Trigger Points
What are Trigger Points?
Trigger points, often called muscle “knots,” are sensitive areas within muscle fibers that can cause pain in other parts of the body. These tight spots form when muscle fibers contract and are unable to release, leading to localized tension and tenderness.
Trigger points can be active, where they consistently cause pain, or latent, where they only cause discomfort when pressure is applied.
Definition/Description of Trigger Points:
The responsive spots or palpable nodules in the tight bands of the musculoskeletal muscles’ fascia are trigger points (TrPs). Jump signs, local soreness, a local twitch reaction, and referred pain—typically manifesting as a pain pattern far from the site—can all be brought on by direct compression or muscle contraction.
The severe pain often takes people aback. They tremble or cry out in response, which seems disproportionate to the pressure the probing fingers exert. They make uncontrollable movements, jerking the head, shoulder, or body parts that cannot be felt. Consequently, an excessively tender TrP is indicated by a jump indication.
There is a momentary visible or palpable contraction of the muscle and skin when pressure is put on them either by needle penetration or transversal slamming palpation. This phenomenon is known as the local twitch reaction. One commonly recognized diagnostic indicator is a local twitch response to activating active TrPs.
Pain experienced somewhere other than the site of the unpleasant stimulus is referred to as pain, sometimes reflected pain. No particular neurological deficiencies or joint swelling are seen. Any person of any gender or race can recreate the unique, recognizable, and persistent pattern or map of pain that characterizes myofascial TrP.
(Radiating pain and referred pain are slightly different. For instance, chest discomfort associated with a myocardial infarction may be either radiating or referred. Referred pain occurs when the pain is near or distant from the affected organ; for example, when a person has pain in their left arm or jaw but not in their chest.)
Causes of Trigger Points:
- Growing older
- harm is brought on by stress, birth trauma, or falls.
- Lack of exercise is prevalent among sedentary people aged 27 to 55, with men making up 45% of this population
- Poor posture includes sitting cross-legged, swayback, telephone, and upper and lower crossing patterns.
- Overuse of muscles and the resulting microtrauma—weightlifting,
- Anxiety, depression, psychological stress trauma, other chronic stress conditions
- hypermobility, joint issues, and disturbed sleep.
TrP classification:
TrPts can be categorized into several classes:
Points of Trigger for Primary, Central, and Secondary Systems
The referred pain map indicates that primary or central TrPs are those that produce excruciating pain locally when under pressure and exposed to radiation. tend to be concentrated in the center of a strong abdomen.
Existing core trigger points in nearby muscles cause secondary or satellite TrPs to form. When the central TrP heals, they typically retreat on their own.
Active and Inactive /Latent Trigger Points
Any site that feels tender and refers to pain when palpated is considered active TrP. Palpation can also bring autonomic sensations, including sweat, lightheadedness, and skin redness.
Only intense digital pressure can cause local or referred pain, as latent TrP does not elicit pain on its own. In pain-free individuals, they may alter the patterns of muscular activation or result in muscle weakening.
Diffuse Trigger Points
Secondary multiple TrPs represent a response of a process known as diffuse, which frequently occurs in cases of severe postural deformity where the originating TrPs are many at first.
Attachment Trigger Points
appear in extremely delicate tendon-osseous connections. A neighboring joint may develop degenerative processes if left untreated.
Ligamentous Trigger Points
Trigger points can even form in ligaments. The presence of TrPs in the spine’s anterior longitudinal membrane may cause instability in the neck. When the ligamentum patellae and fibular collateral ligament are treated, certain knee pain syndromes can be resolved.
