Clubfoot (Congenital Talipes Equino Varus – CTEV)
What is a Clubfoot (Congenital Talipes Equino Varus – CTEV)?
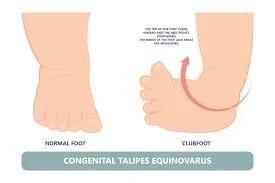
Congenital Talipes Equinovarus, another name for clubfoot, is a complicated congenital foot deformity that, if left untreated, can make walking uncomfortable and difficult for a person. It is described as a malformation involving soft and bone tissues in the forefoot, midfoot, and hindfoot that is complicated and malaligned.
The deformity affects the shape and positioning of the foot, manifesting as a varus hindfoot and adducts and cavus (an inward twisting) of the midfoot. The foot is kept in a fixed equinus, or downward pointing posture, at the subtalar joint.
In comparison to a typical, unaffected foot, the foot affected by clubfoot is shorter and has a smaller calf circumference. The clubfoot deformity shows variable degrees of stiffness at presentation and is not passively correctable.
Clubfoot can occur bilaterally (60–70%) or unilaterally (30–40%). In men compared to women, it is twice as prevalent. It is the most prevalent congenital foot deformity, affecting 1-2 babies out of every 1000. Though it is seldom linked to other congenital disorders or syndromes, it is often an independent anomaly.
Here is where Talipes Equinovarus originates:
- “Pes” indicates foot.
- “Tali” indicates ankle.
- Foot pointing down, like a horse’s foot, is called ” equinus”.
- Deviation towards the midline is called ”varus”.
Clubfoot is a term used to describe a variety of congenital (existing at birth) foot deformities in which the baby’s foot is twisted out of shape or alignment. The tendons that connect the muscles to the bones are shorter than usual in clubfoot. Clubfoot is a somewhat common birth abnormality that typically affects a single, otherwise healthy infant.
You may have moderate or severe clubfoot.
Approximately 50% of kids who have clubfoot also have it on both feet. Doctors advise treating clubfoot as soon as possible after delivery since it will make it more difficult for the child to walk normally.
Clubfoot can occur on one or both sides (30%–40%) or 60%–70%.
In men compared to women, it is twice as common.
It is the most common congenital foot deformity, affecting 1-2 babies out of every 1000. It is usually a solitary defect, although occasionally it is associated with other congenital disorders or deformities.
The talipes equinovarus deformity is another name for it.
Global Burden of Clubfoot
Insufficient treatment or management of clubfoot can lead to a serious deformity that limits participation in daily activities for the rest of one’s life.
The kit will bear weight through the soles or sides of their feet as they become larger and start to walk on them. The weight-bearing portion of the foot develops a thicker callus, causing discomfort and making the foot vulnerable to infection and damage.
When this occurs in an adult, it typically means that the person cannot wear regular shoes and that, by the time they are in their 20s or 30s, they have significant walking limitations and an obvious foot deformity. This therefore frequently results in prejudice and makes it difficult for the person to get work or an education, which further reduces their ability to make an economic contribution that may have an influence on their family members as well as themselves.
Eighty percent of clubfoot cases are thought to occur in low- and middle-income countries. Due to a lack of finances and access to healthcare, congenital conditions like clubfoot, which may be curable, cause a significant degree of impairment in these nations. In low- and middle-income countries, many newborns with clubfoot do not receive any treatment.
When a kid with clubfoot ultimately starts to walk, the deformity eventually becomes a “Neglected Clubfoot” if left untreated. The child’s foot posture causes them to bear weight across the lateral and dorsal sides of the affected foot, resulting in the formation of a large bursa and callous.
The deformity gets worse when the kid walks, causing more stretching of the soft and bone structures, which causes discomfort and decreased mobility. The effects of clubfoot deformity can significantly affect a person’s life. Girls with clubfoot may be less likely to marry in some nations,
while in others, some social groups believe that deformity is the consequence of a curse. In areas where agriculture is the primary source of income and there is no transportation infrastructure, being immobilized may be highly incapacitating.
Clubfoot treatment in low- and middle-income countries is difficult; the sheer number of kids and adults with untreated clubfoot that surgeons have seen while visiting these regions is a good indicator of the scope of the issue. Regarding the state of clubfoot services in most low- and middle-income countries, not much information is accessible. It has been observed, nonetheless, that similar to Brazil, the kite is offered as a medicinal substitute in a number of countries (Lourenco, 2007).
Others, like Malawi, had almost no clubfoot services available before 2007 and no uniform, national clubfoot management strategy. Parents frequently choose not to seek treatment for their children owing to a lack of resources and the perception that clubfoot is untreatable or a result of fate.
