Inferior Gluteal Nerve
Introduction
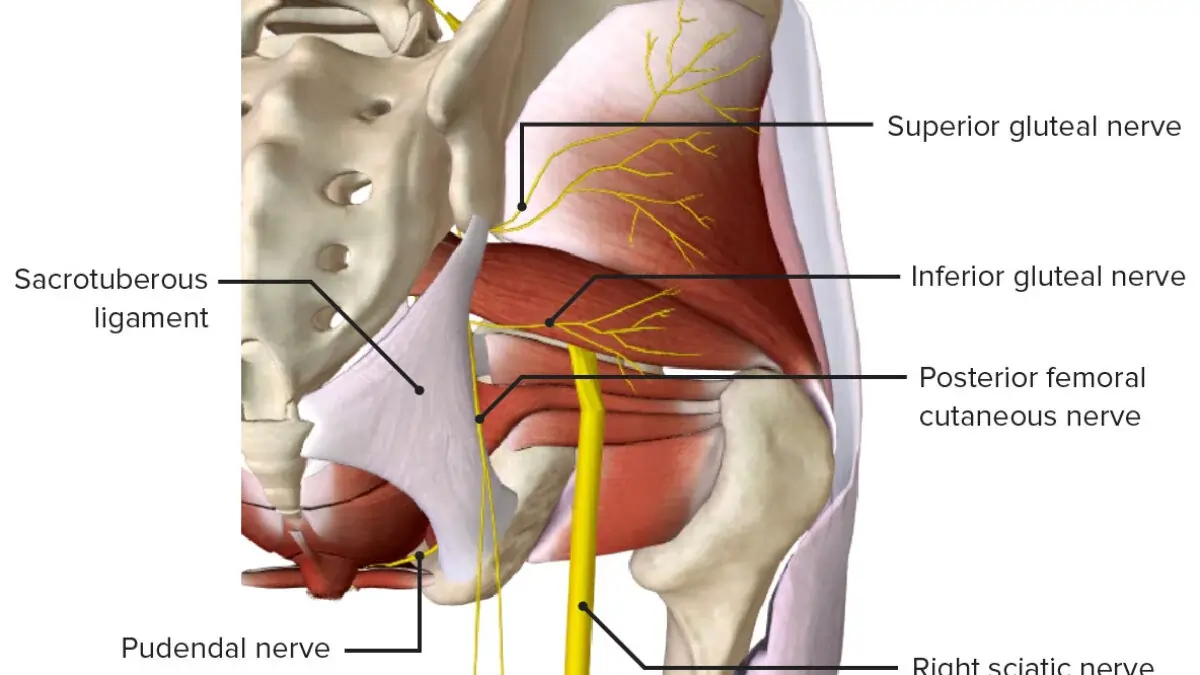
The inferior gluteal nerve is also a motor branch of the sacral plexus, coming from the posterior divisions of the L5, S1, and S2 anterior roots. It flows inferiorly and exits the pelvic cavity via the larger sciatic foramen while going inferiorly to the piriformis muscle.
The gluteus maximus muscle receives motor innervation from the branches of the inferior gluteal nerve.
Structure
The dorsal branches of the ventral rami of the fifth (L5), first (S1), and second (S2) sacral nerves give birth to the inferior gluteal nerve, which supplies the muscle.
The lumbar and sacral plexuses are efficiently connected by the lumbosacral trunk, which is composed of L5 and a minor branch of L4. The sacral plexus is where the lower branches of the L4 and L5 nerves enter.
The lumbosacral trunk, the first through third sacral ventral rami, and a portion of the fourth, with the remaining portion connecting the coccygeal plexus, make up the sacral plexus. In front of the piriformis muscle, the sacral plexus forms in the pelvis.
or femoral cutaneous nerves originate from the sacral plexus, which is created anterior to the piriformis muscle.
However, because they exit the pelvis through the larger sciatic foramen, most sacral plexus nerves are hardly identifiable. A mass of nerves on the piriformis and the anterior main branches of the nerves entering the plexus—the first sacral nerve being a particularly big one—can be identified from the pelvis.