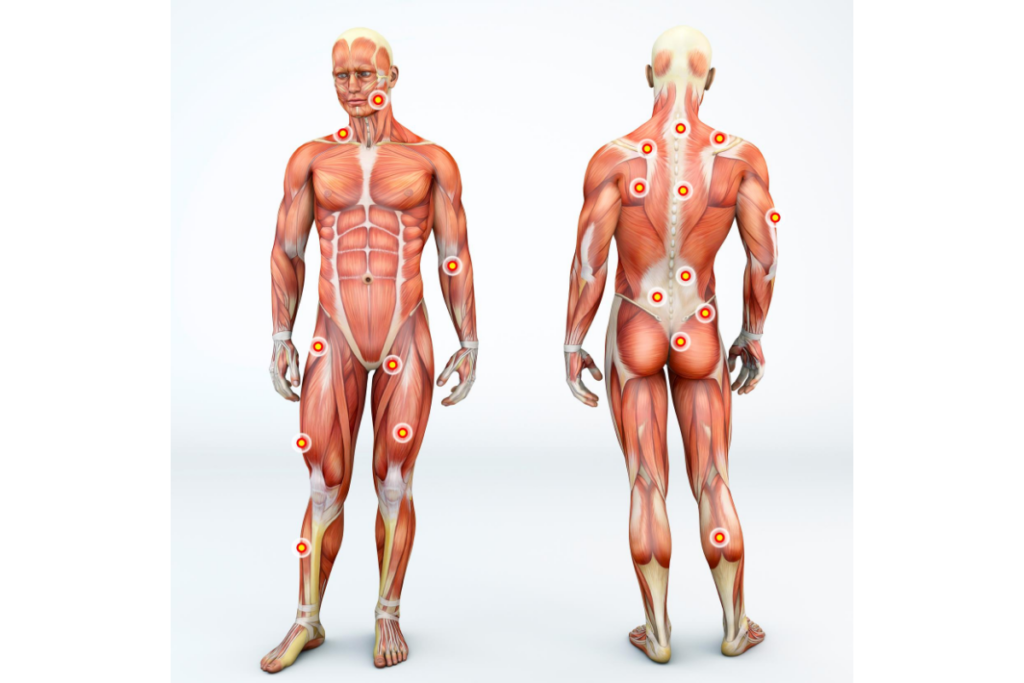
Where Can Individuals Find Trigger Points?
Anyplace on the body could potentially produce trigger points and knots in the muscle. There can be a tiny spot of tissue tension anywhere there is muscle tissue. This might act as a catalyst. Trigger points may be more prevalent in the following body parts:
- Your upper trapezius muscles are just above your shoulders, on either side of your neck.
- Your lower back’s quadratus lumborum muscles
- Your hamstrings
- Your calf muscles
- Along the band of your iliotibial
- Anywhere in your body can develop trigger points, and if they happen too frequently, you may develop chronic pain and myofascial pain syndrome.
Which symptoms are associated with trigger points?
How can you determine whether anything is a trigger point? Some frequent symptoms that help distinguish trigger point discomfort are listed below. Instead of being on a nerve or bone, the nodule or band you are pressing on is in a muscle. You’re pressing on a point about suffering. This is not the kind of nerve pain that feels like needles, pins, or an electric shock when you lightly touch a nerve. This is not the case with a trigger point referral. This ache radiates more like a dull aching agony. You have persistent muscle soreness that gets worse when you move or exercise. You’ve chronic muscle pain.
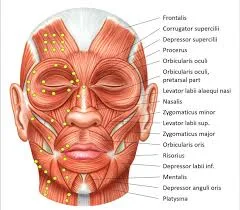
- In most cases, a patient seeks assistance for a chronic pain condition (such as headaches, aches all over, stiffness in the morning, temporomandibular joint syndrome, or tinnitus), which is frequently physically distant from the active trigger site.
- Impaired muscles or technically linked muscles may exhibit muscular weakness, imbalance, or altered motor recruitment.
- Range of Motion (ROM) changes.
- a painful motion. and/or that moving can occasionally make symptoms worse.
- Associated symptoms include tinnitus, migraines, tension headaches, and temporomandibular joint issues.
- Anomalies and compensations in posture
Deep hurting in a specific muscular location that is characterized as throbbing, tight, stiff, or vice-like. - Persistent or worsening pain
- a sensitive muscular knot. Trigger points are tiny lumps, nodules, or knots in muscles that hurt when touched and occasionally when left untouchable.
- Pain in the muscles that worsens as the injured or afflicted muscle is strained or stretched
- Pain-related sleep disruptions and behavioral issues
- reduced range of motion in the areas that are affected (e.g., you might not be able to rotate your shoulder all the way).
- Stiffness in the muscles
- Feeling tired
- A headache
- Lightheadedness
- Mood fluctuations
- painful or sensitive muscles
- The affected muscle or muscles are weak.
