Kyphosis
Defination
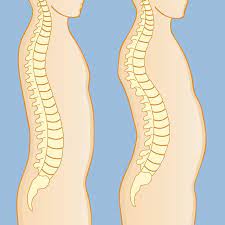
Kyphosis is a spinal condition that results in an excessive curve of the spine and an abnormal rounding of the upper back. Sometimes the condition is referred to as roundback or hunchback in the case of a severe curve. Although it can happen at any age, kyphosis is most common in teenagers.
Most of the time, there are no problems with kyphosis and no medical treatment is necessary. A patient may occasionally need to perform exercises or wear a back brace in order to strengthen their spine and correct their posture. However, in severe cases, kyphosis can result in breathing difficulties, severe spinal deformity, and pain. Surgery can be necessary for patients with severe kyphosis with the goal of reducing the excessive spinal curvature and improving their symptoms.
A kyphosis of 20 to 45 degrees should be the normal range for the thoracic spine, however, problems in posture or structure might cause a curve outside of this range. Doctors often use the term “kyphosis” to refer to the clinical disease of excessive curvature in the thoracic spine that results in a rounded upper back, even though the correct term for a curve that is more than normal (more than 50 degrees) is really hyperkyphosis.
Kyphosis severity varies. In general, the more severe the disease, the greater the curve. Those with milder curves may experience minimal back pain or none at all. More severe curvature may result in a noticeable hump on the patient’s back as well as major spinal deformities.
Anatomy
There are three segments to your spine. These segments make three natural curves when viewed from the side.
Lordosis is the term for the C-shaped curves found in the cervical (neck) and lumbar (lower back) spines.
Kyphosis is the term for the thoracic spine’s (the chest’s) reverse C-shaped curve.
Balance and maintaining an upright posture are made possible by the spine’s natural curvature. If any curve becomes larger or smaller, it becomes difficult to stand up straight and our posture appears unnatural.
The following are some of the smaller spine segments:
Vertebrae. Normally, the 24 small, rectangular vertebrae that make up the spine are placed on top of one another. Your back’s characteristic curves are the result of these bones joining together to form a canal that protects the spinal cord.
Intervertebral discs. Flexible intervertebral disks are located in between each vertebrae. They have a half-inch thickness and are spherical, flat, and smooth. Intervertebral disks cushion the vertebrae and absorb shock while walking and running.
Causes of Kyphosis
A healthy spine is made up of vertebrae, which resemble cylinders arranged in a column. When the back vertebrae begin looking like wedges, it is called kyphosis.
Vertebrae may change shape in the following ways:
Fractures. Spinal curvature may be caused by broken vertebrae. The most frequent type of fractures are compression fractures, which can happen in weaker bones. Often, mild compression fractures don’t show any symptoms at all.
Osteoporosis. Spinal curvature can result from weak bones, particularly if the weak vertebrae through a compression fracture. Older women and those who have used corticosteroids for a longer duration of time are more likely to develop osteoporosis.
Disk degeneration. Soft, round disks act as cushions between the spinal vertebrae. These disks flatten and decrease with age, worsening kyphosis frequently.
Other causes for kyphosis include the following: https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/kyphosis
- An infection (like tuberculosis)
- Neurofibromatosis is a condition where tumors grow out of nerve tissue
- Polio
- Muscular dystrophy (a collection of hereditary illnesses characterized by muscular weakening and tissue loss)
- Connective tissue diseases.
- Spina bifida: a congenital condition where the spinal canal and backbone fail to close before birth.
- Tumors
- Paget disease is a condition characterized by abnormal regrowth and breakdown of bone.
- Some endocrine (hormone) disorders
- Scoliosis (a spinal curvature that, when viewed from behind, can look like a C or S)
Types of Kyphosis
There are many types of kyphosis. The following three most frequently affect kids and young adults:
- Postural kyphosis.
- Scheuermann’s Kyphosis
- Congenital kyphosis
Postural Kyphosis
The most prevalent type of kyphosis, postural kyphosis, usually shows itself throughout adolescence. It is not linked to serious structural problems of the spine, although it is observed clinically as slouching or poor posture.