Function
Extending the flexed thigh and aligning it with the trunk is the gluteus maximus’ primary job. In a bipedal walk, it could stop the trunk’s forward motion from causing bending at the supporting hip. When the knee extensors are relaxed, they stabilize the femur on the tibia and are continually active in strong lateral rotation and abduction of the thigh. It is also sporadically active during the walking cycle and stair climbing. Furthermore, the gluteus maximus plays a significant part in some activities, such as standing or running.
A strong extensor of the thigh or trunk when the lower limbs are in a fixed position is the gluteus maximus, a big muscle with many attachments. Another powerful hip stabilizer is the gluteus maximus. It helps to laterally rotate the thigh and expands it at the hip. When the heel strikes, it contracts, stopping hip flexion and starting extension, which slows the trunk’s forward motion. The trunk doesn’t collapse forward because of this action.
Surprisingly, though, the gluteus maximus is not used much when walking, is relaxed when standing, and has little postural significance. It is used for running, climbing, and getting up from a seated or hunched posture. Additionally, it regulates hip flexion when seated.
Course
The larger sciatic foramen is where the inferior gluteal nerve exits the pelvis, going beneath the piriformis muscle. After there, it splits into muscular branches that nourish the gluteus maximus and enter the deep surface of the muscle posteriorly.
The sciatic nerve is superficial to the inferior gluteal nerve. According to some descriptions, it has several branches, and the gluteus maximus above them is innervated.
Very inferiorly, the inferior gluteal nerve penetrated the deep surface of the gluteus maximus. The nerve splits into upward and downward diverging branches at the lower border of the piriformis muscle, and these branches then enter the gluteus maximus. The posterior femoral cutaneous nerve may get a branch from the nerve as well.
The piriformis muscle consistently appeared superior to the inferior gluteal nerve. The nerve’s branching properties may be divided into two major groups. One group consists of small stalks that originated underneath the piriformis and gave rise to all of the nerve’s terminal branches that extended across the gluteus maximus muscle. Four to six branches were growing from the stem. The second kind is characterized by a partial split of the stalk that happens close to the piriformis’s covering. The inferior gluteal nerve had two or three divisions beneath the piriformis, which would split again near where the nerve entered the muscle belly.
When the nerve exited the sacral plexus inferior to the piriformis, it was usually observed medially and near the sciatic nerve. The nerve in each specimen passed through the inferior third of the muscle belly and into the deep surface of the gluteus maximus, around 5 cm from the tip of the greater trochanter of the femur.
The inferior gluteal artery, a branch of the internal iliac artery’s anterior trunk, runs across the inferior gluteal nerve.
It was discovered that the inferior gluteal nerve and artery had an unexpected interaction. However, recent research has shown that there is no reliable correlation between them.
External anatomic markers and the common stalk of the inferior gluteal nerve are related. The targeted area should be positioned at the depth of the posterior border of the proximal femur, medial to the landmark of the ischial tuberosity, and inferior to the most conspicuous part of the greater trochanter. The inferior gluteal nerve’s origin may be consistently reached by triangulating these three positions. When employing electrical stimulation to avoid pressure ulcers, will produce the greatest amount of stimulation of the gluteus maximus muscles.
The larger sciatic foramen, located under the piriformis, is where the sciatic nerve (L4 to S3), the biggest nerve in the body, exits the pelvis right away. Above the piriformis, the superior gluteal nerve travels backward via the larger sciatic foramen, whereas the inferior gluteal nerve travels backward through the same foramen but below it.
Muscle Supply
Returning from a squat and extending the hips and torso are the main functions of this muscle. The gluteal tuberosity of the femur and parts of the iliotibial fascia are where the gluteus maximus muscle inserts itself. Its broad base of origin extends from the posterior surface of the iliac crest to the lateral border of the coccyx, where it fascially attaches to the sacral multifidus and gluteus medius.
When comparing the gluteus maximus muscle during various physical actions, Bartlett and colleagues discovered that sprinting significantly outperformed walking, running, and climbing. When they contrasted this muscle pattern with that of apes, they discovered that humans exhibited more gluteus maximus activation during running with varying insertional patterns, indicating an evolutionary adaptation.