- Pain in the affected muscle that worsens with time or does not go away
- existence of excruciating muscle knots that, when compressed, cause excruciating regional or referred pain.Points of origin that cause discomfort
- Affected postures or irregularities in posture, such as hunching, rounding of the shoulders, or forward head posture (not in line with the spine)
Diagnostic Techniques of Trigger Points:
The palpation
Palpation is still the gold standard for diagnosing and evaluating TrPs, and emerging diagnostic techniques are evaluated against this standard. However, according to interrater reliability estimates, palpation is unreliable.
Imagining
Recently, imaging techniques have demonstrated the ability to detect TrPs:
Shear wave elastography and vibration sonoelastography are thought to produce more accurate results since they employ mechanically produced stimuli.
Anamnesis
A patient’s description of their medical history, or anamnesis, ought to be detailed. It is necessary to inquire about fibromyalgia and whether it runs in the family history of illnesses. Additionally, as a sedentary lifestyle and lack of exercise may be pathogenic factors, the patient should be questioned about his physical and everyday activities both now and in the past. In addition, it is necessary to inquire about and thoroughly assess chronic muscular overuse, everyday stress, drugs (and their usage), and sleep disorders.
Analysis
A worldwide Delphi panel updated the TrP diagnostic method in 2018 and suggested that a taut band, a hypersensitive area, and referral pain be present in at least two cases.
Moving the fingertips forward and backward perpendicular to the muscle fibers is the proper way to perform palpation. As an alternative, a pincer grasp can be used to palpate specific muscles. After identifying the taut band, it is important to pinpoint the hypersensitive area by gently compressing specific areas along the band.
Differential Diagnosis:
Fibromyalgia – The symptoms of fibromyalgia include widespread bodily pains and fatigue. It affects all other tissues (muscle, bone, tendon, ligaments, and fat) and is more common in women. Tender spots may also form. Although patients may not exhibit jump symptoms when pressed or linked to pain maps, tender spots are distinct locations of tenderness over soft tissues that produce local pain and are tender to the touch. It can be challenging to distinguish between these two pain syndromes without a comprehensive examination by a qualified medical professional because their symptoms may overlap. Even so, they might interact and occur simultaneously.
Other ailments that feature trigger points and muscular soreness include:
Musculoskeletal Diseases
- Occupational myalgias
- Post-traumatic hyperirritability syndrome
- Joint dysfunction (osteoarthritis)
- Tendonitis and bursitis
Neurological Disorders
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Sphenopalatine neuralgia
Systemic Diseases
- Systemic lupus erythematosus (SLE)
- Rheumatoid arthritis
- Gout
- Psoriatic arthritis
- infections caused by bacteria, viruses, parasites, protozoa, and Candida albicans
- Lyme Disease
Hypoglycemia and Hypothyroidism
Heterotopic Pain of Central Origin
Axis II-Type Disorders
Psychogenic pain
- Painful behaviours
Management of Trigger Points:
Drugs
Over-the-counter treatments like Tylenol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) including aspirin, ibuprofen, and naproxen can help reduce milder types of pain. Acetaminophen and NSAIDs both alleviate discomfort from stiffness and muscular pains, and NSAIDs also lessen inflammation (irritation and swelling). Muscle relaxants, antidepressants (Cymbalta), anti-anxiety medications (Valium), NSAIDs (Celebrex), or a brief course of harsher painkillers (codeine), hydrocodone, and acetaminophen (Vicodin) may be prescribed by a doctor if over-the-counter medications are ineffective.
Injection at the Trigger Point (TPI)
A tiny needle is inserted into the patient’s active TrP during this surgery. The injection may contain a corticosteroid in addition to saline or a local anesthetic. In addition to relieving pain, the injection renders the TrP dormant. A short course of treatment will frequently provide long-lasting relief. In a single visit, multiple sites may be injected. A dry-needle method that doesn’t use medicine can be employed if a patient has a drug allergy.
Management of Physical Therapy
- Everyday variables that trigger the formation of TrPs should be minimized or removed if at all possible.
