Axonotmesis
What is an Axonotmesis?
The term “axonotmesis” describes the anatomical disruption of an axon that does not, or only partially, disturb the framework of connective tissue. Axonotmesis is a condition in which a peripheral nerve in one of the body’s limbs is injured.
This type of injury results in damage to the axons and their myelin sheath, but leaves the endoneurium, perineurium, and epidermis intact. With time, distal motor and sensory capabilities are lost completely, resulting in Wallerian degeneration from ischemia, or blood supply loss. Typically, a more severe crush or contusion than that which causes neuropraxia results in Axonotmesis.
Axonotmesis is primarily caused by a stretch injury. These strain injuries have the potential to break bones or dislocate joints, which can result in the tearing of peripheral nerves. If the exposed nerve axon does not cause acute pain, an individual can recognize a nerve injury by experiencing odd sensations in the affected limb.
A nerve conduction velocity (NCV) test may be requested by a physician to fully diagnose the problem. Electromyography, which is done after three to four weeks and is used to diagnose nerve injury, reveals symptoms of denervations and fibrillations, or abnormal connections and contractions of muscles. Regrowing the axon to the target muscle is necessary for this kind of nerve damage, and it takes time.
Pathophysiology of the Axonotmesis
Understanding the overall structure and function of peripheral nerves is an essential component of understanding axonotmesis. The myelin sheath, a protective covering, surrounds the axons that make up peripheral nerves. Rapid nerve impulse transmission depends on the myelin sheath. When an axon is injured but the surrounding connective tissues such as the endoneurium, perineurium, and epineurium remain intact, this condition is known as axonotmesis.
Axonotmesis most often results from traumatizing traumas such as crush or strain damage. Loss of sensory and motor functions may result from these injuries, which can impair the axon’s capacity to send messages. When an axon undergoes damage, a process known as Wallerian degeneration may take place. The axon that is farthest from the cell body degenerates throughout this process and is subsequently destroyed by macrophages. Axons are still alive and may even regenerate in their proximal region, which is the region nearest to the cell body.
Causes of the Axonotmesis
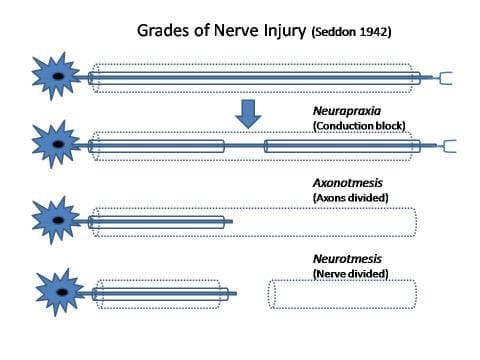
Peripheral nerve injuries such as axonotmesis are usually caused by percussion, crush, or strain traumas. The Seddon classification criteria have assigned this injury a second-degree categorization. Other factors are:
- Compression
- Traction
- Direct blunt injuries.
- Fractures
- Dislocations
- Contusions
- Injection of harmful chemicals.
Signs and Symptoms of the Axonotmesis
Depending on the location and severity of the nerve lesion, axonotmesis can manifest differently clinically. Typical signs and symptoms include:
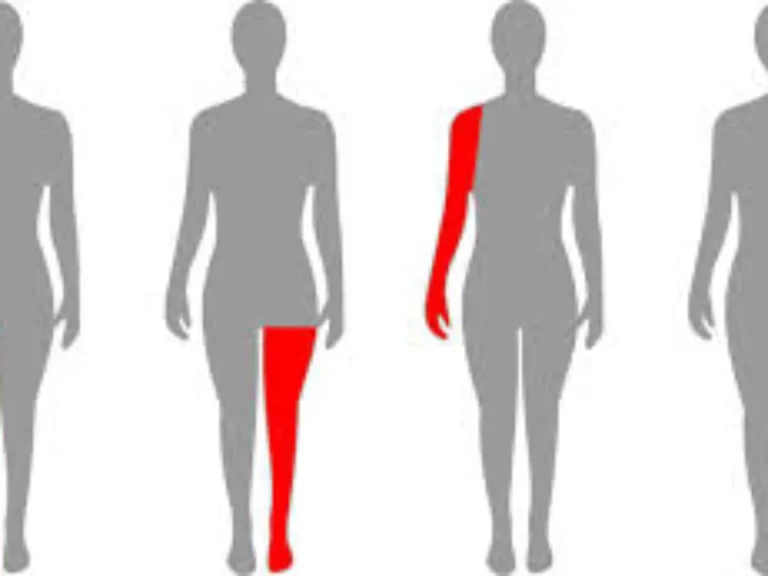
- Sensory Loss: Individuals may feel tingling or numbness in the places where the injured nerve innervates. Depending on the nerve implicated, a certain pattern of sensory loss is typically observed.
- Motor Dysfunction: Patients may suffer from weakness or paralysis in the muscles that the afflicted nerve supplies. This could lead to issues with coordination and the ability to move.
- Autonomic Dysfunction: Patients may suffer from abnormalities in blood flow regulation, sweating, or other involuntary activities if the damaged nerve has autonomic functions, although these are less common.