Epidemiology
With a male-to-female ratio of 2.5 to 2.8, clubfoot is more frequent in males. Across nations and areas, different occurrences have been reported, ranging from 1–1.50 per 1000 live births to 3 per 1000 live births.
Ethnic disparities in prevalence have also been documented, with the Polynesian Region having the greatest frequency (6.8%) and the Chinese population having the lowest incidence (0.6%). Among Caucasians, the cumulative incidence is around 1 per 1000 live births. 80% of clubfoot babies born worldwide are born in low- and middle-income nations.
Causes of Clubfoot
About 80% of instances of clubfoot are idiopathic. The remaining 20% are associated with various conditions, most often cerebral palsy, arthrogryposis, and spina bifida. Clubfoot prevalence varies worldwide, with estimates for Chinese people at 0.39/1000 live births, Caucasians at 1 -2/1000, and Polynesians at 7-8/1000. In LMICs, birth prevalence has been observed to range from 0.51 to 2.03/1000 live births.
Clubfoot is poorly known to have several causes. Environmental variables, seasonal fluctuation, and in-utero positioning have all been proposed as potential causative factors, although they have not been consistently proven. There is most likely a genetic component as well. Many countries and communities have differing opinions regarding the cause of congenital clubfoot.
These include sorcerous influences, spells, or curses, which frequently result in mothers being held accountable for the malformation. It is crucial to convey to families that children with clubfoot are invaluable members of the community since these misconceptions may lead to the child’s exclusion from society.
Several theories, taking into account both extrinsic and intrinsic factors, have been put forth to explain the genesis of clubfoot. These include the fetus’s intrauterine position, mechanical compression or elevated hydraulic pressure, disruptions in fetal development, viral infections, vascular deficiencies, muscular abnormalities, neurological abnormalities, defects in the development of the bones’ structures, and genetic defects.
Researchers think that environmental factors and genetics have a role.
While the specific cause of structural CTEV is unknown, environmental factors and genetics may have a role. Postural CTEV, on the other hand, may arise from packing disorder, a condition in which a firstborn child weighs more than 4 kg at birth and has less fluid surrounding him or her in the womb
It is believed that clubfoot is idiopathic in 80% of instances.
The remaining 20% commonly coexists with other conditions, such as arthrogryposis, cerebral palsy, and spina bifida. Clubfoot incidence varies globally, with estimates for Chinese people at 0.39/1000 live births, Caucasians at 1-2/1000, and Polynesians at 7-8/1000.
It has been found that among LMICs, birth generality varies between 0.51 and 2.03/1000 live births.
The understanding of clubfoot’s cause is lacking.
Environmental effects, seasonal changes, and in-utero placement have all been suggested as potential cause factors, but they have not been consistently established. There is most likely a genetic component as well.
There are different opinions regarding what causes a person to have clubfoot from birth in several cultures and areas.
These include sorcery, spells, or curses; often, mothers are held responsible for the deformity.
Families should be informed that children with clubfoot play a vital role in society, since these misconceptions may lead to the infant being kept out of society.
Who is at risk for congenital clubfoot?
The likelihood of boys developing clubfoot is up to double that of females. The infant is also more vulnerable if there is a family history of clubfoot.
The children are more susceptible if they have:
Some additional birth abnormalities, such as cerebral palsy or spina bifida.
an inherited illness like Edward syndrome (trisomy 18).
If a mother has a condition known during her pregnancy, her child may be more likely to have clubfoot.
This is an issue with inadequate amniotic fluid, the fluid surrounding the fetus, and Zika infection during pregnancy, which can result in birth abnormalities and other issues.
Smoked, drank alcohol, or used illicit substances when they were expecting.
Although reported, the following suggestions have not been validated and should not be taken seriously as actual causes:
- Neurogenic Theory: Clinically apparent muscular weakness may be caused by a reduced motor unit, which is included in the common peroneal nerve distribution.
- Myogenic Theory: This theory is supported by the existence of abnormal muscles that can cause equinovarus deformities, such as the accessory soleus muscle and the flexor digitorum accessories longus muscle.
- Vascular Theory: Blood flow in the anterior tibial artery and its offshoots is diminished.
- Embryonic Theory: A developmental abnormality that can appear up to 12 weeks after conception.
- Chromosomal Theory: Unfertilized germ cells may contain certain chromosomal abnormalities.
- Osteogenic Theory: A 7–8 week embryo has a transient stop of development for an unidentified reason, which may result in clubfoot or other abnormalities.