At the hip, the gluteus maximus is a strong thigh extensor. Gluteus maximus pathology will appear in two distinct circumstances. Patients will show signs of trouble climbing stairs. Leaning the patient up to the next stair level is the function of the gluteus maximus. The femoral nerve innervates the quadriceps femoris, which flexes the thigh at the hip and the leg at the knee to raise the foot to the next stair level. When getting out of a chair, the gluteus maximus is used in a second scenario. These movements make effective use of the thigh’s capacity to expand at the hip.
The gluteus maximus’ function in power extension during pelvic thrusting during sexual activity is another frequently overlooked feature.
Embryology
Neural crest cells create the inferior gluteal nerve, which is part of the peripheral nervous system. During the early stages of vertebrate development, neural crest cells form in the space between the neural plate and the non-neural ectoderm. The ectoderm will ultimately develop into the epidermis, the neural plate into the central nervous system, and the neural crest into the peripheral nervous system. The inferior gluteal nerve is part of the sacral plexus and transports the fifth lumbar division through the second sacral.
Anatomical Variation
Variations in the inferior gluteal nerve’s path have been the subject of some research. Similar to the variances observed with the sciatic nerve, Tillman discovered that 17 out of 112 people had the inferior gluteal nerve travel through the piriformis. They found that men were more likely to have this variant.
The gluteus maximus was innervated by a division of the common peroneal nerve in a rare example from Sumalatha et al., where the inferior gluteal nerve was missing. In around 0.2% to 4.4% of adults, the inferior gluteal nerve will pass superiorly to the piriformis, even though most anatomy textbooks depict it going below the piriformis.
Variations in the Inferior Gluteal Nerve
A variation of the inferior gluteal nerve and sciatic nerve has been reported. The inferior gluteal nerve on the right was quite thick. The common fibular nerve gave rise to the inferior gluteal nerve. These differences make injections in the sciatic and inferior gluteal nerves potentially highly crucial and even harmful when used intramuscularly to treat a spastic piriformis muscle for piriformis syndrome.
There has been an instance of the inferior gluteal nerve being absent from birth. The tiny medial trunk and the much thicker lateral trunk were formed by the innervation of the piriformis muscle, which was punctured by the common fibular nerve. Once more, these differences are crucial for deep injections of the gluteal region, including piriformis muscle injections. Nerve block damage during posterior hip surgeries is another factor to take into account.
There have been reports of bilateral variants in the sciatic nerve, where the tibial nerve division exited below the piriformis on the right and subsequently joined the tibial division, whereas The piriformis muscle is where the common fibular nerve leaves the body.
Clinical Importance
Sciatica
Piriformis syndrome usually affects the sciatic nerve, although it can affect any structure that passes through the infra-piriform foramen, including the inferior gluteal nerve. Gluteus maximus atrophy is the predominant symptom of inferior gluteal nerve entrapment.
One useful method for evaluating a neurological injury is the Seddon and Sunderland categorization of peripheral nerve impairment. Neurapraxia, axonotmesis I–III, and neurotmesis are the five primary categories of nerve impairment established by Seddon and Sunderland. Neurapraxia is characterized by localized demyelination. The likelihood of a full recovery is often highest in this condition, which is the least severe. A more advanced stage of nerve damage that affects the axon is called axonotmesis.
The surrounding endoneurium and perineurium are involved in the progression of axonotmesis grade I to III. Although it is less common, this stage can recover. The most severe stage is neurotmesis. Post-surgical compromise is commonly present at this point, which usually entails total transection. Without surgical repair, the majority of these disorders do not completely heal. An end-to-end repair of the damaged nerve is the recommended therapy for these problems. 70% of patients with iatrogenic nerve injury recovered well after surgery, according to Kretschmer et al.
Sciatica is a type of pain that radiates down the back of the lower limb from the sacral plexus. A herniated lumbar disc can cause compression of the sciatic nerve’s extra-spinal segments, which can mimic sciatica. Lumbar discomfort may result from pathology affecting the hip and sacroiliac joints. Sciatica was long believed to be caused by a herniated lumbar disc. This is undoubtedly the case, although sciatic neuropathy might be mistaken for a piriformis condition.