When asked to stand up straight, patients with postural kyphosis can often correct the normally round and smooth curve that results from the condition.
Postural kyphosis is more common in girls than in boys. It rarely is painful, and since the curve does not advance, issues with it in later life are unusual.
Scheuermann’s Kyphosis
Scheuermann’s kyphosis is similar to postural kyphosis in that it usually appears in adolescence. Postural kyphosis is less likely to cause a severe deformity than Scheuermann’s kyphosis.
The cause of Scheuermann’s kyphosis is a structural deformity in the spine. An X-ray taken from the side of a patient with Scheuermann’s kyphosis will reveal that three or more consecutive vertebrae have a more triangular shape rather than the typical rectangular shape.
The vertebrae wedge together near the front of the spine as a result of this abnormal form, which reduces the usual disk space and causes the upper back’s forward curve to be exaggerated.
Congenital kyphosis
Congenital kyphosis is a rare cause of hyperkyphosis, although it can be severely painful, rapidly progressing, and is more frequently associated with neurological problems than other types of kyphosis. Congenital kyphosis is classified into two types: failure of formation (Type 1) and failure of segmentation (Type 2).
One or more vertebral bodies will not develop as a result of the lack of development, leading to a kyphosis that will worsen as the child develops. the failure of segmentation occurs when two or more vertebral bodies fail to separate. typically, a child with this type of deformity will be diagnosed after they can walk. the most frequent cause of spinal cord compression from spinal abnormalities is congenital kyphosis.
Epidemiology
In general, hyperkyphosis becomes more common as people age, especially beyond the age of 40. In individuals 60 years of age and above, the frequency ranges from 20% to 40%. While males and females have been affected, women see an increased rate of rise, particularly following menopause. Age-related kyphosis is typically caused by underlying osteoporosis and/or fractures; however, only one-third of patients with severe kyphosis have vertebral fractures visible on radiographic examination.
A longitudinal study with a total of 100 healthy volunteers (females and males at least 50 years of age) found that the average thoracic kyphotic angle increased by around 3 degrees each ten years.
In the US, the prevalence of Scheuermann’s disease ranges from 0.4% to 8%, and men are nearly twice as likely to have it as women. The majority of cases get diagnosed between the ages of 13 and 16, with uncommon cases detected before the age of 10.
Pathology
Age-related kyphosis increases in young adults and teenagers, the kyphosis angle ranges from approximately 25° (range 20–29°) to approximately 38.5° (range 35–42°) in persons over 65 years of age 5, 7. Although there does not appear to be a gender preference, ethnicity may have an effect.
A kyphosis angle greater than 40° is usually considered the threshold for hyperkyphosis, while there is no published consensus. When using the >40° threshold, the incidence of hyperkyphosis is ~30% (range 20-40%) in people 60 years of age and older, and ~55% in people 70 years of age and older. In order to prevent overdiagnosis, some publications suggest a threshold of >50° 5 or >60°; however, an age-adjusted range between 20 and 60° may be more suitable.
Symptoms of Kyphosis
Depending on the cause and severity of the curve, kyphosis might present with different symptoms. These could consist of:
- Rounded shoulders
- A visible back hump
- Back Pain – Minor pain in the back
- Fatigue
- Stiffness in the spine
- Tight hamstrings (muscles on the back of the thigh)
Rarely, progressive curves over time may result in:
- Leg weakness, numbness, or tingling
- Sensation loss
- Changes to bowel or bladder routines
- Breathlessness or other breathing problems
Diagnosis
Physical and History
The most noticeable symptom of hyperkyphosis is a rounded back, which is a cosmetic deformity caused by the spine’s excessive forward curvature. As already mentioned, age-related kyphosis causes this deformity to manifest beyond the age of 40, whereas postural kyphosis (normal vertebral structures) and Scheuermann disease (vertebral structural deformity) cause the excessive curvature to become noticeable in young people.