- Mechanical Block Theory: A mechanical obstruction that develops during the intrauterine development stage, such as intrauterine fibrotic bands, inadequate amniotic fluid, an uneven uterine cavity, etc., may give birth to Talipes equinovarus.
Clinically Relevant Anatomy & Clinical Presentation
There are 26 bones in the foot. In relation to this congenital malformation, the Talus, Calcaneus, and Navicular are most significant. The easiest way to comprehend the underlying abnormality of clubfoot is to break it down into four parts, the initials of which stand for the word CAVE.
These constituents are Equinus, Varus, Adductus, and Cavus. The midfoot is affected by the Cavus and Adductus abnormalities, whereas the hindfoot is affected by the Varus and Equinus deformities.
The initial component of the clubfoot deformity is the cavus in the midfoot. The foot’s arch is higher than usual. due to the plantarflexion of the first metatarsal with respect to the calcaneum and hindfoot.
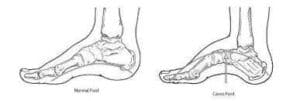
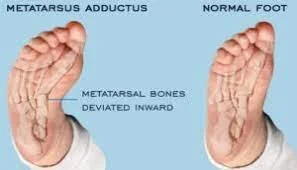
Moving toward the midline is called adducts. The second component of clubfoot deformity is the adducts. Adduction of the forefoot toward the midline occurs. This is the second component of the clubfoot deformity. The navicular dislocates off the talus and moves medially. A component of the adductus deformity is the calcaneum’s medial rotation beneath the talus.
Varus denotes a moving toward the center. The third component of the clubfoot deformity is the varus of the hindfoot. The heel and tibia are positioned in a varus.
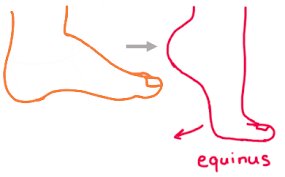
Equinus is a term used to describe a greater plantarflexion of the foot. The whole foot is pointing downhill with respect to the tibia. The fourth component of the clubfoot deformity is hence the equinus of the hindfoot.
The deformity is characterized by adduction and inversion at the subtalar, midtarsal, and anterior tarsal joints in addition to equinus/plantarflexion at the ankle. “Congenital dislocation of the Talo-Calcaneal-Navicular (TCN) Joint” is one way to characterize clubfoot. In clubfoot, the calcaneum rotates beneath the talus while the navicular glides medially on the talus.
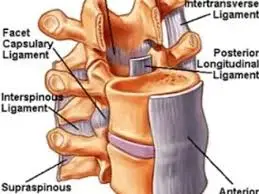
Ligaments and muscles hold the foot in an adduction and inversion position. The flexor digitorum longus, flexor hallucis longus, triceps surae, and tibialis posterior are the muscles that are contracted. Additionally, there is an imbalance between the muscles of the everted dorsiflexor and the inverter-plantar flexor. Typically, the peroneal and calf muscles are underdeveloped. The foot might be inverted due to weak peroneal muscles. The ankle’s posterior and medial ligaments are densely packed.
Classification
Those who treat clubfoot must use the same terminology to differentiate between the various forms because there are differences between them.
Every kind of clubfoot is different and may require a different course of therapy. Early diagnosis of the type of clubfoot a person has can assist in determining the best course of action. Clubfoot cannot be categorized universally; however, it can be categorized based on the type of deformity present.
Positional Clubfoot
A flexible foot that was maintained throughout time in an unusual posture in utero is known as positional clubfoot. Because of the protracted posture, the baby may arrive at birth with one or both feet in an unusual resting position. The forefoot and ankle passive range of motion is usually unlimited in children with positional clubfoot.
There is some deformity in the foot at birth, but the bone alignment remains unaffected, and conservative therapy incorporating weight bearing, range of motion, and stretching is likely what corrects the foot position. After conservative treatment, the foot may require one or two casts in a small percentage of instances to preserve the corrected position; nevertheless, most of the time, these feet correct well and do not result in any serious, long-lasting damage.
Idiopathic Clubfoot
The most prevalent classification for clubfoot is “Idiopathic Clubfoot,” which denotes that the deformity’s origin is unknown. There can also be a clear genetic component to idiopathic clubfoot, meaning that a person’s chances of having clubfoot or passing it on to their offspring are increased (3–10%) if they have a parent, sibling, or relative who has the condition. There is a broad range of disability within the category of idiopathic clubfoot, depending on the severity of the condition and whether it has been well treated, partially treated, badly treated, or left untreated.
