Post-Traumatic Elbow Stiffness
Introduction
Post-traumatic elbow stiffness is a condition characterized by reduced range of motion in the elbow joint following an injury, such as fractures, dislocations, or soft tissue damage. It results from scar tissue formation, joint contractures, or heterotopic ossification. Management typically involves physical therapy, stretching, and, in severe cases, surgical intervention to restore mobility and function.
The elbow joint range of motion is restricted by a common condition called post-traumatic elbow stiffness. After an injury to the elbow joint or surrounding tissues, it may happen.
Several surgical procedures are now available, and the recommendation must be based on the surgeon’s skill level, the patient’s features, and the extent of joint limitation. Joint degradation and incongruence negatively impact the prognosis, while a positive surgical prognosis has been linked to heterotrophic ossification alone.
Post-traumatic Stiffness: What Is It?
In medicine, stiffness is the inability to move a joint because of a loss of range of motion caused by an illness or injury (such as trauma).
A crippling consequence of trauma that results in decreased or lost motion and functional impairment is post-traumatic stiffness. It will be challenging for you to bend or straighten your elbow and carry out daily tasks if you have post-traumatic stiffness in it. Both intrinsic and extrinsic post-traumatic stiffness are possible.
Pathogenesis
Post-traumatic elbow stiffness has a complex etiology, with both extrinsic and intrinsic causes frequently contributing to the development of a clinically stiff elbow. The elbow articulation itself has intrinsic causes of post-traumatic elbow stiffness, which might include impinging osteophytes from future arthrosis or articular incongruities from the initial trauma. Motion-limiting intra-articular adhesions can arise after immobilization following trauma or surgery.
Retained hardware, capsular contractures, and heterotopic ossification are common extrinsic causes of elbow stiffness. One type of dystrophic calcium deposition that arises from local tissue damage due to stress, whether from injury or surgery, is heterotopic ossification. Depending on its location, the ossified deposit might limit flexion-extension, or both.
It functions as a mechanical block to motion. Although there are no known patient-related risk factors for the development of heterotopic ossification following elbow trauma, glenohumeral dislocation, a longer recovery period between injuries and surgeries, and more surgical operations are independent risk factors for the development of heterotopic ossification.
Classification
The Kay and Morrey classification systems are the two primary classification schemes used to describe elbow stiffness. The process that contributes to stiffness is the foundation of the Kay classification system.
- Soft-tissue contracture (type I)
- Soft-tissue contracture with ossification (type II)
- Nondisplaced intra-articular fracture with soft-tissue contracture (type III)
- Displaced intra-articular fracture with soft-tissue contracture (type IV)
- Post-traumatic osseous bars (type V)
Soft tissue contracture(type I)
Elbow motion is physically restricted by soft tissue contractures, which results in stiffness. The elbow capsule thickens in individuals having surgery to remove soft tissue contractures and is frequently linked to post-traumatic stiffness. Additional investigation has also shown that there are more myofibroblasts, which are very contractile, and that the extracellular matrix is proliferating. Increased collagen crosslink production, decreased proteoglycan content, and lower water content have all been shown by histology.
Heterotopic ossification(type II)
The improper production of mature lamellar bone into non-skeletal tissue is known as HO, and it may also be the cause of post-traumatic stiffness. Pluripotent mesenchymal cells undergo differentiation into osteoblasts, which then generate osteoid, which mineralizes into bone, to form this heterotopic bone. The resulting ectopic bone has no real periosteal layer and is more metabolically active.
The heterotopic bone may be differentiated from other pathological bone-forming states such as myositis ossificans and periarticular calcification, where amorphous calcium deposits accumulate in soft tissues surrounding the elbow following injury, since histologically it looks exactly like natural bone. Clinically, HO shows up as a mechanical block to elbow joint action, which limits the range of motion. Imaging can be used to identify the appearances.
Nondisplaced intra-articular fracture with soft-tissue contracture (type III)
An elbow stiffness condition known as “nondisplaced intra-articular fracture with soft-tissue contracture (type III)” occurs when there is a little fracture within the joint itself that is not greatly displaced but is accompanied by tightening of the soft tissues around it.
Displaced intra-articular fracture with soft-tissue contracture (type IV)
The term “displaced intra-articular fracture with soft-tissue contracture (type IV)” describes a kind of elbow stiffness that particularly denotes a considerably displaced fracture within the joint along with tightened soft tissues surrounding the elbow joint.