Damage to the sciatic nerve causes paresthesias in the leg and foot, radicular pain in the hip or lower back, and pain when sitting. There may be motor weakness or abnormal reflexes.
Piriformis Syndrome
The anterior sacrospinous ligament, the sacroiliac joint, the sacrotuberous ligament, and segments S2–S4 of the sacrum are the origin of the piriformis muscle. On the greater trochanter, it inserts onto the femur after leaving the greater sciatic foramen.
Buttock discomfort, sciatic notch soreness, pain that worsens when sitting and goes away when standing, and higher pain when doing certain tests, including the FAIR test and Pace test, are the most typical signs of piriformis syndrome. The inferior gluteal nerve may be the origin of certain myogenic buttock discomfort.
There are two distinguishable forms of piriformis syndrome: primary piriformis syndrome, which is caused by the piriformis itself, and secondary piriformis syndrome, which is caused by a difference in leg length, fibromyalgia, congenital variation in the piriformis and sciatic nerve length, or spinal stenosis. Wallet neuritis, extra-spinal sciatica, and deep gluteal space syndrome are synonyms for piriformis syndrome.
Injections of corticosteroids reduce piriformis syndrome discomfort.
Wallet Neuritis Syndrome
Despite the absence of neurological tests for piriformis syndrome, such as flexion, adduction, internal rotation (FAIR test), and pace sign, wallet neuritis (sitting with a fat wallet in the back pocket) might resemble the condition. An extra-spinal neuropathy called wallet neuritis affects the ipsilateral side of the body and results in lower limb and gluteal discomfort.
Deep Gluteal Space Syndrome
In deep gluteal syndrome, non-discogenic sciatic nerve entrapment causes gluteal discomfort from extra pelvic sciatic nerve entrapment. The diagnosis of sciatic nerve lesions may be complicated by extra-spinal lesions of the sciatic nerve. Cluneal condition, osteitis ilii, quadratus lumborum syndrome, and piriformis syndrome are examples of these extra-spinal lesions. Therefore, whereas some authors describe the piriformis as a distinct structure, others claim that the phrase “deep gluteal space” now includes the piriformis.
The following are the limits of the deep gluteal space.
- The proximal femur, posterior acetabular column, and hip joint capsule form the anterior border.
- The Gluteus maximus and inferior gluteal nerve form the posterior border.
- Lateral boundary: gluteal tuberosity and the lateral lip of the linea aspera
- Medial border: sacrotuberous ligament and falciform fascia
- The Sciatic notch and the surrounding osseous edge form the superior boundary.
- On the inferior side, the hamstring muscles originate from the ischial tuberosity.
- The vascular system, the Gemelli-obturator complex, the piriformis muscle, and the hamstring muscles are all found in the deep gluteal area. Ischiofemoral impingement, fibrous bands connected to the sciatic nerve, and piriformis syndrome are issues related to the deep gluteal region.
Some of the tissues seen in the larger sciatic foramen may be connected to the deep gluteal space syndrome. These include the sciatic nerve, the quadratus femoris, the obturator internus, the posterior femoral cutaneous nerve, the superior and inferior gluteal nerves, and the pudendal nerve.
Buttock and sciatic discomfort, aversion to sitting, loss of lower extremity feeling, limping, lumbar pain, and nocturnal pain are the most typical signs of deep gluteal space syndrome.
The anterior/seated piriformis test, Lasegue test, Freiberg sign, Beatty sign, Pace sign, and the FAIR test are some of the tests that might help identify deep gluteal space syndrome.
Both endoscopic and open surgical techniques can be used to reach the deep gluteal region.
Surgical Importance
Total Hip Arthroplasty (THA)
Posterolateral Approach
The posterolateral approach is one of the most popular surgical techniques used by total joint replacement surgeons. A real inter-nervous plane is not used in this dissection. The gluteus maximus fibers are bluntly dissected proximally and the fascia lata is sharply incised distally during the intermuscular gap. The hip joint capsule and the short external rotators are carefully dissected during the thorough dissection. These structures, which are subsequently restored to the proximal femur via trans-osseous tunnels, require caution to preserve.