The Arica Clubfoot Training explains them as follows:
- Untreated Clubfoot
Untreated clubfeet are those that have had very little or no therapy from infancy until the age of two.
If clubfoot receives insufficient care, it may develop into a severe deformity that renders the patient permanently unable. The child will bear weight through the tops or sides of their feet as they become bigger and start to walk on them. The weight-bearing portion of the foot develops a thicker callus, causing discomfort and making the foot susceptible to infection and damage.
Usually, by the time the individual reaches their 20s or 30s, they will be unable to wear regular shoes and have significant trouble walking. People with clubfoot may face discrimination because of their obvious disability, and they may not be able to get work or education. People who are born with clubfoot may not be able to work and make an economic contribution to society, which has an impact on society overall in addition to being extremely tough for the individual and their family.
- Treated Clubfoot
“Treated clubfeet” refers to untreated clubfoot that has undergone Ponsetti therapy correction. Clubfoot-treated children are often braced nightly until they are 4 or 5 years old and full-time for 3 months.
- Recurrent Clubfoot
Although the Ponsetti therapy for this Clubfoot patient had positive results, the deformity has now returned. Recurrence refers to any or all of the original clubfoot deformity’s components returning following effective therapy. This can occur at any point until bone development is attained, although it is more likely in the first and second years following therapy, particularly if bracing has not been maintained.
The most frequent cause is early braces discontinuation.
- Neglected Clubfoot
When a child older than two years old has neglected clubfoot, little or no therapy has been administered. In addition to responding to Ponsetti treatment, the neglected clubfoot may have a bone deformity that has to be surgically corrected.
- Atypical Clubfoot
This condition, known as clubfoot, is characterized by an extended big toe, a plantarflexed first metatarsal, and frequently swollen feet. While some children are born with atypical clubfoot, we think that some acquire it as a result of mistreatment; this most frequently happens when a cast slips off.
- Complex Clubfoot
Any deformed foot that has been treated in any method other than the Ponseti procedure may have extra complications due to increased disease or surgical scarring.
- Resistant Clubfoot
This case of clubfoot has been correctly treated with Ponseti Treatment, yet no significant improvement has occurred. A common finding is that this particular kind of clubfoot is secondary or syndromic rather than idiopathic.
Secondary Clubfoot
On the other side, secondary clubfoot happens when another illness or disease is connected to or causes the development of clubfoot. These illnesses are either neurological, like spina bifida, which is linked to simultaneous sensory and/or motor deficits, or syndromic disorders, like arthritis, which are linked to more widespread symptoms and the involvement of other musculoskeletal problems.
Signs and Symptoms of CTEV
Here are some signs to watch out for to determine whether your child has CTEV:
- Inward turn of the feet
- Calf muscle tightness Minimal range of motion in the foot joints in infants with structural CTEV
The heel turns inward when the upper parts of the foot are typically bending downward or inward.
Because the patient’s feet’s calf muscles are undeveloped, they seem somewhat shorter.
Extra-tight Achilles tendons, often known as heel cords, can also be present in children with deformed feet.
Parents should exercise particular caution because there is no pain or suffering associated with this disease.
Parents need to keep track of the modifications in their kids’ foot motions and share this information with physical therapists.
Diagnosis
Clubfoot is often diagnosed during pregnancy, during an ultrasound, or at delivery. Once the foot is born, it is examined by gently examining it to determine whether it can be reverted to its usual position. If not, clubfoot has been positively diagnosed.
Assessment
It’s important to perform a thorough evaluation when a child with clubfoot initially appears to rule out any further neuromuscular problems. This should include of:
- Hands and upper limbs for deformities, tone, and range of motion
Check the neck, head, and face for any indications of a syndrome or torticollis symptoms. - Complete examination of the child’s spine (in a prone position) for any anomalies, including spina bifida
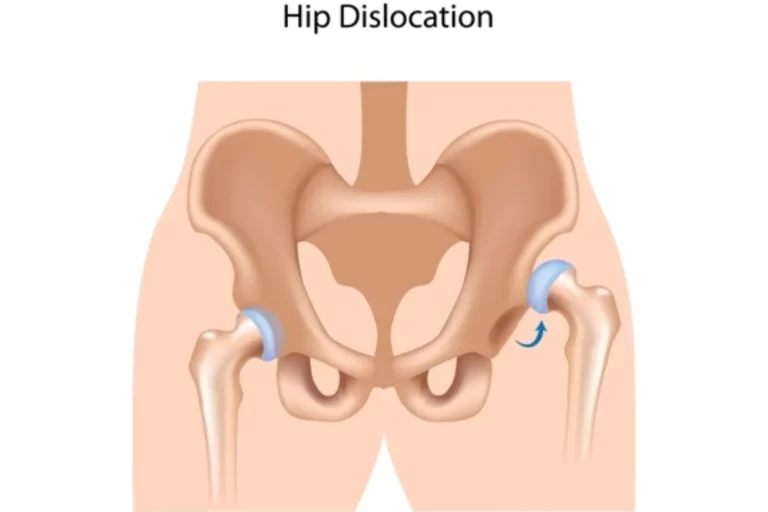
- the hips for any indication of hip dysplasia development
Leg length, range of motion, tone, and deformity in both lower limbs
Treatment/Management of Clubfoot
There have been many various approaches to treating clubfoot, but since the 1970s, the Ponseti Method of therapy has gained favor and, in many countries, has entirely supplanted the earlier approaches, which combined conservative and surgical therapies. The Corrective Phase and the Maintenance Phase are the two equally significant phases of the Ponseti Method.