Post-traumatic osseous bars (type V)
Because of the disruption of the germinal matrix and related vascular supply, which may result in bone development arrest, altered joint mechanics, and functional impairment, Salter-Harris V injuries frequently have a bad prognosis. Orthopedic examination and subsequent surgical intervention are therefore frequently necessary.
Causes
Orthopedists are aware of the elbow joint’s tendency to become stiff following trauma, which can happen even in cases of minor trauma. The high degree of congruence, the intricacy of the joint surfaces, and the high tissue sensitivity to trauma, particularly in the joint capsule, are the primary factors that expose the elbow joint to this problem. Orthopedists can directly affect parameters related to a range of motion loss, in addition to the direct correlation between elbow joint stiffness and trauma, inadequate rehabilitation, and needless protracted immobilization.
The following are the main reasons for post-traumatic elbow stiffness:
- Bone fracture in the elbow
- Previous surgery to the joint
- Loose bodies in the elbow
- Mal-union (improper healing of a fractured bone)
- Elbow Dislocation
- Heterotopic ossification (bone growth in non-skeletal tissues)
- Cranial trauma (injury to brain, skull)
Post-traumatic elbow stiffness is diagnosed and treated based on its cause.
Symptoms
- Pain in the elbow
- A feeling of a locked elbow
- Decreased motion of the joint
Diagnosis
Assessment
Measuring and comparing elbow flexion and extension to the contralateral side is important because, in healthy individuals, maximal flexion and extension range from 140° to 150° and –10° to 10°, respectively, and are influenced by age and sex. Even though elbow stiffness is typically painless, end-range pain is typically present. Although it might be challenging to measure in patients with a restricted range of motion, elbow stability is frequently not abnormal.
The chance of ulnar entrapment in stiff elbows is increased by pathological alterations of the posteromedial capsule, tissue scarring, or even protruding iron from prior surgery, particularly in posttraumatic stiffness. Consequently, the location in the ulnar nerve’s sulcus should be meticulously recorded, and the nerve itself should be closely inspected for indications of instability or entrapment. Deep flexion may cause symptoms of adhesion or ulnar entrapment.
Unpleasant stiffness, tenderness, or warmth can be a sign of an active infection or inflammation. Measurements of inflammatory indicators (erythrocyte sedimentation rate and C-reactive protein level) are necessary for additional evaluation to rule out infection.
Aspirating the elbow joint and sending synovial fluid for additional examination is recommended for patients exhibiting signs of an active infection. The function of the ulnar nerve must always be given particular consideration during a neurological examination. Assessing the degree of brain injury may require nerve conduction investigations and electromyography.
Physical examination

A physical examination of the affected elbow and a review of your medical history are the initial steps in diagnosing post-traumatic stiffness. Following that, the physician will check for inflammation and flexion range. The initial diagnosis may also be confirmed by an MRI, CT scan, or X-ray (radiograph).
Treatment
Nonoperative treatment
The initial nonoperative therapy strategy will involve either static or dynamic elbow splinting. Additional choices include:
- Physical therapy
- Occupational therapy
- Serial casting of the joint
- Passive mobilization
- Joint immobilization
- Manipulation under anesthesia
- Administration of NSAID
- Botulinum toxin A injections
- Splinting or bracing.
Maintaining the maximum range of motion acquired during surgery is the aim of postoperative rehabilitation. Early active mobilization within 24 to 48 hours is therefore crucial. Sufficient management of postoperative pain is necessary for this. In a specific postoperative rehabilitation plan, patients should be encouraged to rebuild their elbow’s strength and reintegrate it into their daily lives.
The majority of ROM improvement occurs during the initial months of rehabilitation, according to several studies. Contractures that are resistant to conventional exercise regimens can be successfully treated with adjuvant splinting, which can be utilized for 20 days to three months. Since only slight improvements in range of motion are seen until 12 months into treatment, sticking with it can be beneficial.
Physical therapy treatment
Physiotherapy (PT) is an essential and adaptable treatment for posttraumatic stiff elbow. Starting within six months after the stiffness’s development yields the best outcomes. Supine is the ideal posture for active mobilization because it elevates the upper arm and lessens the strain on the joint stabilizers. Exercises that improve proprioception and increase vascular circulation in the hands and wrists can be added in addition to active and passive mobilization to reduce edema.
