Distal Tibiofibular Joint
The distal tibiofibular joint is the articulation between the lower ends of the tibia and fibula, located just above the ankle. It is a fibrous syndesmosis joint, meaning it is connected by strong ligaments, primarily the anterior and posterior tibiofibular ligaments.
This joint provides stability to the ankle, allowing for slight movement to accommodate the talus during foot dorsiflexion and plantarflexion. Proper functioning of this joint is essential for maintaining ankle stability and effective weight transmission through the lower limb.
Introduction
A syndesmosis is a complex fibrous joint with limited range of motion that is made up of two bones connected by ligaments and a strong membrane.
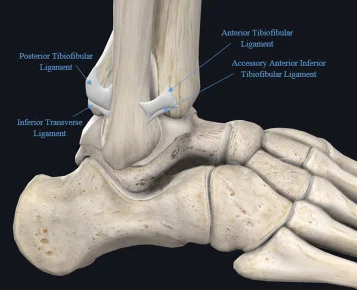
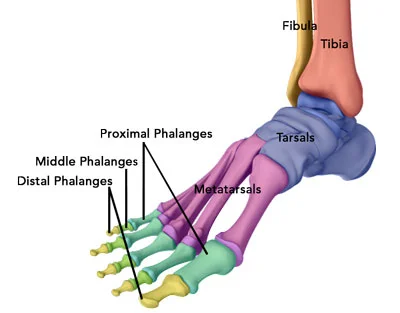
The inferior tibiofibular joint, also known as the distal tibiofibular syndesmosis, is syndesmotic. The interosseous ligament (IOL), anterior-inferior tibiofibular ligament (AITFL), posterior-inferior tibiofibular ligament (PITFL), and transverse tibiofibular ligament (TTFL) attach to this fibrous joint, which is formed between the distal tibia (concave surface) and fibula (convex surface).
In a syndesmosis, two neighboring bones are joined by ligamentous structures, such as a robust interosseous membrane (IOM), to form a fibrous joint. Two bones, the distal tibia and distal fibula, and four stabilizing ligaments—the inferior transverse ligament (ITL), the anterior-inferior and posterior-inferior tibiofibular ligaments (AITFL and PITFL), and the interosseous ligament (IOL), a distal extension of the interosseous membrane—make up the distal tibiofibular syndesmosis. The integrity of the ankle mortise is maintained by the syndesmosis. High ankle sprains, ligament tears, and ankle fractures can all affect the syndesmosis.
Structure and Function
The concave fibular notch of the distal tibia and the convex surface of the distal tip of the fibula interact to form the syndesmotic articulation of the distal tibiofibular joint. For the lower extremities and ankle to function properly, the syndesmosis must be stable.
The anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, inferior transverse ligament, and interosseus ligament are the four connecting ligaments that bind the tibia and fibula together to form the osseous component of the distal tibiofibular syndesmosis.
The distal ligaments of the tibiofibular syndesmosis serve the main purpose of keeping the fibula from moving out of its groove in the tibia, either laterally, anteriorly, or posteriorly. Pathologic external rotational forces that try to laterally/externally rotate the talus are resisted by the ankle syndesmosis, which pushes and displaces the fibula from the tibia.
The anterior-inferior tibiofibular ligament attaches to the anterolateral tubercle of the tibia (Chaput fragment) after emerging from the longitudinal tubercle on the anterior aspect of the lateral malleolus. It keeps the fibula and tibia firmly together and inhibits external talar rotation and excessive fibular displacement.
Attached to the posterior lateral malleolus, the posterior-inferior tibiofibular ligament begins at the posterior tibial tubercle (Volkmann fragment). To keep the tibia and fibula together, it works in tandem with the anterior-inferior tibiofibular ligament. The inferior transverse ligament, which forms a labrum that deepens the articular surface of the tibia posteriorly and contributes to increased joint stability, is located slightly deep in the posterior-inferior tibiofibular ligament.
The tibiofibular mortise is kept from separating too much during ankle dorsiflexion and heel striking by the interosseus ligament, which is located at the distal end of the interosseous membrane and functions as a spring.
Articulating Surfaces
- The articulation between the fibula and the fibular notch of the distal tibia makes up the distal (inferior) tibiofibular joint.
- The joint surfaces are encased in tough, fibrous tissue, a characteristic of a fibrous joint.
Ligaments and joint capsule
The inferior tibiofibular joint lacks an articular capsule and its synovial membrane because it is a fibrous joint. Rather, to enter this joint, the talocrural joint’s synovial membrane protrudes about 4 mm superiorly.
The interosseous ligament, as well as the anterior, posterior, and transverse tibiofibular ligaments, hold the articular surfaces of the distal tibiofibular joint together.