Conservative Methods
There are many different treatment approaches available, but Ponseti’s, Kite’s, and the French approaches seem to be the most well-known.
Ponseti’s Method
It has been demonstrated that the Ponseti Method, which was created in 1963 by Dr. Ponseti, an orthopedic surgeon located at the University of Iowa, is a safer and more effective therapy for clubfoot than surgery. The Ponseti technique is the most effective in treating idiopathic clubfoot patients. Published in 1995, the first long-term research of the Ponseti Technique’s results contributed to the technique’s worldwide popularization.
This method involves a highly particular set of casts and manipulations to rectify the deformity of the foot and, in most cases, to complete the tenotomy of the Achilles tendon to eradicate the equinus deformity. The patient then spends an additional three weeks in a cast.
The patient is then required to wear a foot abduction orthosis, which is a pair of boots adjusted in dorsiflexion and abduction on an immovable bar, nightly for at least four months after the first three-month period. When applied appropriately, the Ponseti Method’s outcomes can, in up to 98% of cases, result in the complete repair of the clubfoot deformity. A long-term follow-up after about 30 years revealed fantastic treatment outcomes, with 78% of clubfoot patients demonstrating “excellent or good” foot function compared to 85% of matched people without congenital foot abnormalities. Due to these results, the Ponseti Method is now the preferred course of therapy for clubfoot in the majority of high-income nations, according to orthopedic doctors.
Ponseti Approach Treatment Phases:
Corrective Phase:
Using a series of manipulations and plaster of Paris casts, the foot posture is gradually adjusted throughout the corrective phase. Ultimately, a minor outpatient operation called a tenotomy is used to cut the Achilles tendon. The infant is visited once a week for therapy during the 4–8-week correction phase.
Maintenance Phase
The goal of the maintenance phase is to maintain the corrected position for the following four to five years after the corrective phase has successfully placed the foot in a favorable position. This is because the foot has a tendency to revert to its deformed posture. This is accomplished by placing the child’s feet in a brace for the first twelve weeks, twenty-three hours a day. then till 4-5 years old at night.
When compared to many therapies for identical conditions, the complete course of treatment can cost as low as $150 USD. This is quite affordable. For this reason, a lot of health ministries, non-governmental organizations, and other stakeholders consider Ponseti therapy to be valuable as an early intervention to help prevent avoidable impairment.
The Ponseti Method is a simple, cost-effective treatment that is currently being used all over the world. More than 90% of baby instances with idiopathic clubfoot have been successfully treated with the Ponseti operation, according to several studies carried out in different countries over the past 20 years. The Ponseti Method is presently the suggested treatment for clubfoot because of its growing body of evidence and efficacy.
The goals of the therapy are as follows: should be able to wear regular shoes and have pain-free, functioning feet in order to avoid permanent damage.
There are main messages to remember from the Ponsetti Management of Clubfoot:
- Assess, Plan, and Manage
- Consult with Parents Right Away (Especially Regarding Braces!)
- Prioritize accuracy before keeping accuracy in the cavus.
- Never touch the heel.
- TWO Individuals to Wear
- Toe to Groin Casts
- Most of the time, tenotomy is necessary.
- Before a tenotomy, cover the talus.
- Continue Talking with Parents: Proper adherence to bracing is essential to sustaining correction!
Exercise Stages After Ponseti Method
Stage 1
Bar and Boots Full Time. The infant will thereafter spend twenty-three hours a day in the boots and bar. The last cast is taken out. During the hour your child is not wearing their brace, we advise you to work out with them. Stretching is becoming accepted as a powerful component of the therapeutic process, even though it was not included in Dr. Ponseti’s initial regimen. By preserving the correction made possible by casting and tenotomy, stretching may assist the child in keeping their foot supple.