Elbow flexion
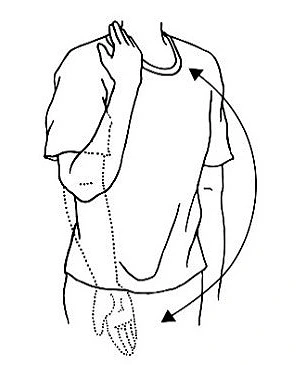
- Drop your arm to one side and stand up.
- Slowly bend your arm upward until your hand touches your shoulder, using a modest weight or none at all.
- Repeat ten times while holding this position for 15 to 30 seconds.
Elbow Extension
- Hold one arm straight over your head.
- Relax to the starting position after bending your arm backward at the elbow until it is no longer possible.
- Perform ten repetitions in each of the first three sets.
Supination/Pronation
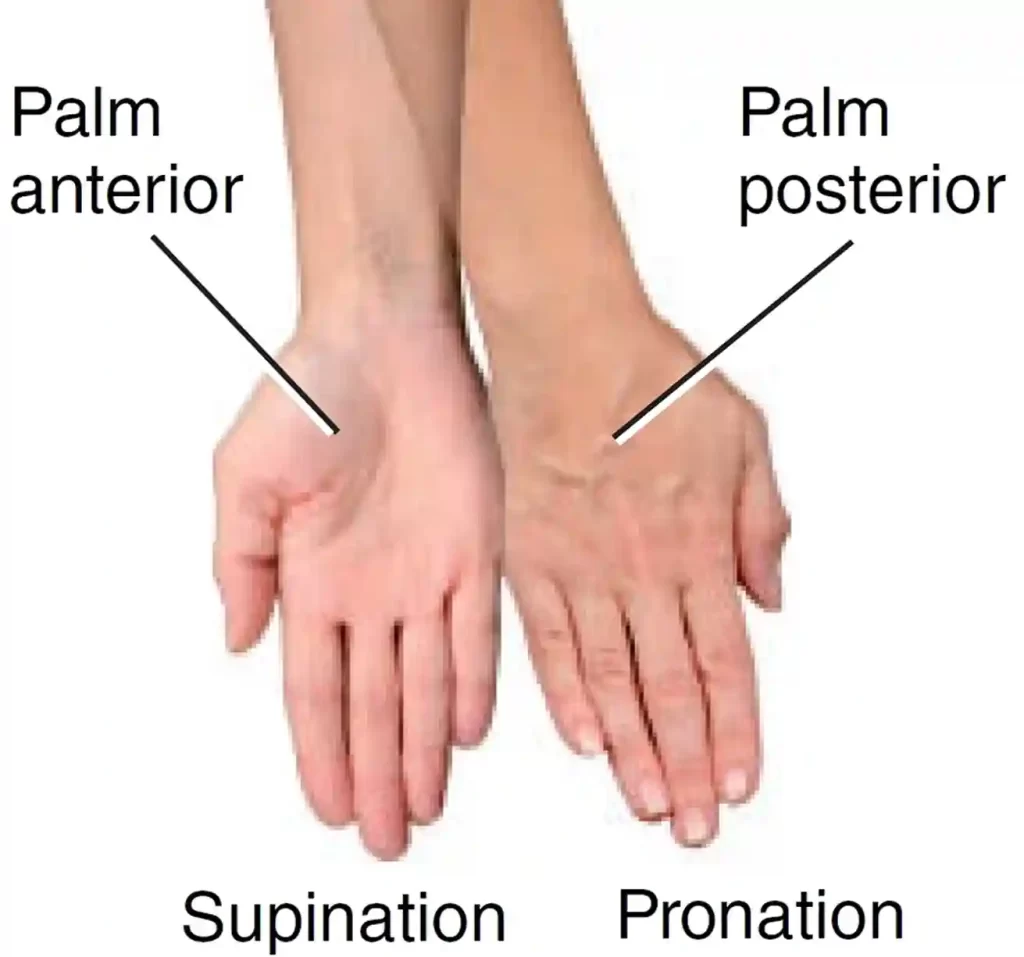
- Holding a hammer, lower it from right to left, then back again while keeping your elbow on a table.