- Pain: Patients may have neuropathic pain, which is characterized by searing, shooting, or aching feelings, depending on the type of injury they sustained.
Diagnosis of the Axonotmesis
A combination of clinical assessment, neurophysiological testing, and imaging techniques is used to diagnose axonotmesis:
- Physical Examination: It is significant to perform a complete physical examination together with a thorough history. Assessing sensory and motor function as well as determining the pattern of abnormalities are the main goals of the clinical examination.
- Neurophysiological Tests: Electromyography (EMG) test and nerve conduction studies (NCS) are important for checking the level of nerve injury. These tests aid in distinguishing between neuropraxia, a less severe nerve injury where just the myelin sheath is affected, and other forms of nerve injuries such as axonal injury. The NCV study states that distal sensory-motor responses are absent in axonotmesis. An electromyography device is used in electromyography (EMG), a medical diagnostic procedure, to assess and record the electrical activity of skeletal muscles.
- Imaging Studies: To determine the amount of the damage and identify any structural damage to the nerve or surrounding tissues, imaging studies like MRIs and ultrasounds may be used for specific situations.
Treatment for the Axonotmesis
Axonotmesis can be treated in a variety of ways, which may involve conservative care, surgery, and rehabilitation:
Conservative Treatment:
To stop further damage, the affected area is usually immobilized and rested during the initial phase of treatment. Pain control and symptomatic therapy are also necessary components of treatment. One option for treating pain is to utilize analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or others.
Surgical Intervention:
Surgery might be required if conservative treatment seems to be failing or if there has been a large amount of damage. If there has been a major disruption in nerve continuity, procedures may involve nerve decompression or repair, in which the nerve is surgically repaired.
Physical Therapy for the Axonotmesis
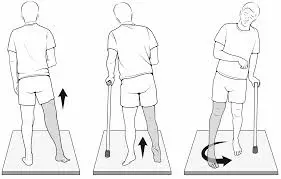
To recover, physical therapy rehabilitation is essential. Increases in strength, coordination, and function are the key goals of physical therapy. Physical therapy assists in the following:
- Pain relief
- Keep your range of motion intact.
- lowering the rate of muscle atrophy
- Education of Patients
- Utilizing assistive technology (Orthotic needs)
Occupational therapy may be required to assist patients to adjust to functional limitations and enhance their quality of life.
Prognosis
- When it comes to healing, the prognosis is typically favorable when proper care and rehabilitation are received. Some factors that influence the nerve’s ability to regenerate are the extent of the lesion, the patient’s age and general health, and the effectiveness of therapy.
- After an injury, nerve regeneration usually starts a few weeks to months later. The healing rate depends on how far the injury is from the site; axonal regeneration can happen as quickly as one inch every month. The recovery process can take range from six months to a year.
- Not every sufferer, though, will fully recover. Some may develop long-term issues such as residual weakness or sensory deficiencies. When nerve restoration is done early and there is less accumulation of scar tissue, the results are frequently better.
Summary
An important peripheral nerve injury known as axonotmesis is characterized by axon destruction that does not compromise the surrounding connective tissues. Optimizing patient outcomes requires a comprehensive knowledge of the cause of the disease, clinical symptoms, and suitable treatment options. To maximize healing and minimize long-term disability, early diagnosis, efficient treatment, and thorough rehabilitation are essential.
FAQs
What happens during axonotmesis?
A more serious kind of peripheral nerve damage called axonotmesis typically happens by pushing, stretching, or crushing. Issues in axonotmesis can affect the endoneurium and perineurium, but not the epineurium. The axon is detached from the soma, and the axon and the myelin sheath are damaged.
What are the three types of nerve injuries?
Classification of nerve injuries. Seddon identified three types of nerve damage:
neurotmesis
axonotmesis
neurapraxia.
How long does it take to recover from axonotmesis?
Sunderland II axonotmesis occurs when an axon is damaged while the endoneurial tube remains normal. A full recovery follows in 1-6 months on average. Sunderland III axonotmesis is caused by injury to the endoneurial tube; in this instance, recovery is less definite, with a partial return anticipated in 12 to 24 months.
Is surgery necessary for axonotmesis?
The number of damaged axons and the amount of scar formation at the site of nerve injury determine whether or not individuals with axonotmesis require surgical intervention.
How may axonotmesis be treated?
The gold standard for treating axonotmesis and neurotmesis is direct nerve restoration utilizing microsurgical procedures because this method provides endurance or continuity between the distal and proximal sections of the nerve.
References
- Chaney, B., & Nadi, M. (2023, September 4). Axonotmesis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK562304/
- Axonotmesis. (2023, July 5). Wikipedia. https://en.wikipedia.org/wiki/Axonotmesis
- Axonotmesis – Knowledge and References | Taylor & Francis. (n.d.). Taylor & Francis. https://taylorandfrancis.com/knowledge/medicine-and-healthcare/axonotmesis/
- axonotmesis. (n.d.). In Merriam-Webster Dictionary. https://www.merriam-webster.com/medical/axonotmesis



One Comment