- education on lifestyle and posture, posture training,
- Self-massage, several times a day, and particularly rhythmic, one-way Deep Stroking Massage,
- Strengthening: solely isometric workouts at first, followed by isotonic ones,
- The phrase “ischemic compression technique” describes a therapeutic approach in which ischemia in the TrPt zone is produced by applying pressure for an extended period. This idea is dubious, though, because the TrP’s nucleus naturally exhibits significant hypoxia. Simons explained a comparable therapeutic approach that does not require further ischemia in the TrP zone (TrP Pressure Release). The amount of pressure ought to be just sufficient to cause the TrP zone’s tension to gradually subside without producing any discomfort. However, both methods demonstrate a notable improvement in the range of motion following therapy.
- Method of Taping,
- Applying the Spray and Stretch Method with ethyl chloride spray,
- Given that TrPs obstruct lymphatic flow, manual lymphatic drainage (MLD)
- Some particular methods include laser, ionophoresis, hot and cold packs, diathermy-electrotherapy, muscle energy technique (MET), myotherapy (MT), and neuromuscular technique (NMT).
Home advice for Trigger Points:
Learning to self-manage the disease is one of the greatest ways to deal with the trigger spots. Using trigger point techniques for self-massage therapy may be part of this. Included are these treatments:
- Applying compression using a back-robber to the points of the trigger.
- Pressing onto the trigger points by rolling over a tennis ball
- To assist smooth out fascial tissue, foam is rolled over the muscles.
- One thing is certain: active therapy programs that involve exercise and posture adjustment are better than passive ones for treating trigger points. See a physical therapist for a thorough evaluation of your condition and to find out how to manage your trigger points through self-care techniques.
- You can also perform these treatments at home, such as:
- As in a heating pad, heat. Ice or cold packs help some folks.
- Exercise, particularly aerobic exercises, increases oxygen delivery to the muscles, stretching exercises assist muscles in stretching, and weight-bearing exercises help strengthen muscles.
- OTC pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like naproxen or ibuprofen. If you are using NSAIDs or analgesics that your doctor has prescribed, avoid taking these medications.
- Breathing exercises, meditation, and yoga to stretch, reduce stress, and relax the muscles are examples of relaxation techniques.
- dietary adjustments Steer clear of recognized inflammatory foods.
- Soaking in warm water.
- massages.
- Each person has this pain ailment for a different amount of time. It might disappear with treatment in a day or a few weeks, but some people may need more time. Your general health is one of the factors that determine how quickly this discomfort goes away.
- Diet.
- quantity and caliber of sleep.
- If you have this trigger point in your calf muscles, take care of yourself. Maintaining your physical well-being through self-care practices may help you focus on managing your discomfort.
FAQs
How do you feel about trigger points?
Trigger points resemble tiny knots or pebbles just under the skin. Most people experience no pain or discomfort while pressing on the trigger site. However, trigger points can occasionally become extremely sensitive, and few people experience severe pain at their trigger point locations.
In what locations are trigger points found?
The central TrPs, which are found in the middle of an abdominal muscle belly where the motor endplate enters, are where myofascial trigger points primarily evolved. These perceptible nodules can develop in any specific site within any skeletal muscle in the body. They range in size from 2 to 10 mm.
Is it possible to apply massage to muscle knots?
Muscle knots can be healed with massage treatments. Massage therapy increases blood flow and circulation. can aid in releasing tense muscles and enhancing muscle function. This aids in reducing stiffness and soreness.
How are knots located by physical therapists?
Physical therapists are trained to detect knots by feeling for shoulder, neck, and back stress. By exerting deep compression with their thumb, fingers, or elbow and holding it for 20 to 30 seconds, they can release this tension.
How are knots located by physical therapists?
Physical therapists are trained to detect knots by feeling for shoulder, neck, and back stress. By exerting deep compression with their thumb, fingers, or elbow and holding it for 20 to 30 seconds, they can release this tension.
References
- Dr.Esha Patel. (2023, January 26). Trigger point – Cause, Symptoms, Treatment | Mobile Physio. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/trigger-point/#How_Do_You_Treat_a_Trigger_Point
- Physiotherapist, D. (2023, March 3). Trigger Points – Classification, Cause, Symptoms, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/trigger-points/#Differential_Diagnosis





10 Comments