- The interosseous tibiofibular ligament, which runs parallel to the leg’s interosseous membrane, joins the bones’ facing surfaces. It serves as the primary stabilizer of this joint and firmly joins the bones.
- The tibia and fibula’s anterior and posterior surfaces are separated by the anterior and posterior tibiofibular ligaments, respectively. Although both run laterally and inferiorly, the posterior ligament is wider and thicker than the anterior. When the foot moves, these ligaments cover the talus’s trochlear surface in two ways: the anterior during dorsiflexion and the posterior during plantar flexion.
- The posterior tibiofibular ligament is located deep in the inferior transverse ligament. According to numerous authors, it is the deepest portion of the posterior tibiofibular ligament. The yellow ligamentous fibers that make up this structure have a significantly higher number of elastic fibers than the white ligaments found in the majority of the body’s joints. In comparison to other ligaments in this joint, this characteristic makes it much more elastic.
Blood Supply and Lymphatics
The popliteal artery, which branches off from the external iliac artery and femoral artery proximally, supplies blood to the distal leg through the anterior and posterior tibial arteries. However, nothing is known about the blood flow to the actual syndesmotic area. Anatomical differences in the vasculature delivering blood to the front aspect of the tibiofibular syndesmosis have been identified in the published studies on the subject. Various blood supply variations to the anterior syndesmosis have been documented in the literature, including:
- The perforating branch of the peroneal artery is the primary source of these branches.
- Smaller arteries from the tibial artery complement the branches of the peroneal artery.
- The peroneal artery provides fewer branches, while the tibial artery provides the majority of the supply.
There is less fluctuation in the blood flow to the posterior part of the distal tibiofibular syndesmosis. Usually, the peroneal artery is the only source of blood flow to the posterior ligaments of the syndesmosis. Rarely are tibial artery branches added to the local vascular supply.
The lower extremity’s lymphatic vessels are further subdivided into medial and lateral groups by the superficial and deep vessels. The external iliac, lumbar (aortic), popliteal, and deep or superficial inguinal nodes are the destinations of these veins’ drainage.
Nerves
The deep peroneal (fibular) nerve, tibial nerve, and sural nerve are among the nerves in the region of the tibiofibular syndesmosis. The peroneal nerve is a branch of the sciatic nerve that starts at the level of the lower thigh, typically where the sciatic nerve divides into the common tibial and common peroneal nerves.
A superficial branch of the peroneal nerve innervates muscles in the lateral compartment of the leg, while a deep branch innervates muscles in the anterior compartment of the leg and the dorsum of the foot. The deep muscles in the back of the leg are supplied by the tibial nerve, which runs posterior to the tibia.
Embryology
The embryo’s limb buds usually form four to five weeks after fertilization, when the lateral plate mesoderm’s mesenchymal cells become activated and grow. The apical ectodermal ridge (AER), HOX genes, retinoic acid, sonic hedgehog (SHH) genes, and the zone of polarizing activity (ZPA) are among the numerous variables that influence the formation of limb buds.
By thickening the distal ectodermic border, the AER forms and sends signals that cause the mesenchyme of the underlying progress zone to grow rapidly without differentiation, starting the formation of limbs. Synchronous limb outgrowth along the anteroposterior, dorsoventral, and proximodistal axes of growth is the result of retinoic acid’s upregulation of HOX and SHH genes, which starts the production of transcription factors and limb growth.
The lower limbs’ development also involves the expression of the T-box transcription factor Tbx4, which generates the growth factor Fgf10, which acts at the AER to promote mitosis and additional limb growth. The ZPA is a group of cells located on the back of the limb near the AER. As the limb grows, it moves distally with the AER.
Additionally, the ZPA releases retinoic acid, which regulates the limb’s growth and development along the anteroposterior axis. The regional formation of the developing limb and more complex limb polarization result from the promotion of HOX gene expression by SHH and Fgf products. Changes in limb morphology or malformations can result from errors in the expression of the T-box and HOX genes.
Clinical Significance
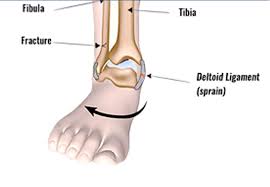
For ankle stability and load transmission during walking and other activities, the tibiofibular syndesmosis is crucial. Thus, in addition to anterolateral ankle pain, individuals with syndesmotic damage often report ankle instability and instability when bearing weight.
The external rotation test and the squeeze test are two frequently used procedures to evaluate syndesmosis during physical examinations. In the external rotation test, the patient sits with the knee bent to 90 degrees and rotates the foot laterally while keeping the ankle locked in neutral.