Along with the outward appearance of the deformity, patients frequently experience fatigue, increased forward head position, fatigue, mild to severe pain in their backs, and uneven shoulder height. In more severe cases, patients may experience incontinence of the bowel or bladder, weakness, shortness of breath, and loss of sensation.
Generally, there are three components to the physical examination: palpation, range of motion testing, and observation. In severe cases, the upper back will appear rounded and frequently described as having a “hump” upon sagittal plane examination. In less severe cases, you might not notice the “hump” in the back. The paraspinal muscles are usually sensitive to the touch.
Particularly, Scheuermann’s disease is related to tight hamstrings. These muscles are considered “lumbar compensators” and can lead to overcompensation, which raises the risk of imbalance in these individuals. The typical values for the thoracolumbar spine’s range of motion are 30 degrees for extension, 90 degrees for flexion, and side bending and rotation.
Finally, for patients suffering from hyperkyphosis, it is critical to assess the nervous system. In most situations, there are no neurological symptoms, but in cases of severe kyphosis, there may be numbness, tingling, weakness, and incontinence of the bladder and bowel. In these situations, it is best to order an MRI in order to rule out cord compression.
Evaluation
As previously mentioned, a small degree of kyphosis is typical due to the structure and shape of the disc and vertebral bodies. On the other hand, we refer to hyperkyphosis when the kyphosis angle is greater than 40 degrees, which is the young adult’s 95th percentile.
The gold standard for objectively assessing kyphosis is a standing lateral spine X-ray. Particularly, in older patients, the patient may find comfort in lying down. To diagnose kyphosis based on lateral spinal X-ray analysis, one needs to calculate Cobb’s angle.
This can be achieved by locating the superior and inferior endplates of the vertebrae, which represent the curve’s starting and ending, respectively. The angle at which the superior and inferior endplates cross when a straight line is drawn through them is known as Cobb’s angle.
If radiographs cannot be obtained, there are other options. Radiographs can be replaced with the Debrunner kyphometer or the flexicurve ruler as valid methods for assessing hyperkyphosis. The two arms of the kyphometer, a protractor device, are positioned at the top and bottom of the thoracic region’s curvature. Next, the protractor is used to read the angle. The C7 and L5-S1 lumbosacral spaces are home to the moldable plastic flexicurve ruler.
The kyphosis index is then calculated by dividing the width of the thoracic curve by its length and multiplying the result by 100. A score higher than 13 is regarded as hyperkyphotic. This can be easily understood by recognizing that the index increases with increasing thoracic angle since it causes the thoracic width to widen and the thoracic length to heighten.
Treatment of Kyphosis
Non Surgical Treatment
Kyphosis treatment options may include the following:
Lifestyle changes. Maintaining a healthy weight can relieve certain symptoms and prevent pain.
Over-the-counter pain medications. stronger prescription painkillers, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin IB), naproxen (Aleve), or both.
Supplements of calcium and vitamin D. If you have a family history of osteoporosis, these medications can help Slow kyphosis progression.
Physical therapy Exercises to Help Reduce Kyphosis
Maintaining the health of your spine requires a certain degree of kyphosis or spinal curvature. However, maintaining a healthy degree of curvature in your spine can be facilitated by strengthening and extending the muscles that support your erect posture.
Arm raises

Your shoulder muscles will be strengthened and stretched as a result of this stretch.
Step 1: Adopt a standing position with your hands by your sides and your palms facing front.
Step 2 is to raise your arms and bend them at the elbows so that your palms face forward and your upper arms are parallel to the ground, imitating the shape of a goalpost. Hold for 5 to 10 seconds.
Step 3: Keep raising your arms until they are as high as you can reach, with your palms still pointing forward. After five to ten seconds, maintain this posture and then lower your arms.
10 times for a set, or a maximum of 3 times a day, repeat this exercise.