- Throughout the movement, maintain a straight wrist and maintain control.
- Do this exercise ten times.
Towel Twist

- Hold a towel in both hands while reclining in a chair.
- As if you were wringing out water, twist the towel in different directions.
- After ten repetitions, switch directions for ten more repetitions.
Foam Ball Squeeze
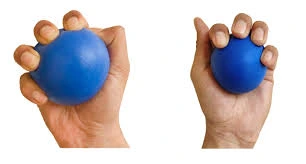
- Squeeze a ball of soft foam in your hands.
- Repeat ten to fifteen times with both hands after holding for thirty seconds.
- Do this exercise two or three times every week.
Stretching exercises:
- Overhead elbow extension: Hold the stretch while extending your arm overhead and bending your elbow slightly back.
- Forearm rotations: Turn your forearm inward and outward while keeping it bent at a 90-degree angle.
- Elbow flexion stretches: With your other hand, gently draw your elbow toward your shoulder.
- Wrist flexor stretches: Bend your wrist gently in your direction while extending your arm straight out with your palm facing down.
Splinting

The conservative management of posttraumatic elbow stiffness frequently involves the use of static, static progressive, and dynamic splinting procedures. To provide stretch in the area that needs the greatest improvement, static splinting entails immobilizing the joint with a static splint.
The static progressive kind allows the patient to enhance joint mobility by progressively increasing tension using a turnbuckle or a strap and loop. It is advised to wear static (progressive) splints for 30 minutes, three times a day. Conversely, dynamic splints employ a spring to allow for flexion or extension in the other direction during active movements while facilitating less tension in the direction that needs development.
It is advised that dynamic splits be worn for a further 6 to 8 hours, ideally at night. Nevertheless, dynamic splints are generally fairly heavy, which makes wearing them at night unsightly. Additionally, these splints cost more than turnbuckle splints. For the treatment of elbow stiffness, splinting can be static, static progressive, or dynamic.
Every splinting technique produced a significant and long-lasting increase in range of motion (ROM), with the static progressive and dynamic splinting groups experiencing improvements in ROM of about 40°. However, static progressive splinting and dynamic splinting produced better results than static splinting for improving flexion.
Continuous passive motion therapy
There has been discussion over the effectiveness of continuous passive motion (CPM) therapy in postoperative rehabilitation for many years. CPM is thought to hasten the removal of hemarthrosis while halting the development of further periarticular soft tissue edema caused by variations in IA pressure. Although a favorable effect was shown, there was insufficient proof in earlier research, and employing a CPM raised patient expenses considerably.
However, O’Driscoll et al. conducted a recent single-center randomized controlled trial in which they directly compared the use of PT and CPM four weeks following surgical arthrolysis. While pain levels, opiate use, and patient-recorded outcome measures were comparable, the results demonstrated that CPM was superior to PT at three, six, and one year in terms of regained total and functional range of motion and time lost from performing daily tasks.
Manipulation under anesthesia
To reduce the risk of iatrogenic fractures, we advise against manipulating under anesthesia for more than eight weeks following trauma or surgery. However, manipulation under anesthesia can be used as a treatment option for early-evolving joint stiffness resistant to intensive physical therapy and splinting, and it is an effective addition to therapy for increasing flexion-extension if used within three months of the injury, fracture fixation, or arthrosis.
Immediate Postoperative Phase:
- To preserve the surgical site and promote recovery, the elbow is usually immobilized with a brace or splint.
- To avoid stiffness and encourage joint mobility, early range-of-motion exercises are started under the direction of the surgeon and physical therapist.
Weeks 1-6:
- To stop stiffness from returning, the focus is on early mobilization and mild progressive range-of-motion exercises.
- To regain function stability and strength around the elbow joint, forearm, and upper arm strengthening activities are started.
Weeks 6-12:
- The rehabilitation program advances to incorporate more strenuous range-of-motion exercises and functional activities as the patient heals.
- Under the direction of the medical team, elbow-related tasks like lifting and reaching are gradually reintegrated.
Months 3-6:
- The emphasis switches to maximizing joint strength, flexibility, and function as well as a gradual return to daily tasks and leisure activities.
- To provide the best possible functional recovery, progressive strengthening activities and neuromuscular re-education are prioritized.