- Massaging the Foot
Following the removal of the cast, the infant’s foot may feel tender to the touch.
You should use lotion or cream to gently massage the child’s foot for the duration of the hour that they are not wearing the boots and bar.
Use a variety of techniques (such as tapping, and tickling) and materials (such as cotton balls, and washcloths) to massage the foot.
This will aid in the foot’s sensitization.
- Stimulating the Muscles
The baby’s foot pulls inward and downward more strongly than it pulls outward and upward because of the original clubfoot abnormality.
Stimulate the baby’s foot’s outside edge to assist balance the power of these muscles, and watch it fan out and upward!
- Stretching within Abduction and Dorsiflexion
When the child is walking, extend their foot out (abduction) and up (dorsiflexion).
Spends time away from the bar and boots.
Consider the last cast gaze and attempt to extend the foot to the same length.
Five times through, hold the stretch for thirty seconds.
- Stretching Into Plantar Flexion (Down)
The length of time the infant needs to wear a cast to cure the clubfoot deformity may cause the muscles on the front of the baby’s ankle to become tense. These muscles need to be stretched in order for your child to be able to adopt a fully toe-down foot posture.
Stretch the child’s ankle by placing one thumb over the midfoot and the other across the child’s lower shin, right above the ankle joint.
The child’s foot should be stretched into a toe-down position by applying pressure. Five times over, hold the stretch for 20 seconds.
You must schedule an appointment as soon as possible with the clinic if the infant is persistently removing their foot from the boot or if they have a sore.
Please try reapplying the boots and bar until the appointment if the infant does not have a sore or if it is not getting worse.
Stage 2
putting on the bar and boots at night and when taking rests. Following three months of continuous use, the child will advance to the stage of sleeping through the night. You should keep up the strengthening and stretching activities that will benefit the child’s developing feet. To prevent your child’s foot from being stiff or regressing to its original look, stretch their foot three times a day and schedule an appointment at the clinic as soon as you can.
- Stretching the Achilles Tendon
Hold your child’s heel in the palm of your hand while their knee is straight.
With the other hand, press up on the midfoot and pull down on the heel (being cautious not to push up on the toes).
Five repetitions of the 20-second hold are required.
- Playing in a Squat Position
Teach the child to play in a squat position with both heels flat on the ground once they are able to walk.
This pose maintains the flexibility of the ankles and feet while stretching the calf muscles.
Encourage the child to walk like a bear, waddle like a duck, and jump like a frog as they become older!
- Strengthening the Muscles
The muscles that lift the foot up and out must be strengthened as the child develops.
Asking the child to use his or her toes to contact your finger as you place it at the outside border of the foot can help to engage these muscles.
Alternative Exercises
- Playing in a sandbox or a plastic tub with sand in the bottom is another approach to building muscle.
- Place the baby’s heel in the sand and use the foot to push the sand away from the body.
- With this motion, the child may create sand mounds that they can later trample over! Drawing drawings in the sand with the foot is also a lot of fun.
- Using a windshield-wiper motion and large outward foot motions, the toddler may draw rainbows.
- As the child makes these motions, ask them to attempt to maintain their heel in the sand.
- As a child gets older, he or she could engage in additional strengthening activities including walking on the inside of the foot and on heels.
- Encourage your child to make letters in the air with their foot once they have mastered the alphabet!
Kite’s Method
In the orthopedic community, this conservative strategy of treating clubfoot is no longer often utilized or accepted. In the 1930s, Dr. Kite created the Kite technique in the United States. After he became disappointed with the unsatisfactory results of surgical therapy and the sometimes painful outcomes after forced manipulations of clubfoot deformity using the then-popular Thomas Wrench, Kite set out to establish a non-invasive treatment technique for clubfoot.
Treatment with Kite’s Method involves a series of casts and manipulations, and then night splinting with the feet slightly abducted and kept in dorsiflexion.
In 800 cases of clubfoot, Kite reported successful outcomes using non-invasive therapy. Further investigations were unable to replicate these results however up to 90% of children treated with the Kite approach required further soft tissue releases by surgery. These disappointing results were ascribed to two primary factors: the use of short leg (below the knee) casts, which are insufficient to retain the right position of the foot, and the anatomically incorrect way of manipulating the foot, which inhibits the deformity from resolving. It can take up to two years for the deformity to be rectified using the Kite approach, which also calls for a large number of casts.