Shoulder Blade Squeeze
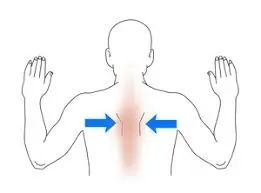
You can strengthen your upper back muscles and reduce tension with this exercise:
Step 1: Take a seat or stand up straight, pulling your shoulders back.
Step 2: Close your shoulder blades as tightly as you can, holding the position for 5 to 10 seconds. Release and repeat.
You can perform 2 sets of this exercise every day, between 3 and 5 repetitions per set.
Stretch the resistance band

Use a resistance band to increase the resistance during shoulder blade exercises. With your arms parallel to the floor, grasp both ends of the resistance band in front of you and extend it as far as is comfortable.
When doing the stretch, concentrate on using your shoulders, particularly your shoulder blades. After 5 to 10 seconds of holding the stretch, progressively release it. This exercise can be done in sets of 3 to 5 repetitions, with a maximum of 3 repetitions each day.
Push-ups

One of the easiest bodyweight workouts to build stronger arms, shoulders, and back muscles is the push-up.
Step 1: Place your hands on the floor, slightly to either side of your shoulders, and lie flat on your stomach.
Step 2: While keeping your toes or knees on the ground, gently raise your whole body off the ground. Try to maintain a straight back and legs.
Step 3: Lower yourself gently back to the ground and repeat.
Mirror image
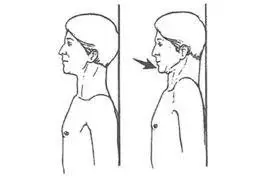
Just perform the opposite action of the posture you’re trying to fix for this exercise.
Step 1: Stand tall, preferably against a wall.
Step 2: Bring your head back precisely over your shoulders and tuck your chin gently.
Step 3: Drop and retract your shoulder blades. Hold for a total of thirty to one minute. Stop if you begin to experience pain.
Place a pillow behind you and press your head into it if it’s difficult to keep your chin tucked in while getting your head to touch the wall.
Superman

Step 1: With your hands out in front of your head, lie on your stomach.
Step 2: Lift both arms and legs toward the ceiling while maintaining a neutral head position and look down at the floor.
Step 3: Imagine stretching far away from your body with your hands and feet. Hold for three seconds, then ten times repeat.
Thoracic spine foam rolling
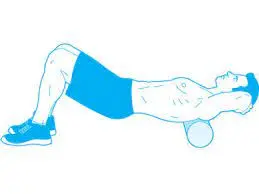
Step 1: Place a foam roller under your lower back while you are lying on the floor.
Step 2: Use the foam roller to gently massage your thoracic spine and back muscles by rolling up and down.
Head retraction
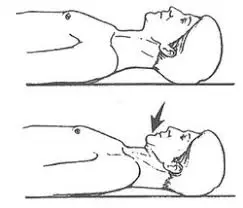
This exercise, which is performed while lying on the floor, is excellent for strengthening the neck muscles, which are frequently weak and stretched.
Step 1: Pull your chin back toward the ground like you’re trying a double chin.
Step 2: For fifteen seconds, hold. Five to ten times, repeat.
Bracing
Children who are still growing can benefit from the use of a Milwaukee brace or a supraclavicular brace, which can often even be used to treat kyphosis. An orthopedic expert prescribes the brace, which is manufactured by an orthotist.
For children who are actively growing and have kyphosis curves greater than 65 degrees, a brace is recommended. Usually, the brace is to be worn for 23 hours a day until the teenager’s growth is complete.
Surgical Treatment
Surgery is frequently advised for those who have congenital kyphosis.
Patients who have severe pain in the back or curves greater than 70 to 75 degrees associated with Scheuermann’s kyphosis may also benefit from surgery. Surgery may be necessary for patients with thoracolumbar curves, or lower back kyphosis if the curves are smaller and reach 25 to 30 degrees.
The most common surgical method for treating kyphosis is spinal fusion.
Spinal fusion has the following goals:
- Reduce the curve’s degree
- Avoid further curve progression.
- Continue to get better with time.
- Reduce severe pain in the back, if any is present.