This test aids in proving that the syndesmotic ligaments are intact. To do the squeeze test, place your thumb on your tibia and your fingers on your fibula in the middle of your lower leg. Then, squeeze your tibia and fibula together. A positive test result is indicated if the test causes pain, which helps detect a fracture.
The most frequent mechanism for tibiofibular syndesmotic injury is external rotation of the talus, which results in excessive fibula-tibia separation and subsequent foot hyper dorsiflexion. A significant portion of physical or sports-related ankle injuries are syndesmotic injuries, which can be challenging to diagnose and have a negative impact on a patient’s functional prognosis.
A longer recovery period and more discomfort are linked to syndesmosis injuries. This is probably because the perforating peroneal artery, which serves as the anterior syndesmosis’s main vascular supply, is susceptible to damage in conjunction with syndesmotic injury. Damage to this vessel would impair adequate blood flow to the injured syndesmosis, which would prolong the healing process.
The restoration of appropriate fibular length and the maintenance of proper position concerning rotation and proximity of the fibula to the tibia are the main objectives in the management of syndesmotic injury. Isolated syndesmotic sprains without diastases or severe ankle instability are usually candidates for non-operative treatment options for syndesmotic injury, which have been reported with generally good outcomes.
A CAM boot or cast with restricted weight-bearing for two to three weeks, followed by a progressive increase in weight-bearing activities until the discomfort is gone, could be part of the treatment. Finally, there is no agreement on the best way to treat syndesmotic damage before, during, or after surgery, and the results mostly depend on a meticulous clinical assessment and management plan tailored to each patient.
FAQs
A distal tibiofibular joint: what is it?
The distal tibiofibular joint syndically articulates between the concave fibular notch of the distal tibia and the convex surface of the distal tip of the fibula. For the ankle and lower extremities to operate properly and dynamically, the syndesmosis must be stable.
What is the distal tibiofibular joint’s articular surface?
Any smooth, avascular, aneural, hypocellular, and lymphatic tissue made of articular cartilage that covers the ends of bones in a joint is referred to as the articular surface. For the bones to move and articulate smoothly, one articular surface is usually convex, and the other is concave.
The distal Tibiofibular joint is made up of which two bones?
The interosseous ligament (IOL), anterior-inferior tibiofibular ligament (AITFL), posterior-inferior tibiofibular ligament (PITFL), and the articular capsule (IOL) support the fibrous joint that is formed between the distal tibia (concave surface) and fibula (convex surface).
Is there cartilage in the distal tibiofibular joint?
An oblique slice at the level of the distal tibiofibular syndesmosis in the anterior (A) and posterior (B) regions. A thin layer of cartilage covers the tibial and fibular facets of the tibiofibular contact zone.
A distal tibiofibular joint is what kind of joint?
The articulation between the fibula and the fibular notch of the distal tibia makes up the distal (inferior) tibiofibular joint. The joint surfaces are encased in tough, fibrous tissue, a characteristic of a fibrous joint.
How does the distal tibiofibular joint move?
There is micromotion in the distal tibiofibular syndesmosis joint. Ankle position and loading patterns were linked to the distal fibula’s mobility about the distal tibia. The clinical management of syndesmotic injuries should consider the syndesmosis’s physiological motion.
What other term would you use to describe the distal tibiofibular joint?
A fibrous joint where two neighboring bones are connected by a robust membrane or ligaments is called a syndesmosis. This idea also applies to the distal tibiofibular syndesmosis, a syndesmotic joint composed of two bones and four ligaments.
What is the distal tibiofibular syndesmosis used for?
A fibrous joint where two neighboring bones are connected by a robust membrane or ligaments is called a syndesmosis. The fundamental purpose of distal tibiofibular syndesmosis is to keep the tibiotalar contact congruent under physiological axial loads.
What is the significance of the distal tibiofibular joint?
The distal ligaments of the tibiofibular syndesmosis serve the main purpose of keeping the fibula from moving out of its groove in the tibia, either laterally, anteriorly, or posteriorly.
What is distal tibiofibular joint diastasis?
Diastasis of the distal tibiofibular joint is caused by external rotation or abduction injuries at the ankle and is linked to significant ligamentous rupture.
What is the most frequent way that the distal tibiofibular syndesmosis is injured?
Syndesmosis damage can be caused by different processes acting alone or in combination. The most prevalent processes are external rotation and hyper dorsiflexion, both separately and especially together. Talar instability and syndesmosis disruption are the results of these conditions, which lead the mortise to enlarge.
References
- TeachMeAnatomy. (2018, October 16). Tibiofibular joints – proximal – distal – interosseous membrane – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/joints/tibiofibular-joints/
- Wikipedia contributors. (2024f, December 12). Inferior tibiofibular joint. Wikipedia. https://en.wikipedia.org/wiki/Inferior_tibiofibular_joint