help you identify any early osteoarthritis symptoms so you can start treatment sooner.
Risk Factors for Rheumatoid Arthritis and Osteoarthritis:
Rheumatoid Arthritis :
- Increased incidence of RA in families as a result of the interaction between environmental factors and patient genetics.
- Air pollution, excessive iron and salt intake, low vitamin D levels, female sex, and occupational dust (silica) are risk factors. smoking (RA seroprevalence). poor socioeconomic status and obesity.
- The risk of mortality is increased by the use of statins, oral contraception/hormone replacement therapy, a healthy diet, moderate alcohol usage, and intake of fish and omega-3 fatty acids.
Several risk factors increase your chance of developing rheumatoid arthritis. This comprises:
- Age. The chance of getting rheumatoid arthritis rises with age, even though it can strike at any age. Just like rheumatoid arthritis, juvenile idiopathic arthritis can strike kids and teens.
- Sex. The prevalence of rheumatoid arthritis is higher in women than in males. About two to three times as many women as males are affected by the illness. Researchers think that certain women may get the condition as a result of hormonal and reproductive factors.
- Genetics and family history. You could be more susceptible to RA if the condition runs in your family. The risk of having RA is somewhat increased by several hereditary factors.
- Smoking. Long-term smokers had a higher risk of developing rheumatoid arthritis, according to studies.
- Being overweight. Some study suggests that obesity may restrict the amount of treatment available for the condition while simultaneously increasing the risk of acquiring it.
- Periodontal disease. RA risk may be elevated by gum disease.
- Lung conditions. Arthritis can also occur as a result of lung and airway diseases.
Osteoarthritis
Osteoarthritis may affect anyone. The risk of developing osteoarthritis is higher in adults over 55 and those going through menopause.
Osteoarthritis is more common in people with certain medical conditions.
- Overweight.
- Diabetes.
- High cholesterol.
- The joints are harmed by some autoimmune diseases.
- Age. Age is the most significant risk factor. As people age, their cartilage gradually deteriorates, making them more susceptible to osteoarthritis.
- Genetics. Your risk is significantly increased if you have a family history of OA, which suggests a genetic predisposition.
- Joint injury: Damage to the ligaments, rips, or fractures can all deteriorate cartilage and increase the risk of osteoarthritis in that specific joint.
- Repetitive stress: Over time, OA may develop as a result of occupations or activities that call for repetitive motions or incorrect loads on certain joints.
- Being overweight. Obesity accelerates the deterioration of cartilage and the onset of osteoarthritis by increasing stress on weight-bearing joints like the knees and hips.
- Weak muscles: Joints that have weak muscles around them are less stable and more vulnerable to arthritis and damage.
- Bone deformities: Uneven joint strain caused by abnormalities in bone alignment or structure can lead to osteoarthritis (OA). Gout and rheumatoid arthritis are two illnesses that can harm joints and increase the chance of osteoarthritis.
- Sex: Osteoarthritis is statistically more common in women than in men, particularly after menopause.
- Occupation: Individuals with professions that include heavy lifting, prolonged kneeling, or both are at a higher risk of developing osteoarthritis (OA) in certain joints.
- Nutritional deficiencies: Low calcium and vitamin D levels can weaken bones and indirectly cause osteoarthritis to develop.
Complications of Rheumatoid Arthritis and Osteoarthritis:
Rheumatoid Arthritis
Having rheumatoid arthritis increases the risk of:
Osteoporosis. You may be more susceptible to osteoporosis, a disorder that weakens bones and increases their susceptibility to fracture if you have rheumatoid arthritis and are aware of the drugs used to treat it.
Rheumatoid nodules. Usually, pressure points like the elbows are where these stiff tissue lumps form. These nodules, however, can develop in the heart, lungs, or any other part of the body.
Dry mouth and eyes. Sjogren’s syndrome, which results in a lack of moisture in the lips and eyes, is more common in those with rheumatoid arthritis.
Infections. Rheumatoid arthritis, as well as many of the medicines used to treat it, can impair the immune system, increasing the risk of infection. Vaccines can help prevent diseases including influenza, pneumonia, shingles, and COVID-19.
Abnormal body composition. People with rheumatoid arthritis usually have a higher fat-to-lean mass ratio, even if their BMI is normal.
Lung disease. People with rheumatoid arthritis are more prone to lung tissue inflammation and scarring, which can cause shortness of breath over time.
Lymphoma. Lymphoma, a kind of blood cancer that is more frequent in patients with rheumatoid arthritis, originates in the lymphatic system.
Osteoarthritis
Crystals may form in the joints as a result of the cartilage alterations caused by osteoarthritis. These might be:
- Gout attacks can be triggered by crystals of sodium urate. The most often impacted joint is the big toe.
- Crystals of calcium pyrophosphate (CPP) can cause edema and severe pain. Although they can occur in any joint, CPP crystals are more prevalent in joints who already have osteoarthritis.
- The most frequent side effects of osteoarthritis are pain and stiffness, which can vary in intensity. The soreness may be continual or inconsistent, making it difficult to move your joints.
- Reduced mobility: OA might make it challenging to get out of bed, move, or climb stairs. This can increase your risk of falling and make you more dependent on others for help with daily tasks.