Peripheral Nerve Injury in THA
The incidence rates and total risk of peripheral nerve damage with the most popular THA techniques have been documented in several of studies. The literature reports a wide range of incidence rates. Up to 8% of THA patients had the condition, according to reports from the 1980s and 1990s. According to more recent research, THA patients had a 0.6% to 3.7% chance of suffering nerve damage, with the incidence rate at least doubling in the revision situation. Since the early 1970s, the latter has been extensively documented in the literature.
Inferior Gluteal Nerve Considerations
The inferior gluteal nerve receives far less attention in the literature than injuries to the sciatic, femoral, obturator, superior gluteal, and lateral femoral cutaneous nerves. The precise “definition” of a clinical result varies greatly from one research to the next. Thankfully, most nerve injuries (i.e., moderate neuropraxia) are not severe. The actual frequency of neurologic damage after THA, however, is probably underestimated by the postoperative clinical assessment; this is especially true for the inferior gluteal nerve.
The inferior gluteal nerve’s architecture and path to its anatomic vulnerability during the posterolateral approach to the hip have been described by several cadaveric investigations. Apaydin et al. created a triangle landmark for the inferior gluteal nerve using 36 cadavers, which included the greater trochanter, ischial tuberosity, and posterior inferior iliac spine.
Other Technical Considerations
The potential advantages of minimally invasive THA procedures can only be realized clinically with a thorough understanding of nerve anatomy, even though many authors advocate for their use. This is because the advantages of improved visualization during these procedures may be outweighed by the possibility of iatrogenic neurovascular injuries.
There are ways to lessen the possibility of nerve damage. One method is a less invasive total hip replacement, in which the surgeon removes less tissue and does not cut the gluteus maximus tendon, greatly minimizing nerve damage. Nevertheless, mastery is necessary for greater comprehension of the nerve’s path.
Marcy et al. outline an alternative method for treating the hip. Instead of splitting the gluteus maximus, they only pull the muscle back with minimal nerve injury. However, there are drawbacks to this method. It is labor-intensive as it necessitates a large amount of muscular mobilization. The gluteus maximus muscles are divided in the more popular method. The incision must run about 10 cm down the iliotibial tract and be 5 mm or less from the greater trochanter’s apex. The inferior gluteal nerve will be safeguarded by this path.
FAQs
What is the difference between superior and inferior gluteal nerves?
The sciatic notch above the piriformis muscle is where the superior gluteal nerve (L4, L5, S1) travels. It feeds the muscles of the tensor fasciae latae and gluteus medius minimus. The inferior gluteal nerve supplies the gluteus maximus (L5, S1, S2).
What is entrapment of the inferior gluteal nerve?
One uncommon (or underappreciated) cause of low back and buttock discomfort is inferior gluteal nerve entrapment. The discomfort that results from the piriformis muscle trapping is sometimes mistaken as myofascial pain.
How do you treat gluteal nerve pain?
Treatment for Deep Gluteal Pain Syndrome
Anti-inflammatory drugs are prescribed to alleviate pain and swelling.
Muscle relaxants to help tight muscles relax.
Stretching and strengthening the gluteal muscles is accomplished through physical therapy.
Muscle spasms can be prevented and extreme pain can be lessened by electrotherapy (TENS).
What is the inferior gluteal nerve used for?
The primary motor neuron innervating the gluteus maximus muscle is the inferior gluteal nerve. It controls how the gluteus maximus moves during tasks like ascending stairs that call for the hip to stretch the thigh.
What occurs if there is injury to the inferior gluteal nerve?
Alteration in the gait cycle (gluteus maximus ‘lurch’) and wasting of the ipsilateral gluteus maximus muscle, which results in the loss of the defined form of the affected buttock, are the main sequelae of inferior gluteal nerve injuries.
References
- Gluteal nerves. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/gluteal-nerves
- Gluteal nerve. (2023, July 30.) StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK532884/
- Wikipedia contributors. (2024b, July 27). Inferior gluteal nerve. Wikipedia. https://en.wikipedia.org/wiki/Inferior_gluteal_nerve