Surgical Procedure
Welding is the process of spinal fusion. The main goal is to fuse the damaged vertebrae so that they grow into a single, strong bone. Because it stops motion between the afflicted vertebrae, fusion of the vertebrae will decrease the degree of curvature and may also aid with pain in the back.
During the treatment, the doctor will usually use metal screws and rods to assist put the vertebrae in better alignment. Safe partial correction, or reducing the curve but not necessarily normalizing it, is frequently the goal. The curvature should ideally be half as large as it was originally. Once the vertebrae are properly aligned, small pieces of bone called bone grafts are placed into the spaces between the vertebrae to be fused. Like a fractured bone healing, the bones grow together over time.
The amount of your child’s curve determines just how much of the spine gets fused. The joined vertebrae are limited to their curvature. The remaining spine bones are still movable and can help in rotation, bending, and straightening. Larger curves frequently necessitate the fusion of additional vertebrae, which reduces the number of movable vertebrae that are still able to bend and twist the spine.
Differential Diagnosis
Vertebral instability.
This usually happens as a result of a degenerative disease’s slow progression or an initiating event. Patients’ spines will be assessed for laxity in the surrounding muscles and for stabilization methods.
Scheuermann’s Disease
Scheuermann disease is a juvenile disease that typically manifests kyphotic abnormalities before puberty.
Ankylosing Spondylitis.
Reactive arthritis, inflammatory bowel disease, and psoriasis are among the major systemic diseases that are typically linked to AS, an inflammatory condition. Additionally specific to this illness are X-ray abnormalities that can help in diagnosis.
Osteoporosis
A gradual degenerative disease characterized by a loss of bone mineralization that affects all bones to variable degrees is called osteoporosis. MRI, X-ray, and bone scan results can be used to diagnose and qualify these findings.
Prognosis
Postural kyphosis.
Not progressive, not irreversible, and does not result in permanent deformity
Conservative treatment usually works when pain is present.
Scheuermann’s Kyphosis
Rarely is surgery necessary.
Conservative measures to relieve pain typically have an effect.
Severe curves (> 100 degrees) are extremely rare to cause cardiac problems.
Congenital kyphosis.
The prognosis and expected results are contingent upon the location and degree of kyphosis.
Results can range from complicated posterior spinal fusion and instrumentation to no treatment for every person.
If not identified and treated promptly, massive, progressive curves may lead to neurologic deterioration.
Complications
Persistent back pain: The incorrect curvature of the spine can strain the muscles and ligaments in the back, causing chronic pain and discomfort.
Breathing difficulties: In severe cases, the hunched position compresses the lungs, making deep breathing difficult. Breathlessness may result from this, particularly when exerting yourself.
Limited physical function: Having a rounded posture might make it difficult to move around and carry out daily tasks like bending over, tying shoelaces, and looking over your shoulder.
Digestive problems: In extreme cases, a severely hunched back may compress the abdominal organs, resulting in heartburn and constipation.
Neurological problems: A curved spine may compress the nerves that pass through the spinal canal, leading to pain that radiates down the legs, numbness, weakness, or even paralysis.
Body image problems: Kyphosis’s hunched appearance can make a person feel self-conscious and low in self-esteem.
Patient Education
In cases when kyphosis results in functional limits, patient education is essential for managing the disease. People should focus on conservative treatments including physical therapy, good body mechanics, and posture. Building muscle strength in the core may help maintain the stability of the spine.
In patients with age-related kyphosis, it’s critical to advise against flexion exercises, particularly for female patients, since studies have shown that flexion-induced movements can raise the risk of fractures when bone strength is compromised. Since the back extensor muscles are known to be weak in hyperkyphosis, the focus should be on extension-based activities to strengthen them.
When to consult a healthcare professional
If a person’s spine has a visible curve or they have chronic pain or stiffness, they should consult a healthcare professional. They are able to identify the root of the issue. A healthcare professional will be able to determine which type a patient has if they have kyphosis.