- Joint damage: Over time, OA may cause damage to your joints’ bone and cartilage. This might result in anomalies like bone spurs, which could make the discomfort worse.
- Additional health problems: Heart disease, depression, and obesity are also potential side effects of OA.
- Osteonecrosis: Bone tissue death is known as osteonecrosis. Osteoarthritis or the use of certain drugs, such as corticosteroids, maybe the reason.
- Baker’s cyst: A fluid-filled sac that forms under the kneecap is called a Baker’s cyst. It might be caused by OA or another illness.
Prognosis:
Rheumatoid arthritis
Rheumatoid arthritis is persistent and progressive. Everyone has several exacerbations and remissions. Within 10 years of being diagnosed with the illness, over half of all patients become incapacitated.
Aside from joint illness, people may suffer from a range of other joint-related disorders that have a significant impact on their quality of life. Each person’s illness progresses differently.
Rheumatoid arthritis is linked to cardiovascular risk factors, infections, respiratory disorders, and the development of cancer. Patients with rheumatoid arthritis are 2-3 times more likely to die than the general population.
Osteoarthritis
The prognosis for people with OA varies according to the affected joint. Patients with bilateral knee OA deteriorate quicker than those with fewer joints affected. Patients with several medical conditions (heart and lung) are more likely to experience lower extremity impairment than those with simply knee arthritis.
Medication does not slow the course of OA, but it can enhance the patient’s quality of life by relieving pain. Physiotherapy can help to detect and adapt joint-stressing activities, as well as alleviate osteoarthritis symptoms.
FAQs
What activities should be avoided if you have osteoarthritis?
Repetitive movements. Repetitive movements may exacerbate the damage to joints already caused by osteoarthritis. These movements might be caused by either work or leisure activities. If some tasks cannot be avoided, it is critical to rest frequently and adopt good form.
What are the top 10 foods to avoid if you have osteoarthritis?
Foods to Avoid with Arthritis: Added sugars. Everyone, including those with arthritis, can benefit from reducing their sugar intake.
Processed and red meat.
Foods with gluten.
High-processed meals include some vegetable oils.
Salty foods.
Foods having high AGE levels.
What are the top five veggies to avoid for arthritis?
Some persons with arthritis claim that nightshade foods such as tomatoes, potatoes, eggplants, and peppers irritate their disease. While there is no evidence to support a relationship between arthritic pain and most nightshades, tomatoes may be an exception. This is because they raise the amount of uric acid.
Is egg good for osteoarthritis?
On the contrary, eggs have been shown to possess compounds with anti-inflammatory properties. Most individuals, including those with arthritis, are encouraged to eat two eggs each week as part of a healthy diet.
Rheumatoid arthritis persists for how long?
A flare might persist for a few hours, weeks, or even longer. For some people, medications can help prevent attacks and keep symptoms from worsening. Medications and home remedies can help control symptoms during a flare.
Is rheumatoid arthritis a dangerous condition?
Rheumatoid arthritis (RA) causes a variety of physical and social consequences, including a lower quality of life. It can cause discomfort, disability, and early death. Premature heart disease.
What is the first stage of rheumatoid arthritis?
In stage 1, there is inflammation within the joint. The tissue within the joint swells. For example, stage 1 RA in the hands can cause stiffness and pain in the fingers and knuckles. These feelings often fade with movement.
What is the most effective therapy for rheumatoid arthritis?
Workouts and relaxation methods might help you reduce pain while also keeping you occupied. Communicate effectively with your healthcare team to gain control over your illness. Get assistance managing the physical, emotional, and mental symptoms of rheumatoid arthritis.
Why does it feel to have rheumatoid arthritis?
Swelling, warmth, and redness.
Rheumatoid arthritis causes inflammation of the lining of joints, causing them to swell, feel hot, and be sensitive to touch. Rheumatoid nodules, or hard swellings under the skin, can form around injured joints in certain patients.
Can I function normally with rheumatoid arthritis?
Many people with RA may live healthy, active lifestyles. For example, disease-modifying antirheumatic drugs (DMARDs) have emerged as an effective and widely available therapy for RA. These drugs work by inhibiting the immune system and reducing the damage they inflict on joint tissue.
What is the fastest method of treating arthritis?
The following measures can often reduce arthritic symptoms:
Weight loss with exercise.
Hot and cold therapy. Heating pads and ice packs might assist in alleviating arthritis pain.
Assistive devices.
References
- Admin. (2020, December 2). Osteoarthritis vs Rheumatoid Arthritis. Madhu Thumu. https://drmadhuthumu.com/osteoarthritis-vs-rheumatoid-arthritis/
- Tadvi, D. (2024, February 9). Osteoarthritis – cause, symptoms, treatment, exercise. Physical Therapy Treatment and Exercise. https://physical-therapy.us/osteoarthritis/
- Tadvi, D. (2025, March 9). Rheumatoid arthritis – Causes, symptoms, treatment. Physical Therapy Treatment and Exercise. https://physical-therapy.us/rheumatoid-arthritis/#Self_Care
- Comparing RA and OA. (n.d.). WebMD. https://www.webmd.com/rheumatoid-arthritis/rheumatoid-arthritis-osteoarthritis-difference