The French Method
The French Functional (Physical Therapy) Method is a less often used approach for which there is a considerably less body of research data. Users may wish to be aware of this as well.
The French Method involves immobilizing the foot with nonelastic adhesive strapping, stimulating the muscles working on the foot to sustain the reduction obtained by manipulation, and manipulating the infant’s clubfoot on a regular basis. Typically, treatment lasts for around two months before being progressively tapered off. In general, improvement happens over the first three months and happens more slowly than with the Ponseti Method.
After an average follow-up of 51.4 months, Richards et al. (2008) compared the Ponseti and French Methods and discovered that, though the outcomes were quite similar, foot handled with the Ponseti Method showed a trend towards a superior clinical outcome compared to those managed with the French Method (p = 0.31). Results for the Ponseti Method were rated as “Good” by 72% of participants, “Fair” by 12%, and “Poor” by 16%; in contrast, the French Method yielded ratings of 67%, 17%, and 16%, respectively. According to the authors, this could have been because it took a significant amount of work to teach the parents the procedure and get them to consistently do it—that is, stretch, tape, and splint every day for up to two years.
Surgical Intervention
As many as 45% of patients treated with various forms of soft tissue release observed favorable results from the early surgical therapy of clubfoot in the late 1800s. During the 1980s and 1990s, surgical methods were the preferred course of therapy after regaining favor in the 1970s. Many of these methods involved a significant relaxation of the soft tissues in the foot, similar to posteromedial release (PMR). Turco, whose work had a significant impact on the development of surgical procedures, said that 83% of patients at follow-up, which occurred between two and fifteen years after the first treatment, showed that his PMR approach had excellent or good outcomes.
However, ten years following surgical release therapy, patients had significant degrees of foot and ankle stiffness and weakness, according to several long-term follow-up investigations, especially Aronson & Puskarich (1990). The majority of orthopedic physicians currently hold the opinion that clubfoot is best treated non-invasively at first, which is supported by this and other data.
Surgery
- Achilles tendon Lengthening
- Tendon Transfer
- Reconstructive Surgery
What are the risks of clubfoot surgery?
Congenital clubfoot surgery has the following risks:
- nerve damage.
- infection.
- bleeding.
- stiffness.
Some At-Home Exercises for Treating Clubfoot.
The baby’s clubfoot can be treated at home with a few easy exercises that the doctor might recommend. They are as follows:
- Metatarsus Adduction (stretching instep out)
Place the left hand on the inner of the infant’s foot to begin this practice.
Stretch the front of the foot, including the toes, progressively downward and away from the heel by placing the fingers of your right hand between your toes.
Return it to its original place after holding it for ten to fifteen seconds.
- Plantarflexion of the ankle (foot downward)
Use your left hand to grip the baby’s heel and ankle as you complete this exercise. Raise your right hand above your foot.
With the left hand holding the heel in place, slowly press the midfoot and toes down with the right palm.
- Ankle Dorsiflexion (foot goes up)
Using your right hand, grip the baby’s heel to complete this exercise. With that hand, slowly pull the calf muscles down. Position the left hand in the center of the rear of the infant’s foot and gently press it in the direction of the heel.
- Toe Stretches
For this exercise, have the infant lie down and gradually lift each toe individually, maintaining a 90-degree angle at the heel and ankle.
Strengthening Exercises
Touch the infant’s toes, calf, and rear of the foot gently to tone up their muscles. In response, the infant will raise his leg and extend his muscles.
Ten times over, repeat that.
AFO For Clubfoot
The Clubfoot AFO is composed of a molded Duraflex inner boot with dorsum pinch cushions and a solid ankle AFO constructed of thin copolymer thermoplastic. The end product is a beautifully customized fit that offers strength, durability, and comfort.

A custom-made brace called the Clubfoot AFO is perfect for kids with idiopathic or non-idiopathic clubfoot. Children whose feet might not fit properly into a shoe or sandal brace benefit most from this AFO. This includes kids with idiopathic clubfeet, meningomyelocele, or syndromes, which cause their feet to be small and boxy, making it harder for them to wear sandals or shoes.
It is planned to utilize the Clubfoot AFO for both atypical/complex and conventional instances of clubfoot. In comparison to other clubfoot braces, our AFO is made to provide superior ankle and foot control while also being more comfortable. Hospitals like St. Louis Children’s Hospital are now employing this brace solely for all instances of clubfoot treated with the Ponseti approach due to its extraordinary performance and excellent parent response.