Postural kyphosis does not necessarily require therapy because it does not cause permanent abnormalities in the bones. It might only take physical activity to lessen the curve.
Treatment that is started early in the course of the disease is frequently helpful for congenital, age-related, or progressive forms of kyphosis. Whether or not surgery is performed, individuals should be routinely monitored to find out whether or not the curve is moving forward in their lifetime.
Conclusion
Excessive forward curvature of the spine, or kyphosis, is a curable disease that, unless it is severe, usually has no effect on a person’s daily activities. This problem can be treated before it worsens with an early diagnosis and course of treatment.
Your healthcare professional will discuss noninvasive treatments with you prior to surgery. You’ll need to monitor your posture even after therapy to make sure the curve doesn’t reappear. Consult a mental health professional if you feel self-conscious about the curve.
FAQ
What is the main cause of kyphosis?
Kyphosis can be caused by poor posture in childhood, unusually formed vertebrae, or developmental issues with the spine.
Is kyphosis serious?
Along with back pain, kyphosis may also result in Limited bodily functions. Weakened back muscles and trouble performing activities like standing up and sitting down are signs of kyphosis. The curvature of the spine might also hurt when you lie down and make it difficult to look up or drive.
What age does kyphosis start?
Although the actual cause of Scheuermann’s kyphosis in children is unknown, the condition runs in families. Primarily, the symptoms appear either during or following the growth spurt associated with puberty. When they are diagnosed, most children are between the ages of 12 and 15.
How painful is kyphosis?
Pain from kyphosis usually feels in the kyphosis’s localized area. In cases when the curvature is severe, the spinal cord may experience pressure and complications as a result of the nerves in the cord being compressed. Lower extremity weakness may result from this.
Can you live a normal life with kyphosis?
Kyphosis rarely results in health issues or requires medical treatment. But as a result, you could start to feel self-conscious about the way you look. Severe forms of kyphosis may result in pain or difficulty breathing. Surgery can be needed for severe kyphosis.
Can kyphosis be fully cured?
You might not have any symptoms in the early stages of kyphosis, and you might not require medical treatment. Kyphosis has a chance to worsen and result in a major spinal deformity if treatment is not given. Although kyphosis cannot be cured, treatment works to stop progressive curvature and relieve symptoms.
References
- Kyphosis – Symptoms and causes. (2022, June 18). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/kyphosis/symptoms-causes/
- Kyphosis: Symptoms, causes, exercises, and more. (n.d.). Kyphosis: Symptoms, Causes, Exercises, and More. https://www.medicalnewstoday.com/
- Lam, J. C., & Mukhdomi, T. (2023, August 8). Kyphosis – StatPearls – NCBI Bookshelf. Kyphosis – StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK558945/
- Kyphosis. (2021, June 1). American Academy of Pediatrics. https://doi.org/10.1542/9781610025058-12
- Kyphosis (Roundback) of the Spine – OrthoInfo – AAOS. (2020, August 1). Kyphosis (Roundback) of the Spine – OrthoInfo – AAOS. https://www.orthoinfo.org/en/diseases–conditions/kyphosis-roundback-of-the-spine/
- Kyphosis. (2023, October 11). Kyphosis | Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/kyphosis
- Exercises to Reduce Kyphosis. (2023, September 25). WebMD. https://www.webmd.com/back-pain/exercises-reduce-kyphosis
- Kyphosis Symptoms & Treatment | Aurora Health Care. (n.d.). Aurora Health Care. https://www.aurorahealthcare.org/services/aurora-spine-services/kyphosis
- Mayhew, P. (n.d.). Kyphosis | Radiology Reference Article | Radiopaedia.org. Radiopaedia. https://radiopaedia.org/articles/kyphosis
- C. (n.d.). Kyphosis: What Is It? Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17671-kyphosis
- Freutel, N. (2023, May 26). Kyphosis Exercises to Treat a Rounded Upper Back. Healthline. https://www.healthline.com/health/exercise-fitness/kyphosis-exercises#exercises-to-try






6 Comments