Long-Term:
- It takes several months to fully heal and resume high-impact activities, with continued monitoring to evaluate joint stability, function, and any possible surgical-related issues.
- Patients must carefully follow the recommended rehabilitation program, show up for follow-up appointments, and discuss any issues or worries they may have during the healing process to maximize the results of elbow stiffness release surgery.
Operative treatment
Elbows with osseous contact or tissue contractures that do not respond to conservative treatment should be treated surgically. The choice between open arthrolysis and arthroscopic arthrolysis depends on several factors, such as the etiology, the location of prior surgery, and the involvement of the ulnar nerve. Arthroscopy provides better joint visualization, less scarring, a lower risk of infection, less pain and swelling, and a quicker recovery than open arthrolysis.
- Open arthrosis (with external fixation)
- Arthroscopic arthrosis
- Partial or total elbow arthroplasty
- Interposition arthroplasty
- Corrective osteotomy with arthrodesis
- Capsular release
- Osteophyte excision
- Musculocutaneous neurectomy
Arthroscopic Surgery for Elbow Stiffness
The limited range of motion in the elbow joint can be addressed with minimally invasive arthroscopic surgery, also referred to as arthroscopic capsular release or arthroscopic contracture release. The procedure entails making small incisions around the elbow, inserting an arthroscope to view the inside of the joint, and using specialized tools to remove adhesions, release scar tissue, and increase joint mobility.
External fixation
In the previous paragraph, the benefits and efficacy of external fixation were presented. After elbow arthrolysis, Shanghai Sixth People’s Hospital has implemented a three-phase external fixation rehabilitation program. Forearm rotation exercises (at least twice daily) and active, assisted, and passive cycles of flexion-extension exercises (30 on the first day, increased by 30 per day until 300 were achieved) are prescribed to patients during the first six weeks following surgery, under the careful supervision of a physical therapist or family members. After every ROM training session and while you sleep, the fixator is locked in the most severe position for elbow flexion or extension. Fixator removal is often done in the outpatient operating room for six weeks.
Total elbow arthroplasty
- This is recommended for older individuals (over 65) who exhibit significant elbow functional impairments in addition to joint surface deterioration.
- Due to the connection between the ulnar and humeral components, a total elbow arthroplasty used to treat fractures is an intrinsically stable structure. A possible drawback of this method is the possibility of stem loosening due to polyethylene wear at the implant connection and transferring weight to the stem-cement-bone contact.
- This procedure is not well documented in the orthopedic literature. Results and complication rates from complete elbow arthroplasty in individuals who had previously had interposition arthroplasty were similar to those following a series of revisions.
Precautions for total elbow arthroplasty
- Active extension should be stopped for 4–6 weeks to facilitate bone-tendon healing if a triceps-reflecting technique has been used.
- Such a restriction is not required if a triceps-sparing technique has been employed.
- To reduce the chance of early polyethylene wear and stem loosening after complete elbow replacement, patients are advised to refrain from heavy or repetitive usage of the operated arm for the rest of their lives.
Interposition arthroplasty
Replacing the joint can significantly reduce pain and restore a reasonable amount of elbow motion for elderly individuals with advanced posttraumatic osteoarthritis-related elbow stiffness. For younger, more active patients, however, interposition arthroplasty may be a viable option for joint replacement since it seeks to improve function and reduce pain while maintaining functional stability. The distal humeral and ulnar articular surfaces are reshaped, a new congruent joint is made, and biological materials such as dermal allographs, Achilles tendon, or fascia Lata allograft are used to resurface the joint. Furthermore, it is possible to repair the collateral ligaments. Nevertheless, this technique’s results are not very predictable.
Capsular release
In the context of post-traumatic elbow stiffness, a “capsular release” is a surgical procedure that allows the elbow to bend and straighten more freely by cutting the contracted joint capsule around the elbow via an open incision or arthroscopically using tiny cameras and tools. This procedure is usually performed when significant stiffness develops after an elbow injury.
Complication
- Heterotopic ossification (HO): The formation of new bone in the soft tissues surrounding the elbow, known as heterotopic ossification (HO), is a serious problem since it severely restricts the range of motion.
- Capsular contracture: This condition limits elbow flexion and extension by tightening the joint capsule.
- Nerve damage: Numbness and tingling in the hand can result from damage to the ulnar nerve, which is especially susceptible to injury close to the elbow.