Evidence
In comparison to other “non-Ponseti” techniques, Ponseti’s Method reduces the number of surgical procedures needed, according to a recent meta-analysis of nine relevant research. When employing Kite’s approach instead of Ponseti’s, a considerably greater risk of poor-to-fair outcomes, relapses, and the need for major surgery was shown by analysis of the pooled odds ratios; however, no significant difference was found when comparing Ponseti’s way to the French method.
According to the current meta-analysis, Ponseti’s approach prevented major surgery across several institutions in 84.9% of patients, was successful in 75.6% of patients, and resulted in a good-to-excellent functional prognosis in 91.1% of patients.
Prognosis
When therapy starts may have an impact on the prognosis. Early intervention increases the likelihood of effective therapy and comparatively “normal” foot function once the kid starts bearing weight. By avoiding recurrence, continued use of the Foot Abduction Brace also improves prognosis. With the Ponseti procedure, some older children may have partial or even complete correction. In certain cases, complete correction of the foot posture may need surgery in addition to a period of casting based on the Ponseti principles.
Outcome Measures
The Pirani score system is the most often used outcome metric. The severity of the clubfoot deformity and the response to therapy are evaluated using this grading system. In terms of the amount of casts required to repair the foot, it has a predictive value. At least four castings will be used if the score is high—four or above. Three or fewer castings are required if the score is less than four. Every component receives a score of 0.5 for slightly aberrant, 1 for highly abnormal, or 0 for normal. See the Bangla Clubfoot Tool and the Roye Score for additional outcome metrics.
Complications of CTEV
As long as your child can stand and walk, CTEV usually doesn’t pose any problems. Then, he or she can have the following challenges:
- Limited movement
- Abnormal gait
- Foot discomfort brought on by improper foot placement
If the illness is not addressed, it may lead to more severe issues including arthritis, low self-esteem, and big calluses or blisters on the foot from an irregular stride.
Conclusion
In conclusion, an adult with clubfoot will never have regular feet. Adulthood will see an increase in the severity of outcomes that were evident at the end of development; under-correction is simpler to address than overcorrection.
As a parent, you can be unsure about what to do if you discover that your unborn child or the fetus has anything unexpected. Throughout your whole pregnancy, you’ve been picturing your kid wearing beautiful clothes rather than having them wear braces, splints, or casts. However, clubfoot is a rather common congenital condition with a very good prognosis. It’s critical to pay close attention to the treatment plan. Success rates rise when this is done. Many kids with clubfoot may run, walk, and even play sports pain-free with the correct care. Consult your child’s physician about the most effective clubfoot treatment plan.
FAQ
What is the main cause of clubfoot?
Most typically, clubfoot first appears at birth. A shortened Achilles tendon, which results in the foot turning in and under, is the cause of clubfoot. In boys, clubfoot is twice as prevalent. Clubfoot correction requires treatment, which typically consists of two stages: casting and bracing.
What are the two types of clubfoot?
The most common type of clubfoot is isolated or idiopathic. It is referred to as isolated clubfoot if your child has it but no other health problems. Idiopathic refers to clubfoot for which the etiology is known. Nonisolated clubfoot: this type of clubfoot occurs in conjunction with other medical disorders.
Is clubfoot a lifelong disability?
However, in the absence of therapy, it can result in a lifetime impairment, including difficulty walking, therefore it’s still regarded as a significant disease. Learn more about clubfoot in newborns and other people by reading on it, along with its causes, treatments, and prognosis.
Is clubfoot 100% curable?
In newborns, idiopathic clubfoot is 95% treatable with casts and stretching. But if kids don’t get this kind of care at a young age, further issues can occur.
Is clubfoot genetic?
Clubfoot most likely runs in families and has a hereditary component. However, the exact gene—or genes—that cause this is still unknown to scientists. The typical downward and inward posture of the foot in all children with club feet is maintained by the tightness of the muscles and tendons around the foot and ankle.
Why is clubfoot common in boys?
With lower risk variants needed for disease manifestation in her male children, the mother’s many risk alleles may account for the high prevalence of clubfoot transmission to sons.
What causes clubfoot in pregnancy?
environment. The risk of clubfoot in the unborn child might be considerably increased by smoking during pregnancy. insufficient amniotic fluid while a woman is pregnant. Clubfoot risk may rise if the baby’s surrounding fluid is depleted in the pregnancy.
References
- Professional, C. C. M. (n.d.). Clubfoot. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16889-clubfoot
- Thakkar, D. (2023, January 4). Clubfoot (Congenital talipes equino Varus) – Samarpan Physio. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/clubfoot-ctev/