- Post-traumatic arthritis: Degenerative arthritis characterized by pain and stiffness can result from repeated trauma to the elbow joint.
- Functional limitations: Everyday tasks including eating, dressing, and maintaining personal hygiene can be severely impacted by severe elbow stiffness.
Prevention for elbow stiffness
Preventive measures are crucial since treating a stiff elbow can be challenging. It has been hypothesized that stiffness after surgery or joint damage progresses via four stages: granulation tissue, fibrosis, edema, and bleeding. 24 Active mobilization, which helps to minimize edema and a rise in the viscosity of inflammatory exudates, which may ultimately predispose the joint to adhesion development, and early surgical intervention for fracture or joint instability are important strategies to prevent elbow stiffness.
Conclusion
A patient’s ability to do activities of daily living is seriously hampered by elbow stiffness, which is also difficult for doctors to treat. To gain a better understanding of the underlying etiology and to establish a strong foundation for the suggested treatment, a comprehensive preoperative workup that includes a 3D CT scan and a radiologic evaluation with a particular focus on the ulnar nerve is necessary. The basis for treatment is whether osseous impingement, soft tissue contracture, or a mix of the two are involved. If conservative measures are ineffective, arthroscopic arthrolysis has emerged as a reliable initial surgical option. Compared to open arthrolysis, this approach has fewer indications but lower rates of complications and revisions. In postoperative rehabilitation, splinting or CPM is necessary in addition to early active mobilization.
FAQs
How can my elbows be relaxed?
Just move your fingers gently toward the bottom of your wrist while keeping your elbow straight out and your palm toward the floor. The back of your forearm should feel stretched. For 30 seconds, hold it.
How is stiffness in the elbow after trauma treated?
Post-traumatic elbow stiffness can be managed non-surgically with joint immobilizers and physical therapy. Conservative treatment is common up until the fourth month, especially when stiffness is not linked to heterotopic ossification or joint deformity.
What is the duration of elbow stiffness following trauma?
Patience is necessary since splinting can alleviate posttraumatic elbow stiffness over a 6- to 12-month period. As a result, we advise a minimum of six months of treatment, or until a pending contract is reached.
How can pain after an elbow fracture be eliminated?
If left untreated, it can potentially result in long-term joint dysfunction and limited range of motion. Therefore, to help lessen post-fracture elbow stiffness and enhance joint function, physical therapy is usually advised. This includes manual treatment, soft tissue mobilization, and range of motion exercises.
How can stiff elbows be loosened?
Applying a body wash that has additional moisturizers added. Treating a particular skin disease, like eczema, with a moisturizer that has been specially prepared. If someone spends a lot of time resting on hard surfaces, they should use elbow pads. Steer clear of aggressive exfoliator products that could aggravate skin irritation or exacerbate dryness.
How can a stiff elbow be massaged?
A popular method here is to apply deep pressure with both thumbs at the center of the muscle, pressing into the knots or scar tissue. Smaller adhesions and scar tissue are broken away with a circular motion when the muscle feels like it is relaxing.
How can someone who has a stiff elbow sleep?
Lying on your back with a pillow supporting your arm is one of the greatest ways to sleep if you have a sore elbow. By doing this, you can lessen the tension on your elbow joint and maintain your arm in a neutral position. To add support, you can also try sleeping on your side with a pillow between your arms and body.
After an injury, how may stiffness be reduced?
Use ice in the evening to lessen pain or swelling from movement during the day, and heat in the morning to warm up tense muscles. Contrast treatment, which alternates between cold and heat, helps to shift inflammation away from the affected area by constricting and widening the blood vessels.
What signs of elbow post-traumatic arthritis are present?
Elbow bending and straightening become more challenging for patients. Rotation of the forearms frequently causes pain for patients as well. Locking of the elbow or a catching sensation from loose bodies in the elbow are further signs of elbow arthritis.
Reference
- Post-traumatic stiffness Henderson | Elbow Trauma | Elbow Pain Las Vegas. (n.d.). https://www.totalsportsmedicine.com/post-traumatic-stiffness-orthopedics-sports-medicine-surgeon-las-vegas-nv.html
- Borras, M. (n.d.). Post-Traumatic elbow stiffness | Rothman Orthopaedics. https://rothmanortho.com/specialties/conditions/post-traumatic-elbow-stiffness