Lordosis
What is a Lordosis?
An abnormal inward curve of the lumbar spine is known as lordosis. However, the typical inward curve of the lumbar and cervical regions of the human spine is sometimes referred to by the terms lordosis and lordotic. In the same way, kyphosis is used to refer to an abnormal convex curvature of the spine. Kyphosis or kyphotic refers to the typical outward (convex) curvature in the sacral and thoracic regions. Greek lordōsis, from lordos (“bent backward”), is where the word originates.
Humans can more easily shift their weight across their pelvis due to lordosis in the spine. Compared to other primates, whose stiff spines force them to adopt an ineffective forward-leaning “bent-knee, bent-waist” gait, this allows a far more efficient walking gait. Therefore, one of the main physiological adaptations of the human skeleton that makes walking as energy efficient as it is is thought to be lordosis in the spine.
Anatomy of spine
The spine is a very complex mechanical structure that combines strength and stability with extreme flexibility. Physical demands are always placed on the typical spine, no matter what posture you’re in or what you’re doing, including sleeping.
The spine’s primary functions are listed below:
- Protect your internal organs, spinal cord, and nerve roots.
- Provide flexibility in movements.
- Maintain balance and structural support for upright posture. The weight of the head, shoulders, arms, and upper body is supported by the spine. The hips and legs then receive the weight of the upper body. The spine makes an effort to maintain a uniform distribution of body weight over the pelvis.
- This can relieve back pain and muscular fatigue by lessening the amount of work that the spinal muscles must perform.
- While the adult spine is normally balanced over the pelvis, maintaining an upright posture requires little effort from the muscles.
- When the spine tries to maintain an upright position, loss of spinal balance can cause stress on the spinal muscles and deformity.
Regions of the spine
In the spine, there are 33 vertebrae. The spine is separated into the following regions anatomically:
- The cervical spine, which consists of the top 7 vertebrae that make up the neck, is designated C1–C7.
- The 12 vertebrae in the thoracic spine, or upper back, are numbered T1 through T12.
- The 5 vertebrae of the lower back, or lumbar spine, are numbered L1 through L5.
- There are nine vertebrae that combine to form a single, solid bone that is the sacrum and coccyx (tailbone). the sacrum is referred to as S1.
The curves of the spine
The typical spine is a straight line with one vertebra directly on top of the other when viewed from the front or back. A scoliosis is a side-to-side curvature of the spine.
The typical spine has three progressive curves when viewed from the side:
The neck slopes backward in a condition known as lordosis.
The kyphosis of the thoracic spine causes it to bend upward.
There is lordosis in the lumbar spine as well.
The spine’s ability to carry the weight of the head and upper body and keep its equilibrium when standing up is helped by these curves.
Vertebrae
All vertebrae, from the cervical to the lumbar spine, share the same basic structures, even though their looks vary slightly. These structures are also named the same. The only cervical vertebrae that differ structurally in order to support the skull are the first and second.
An anterior and a posterior arch, together known as a foramen, are present in every vertebra. Every vertebral foramen serves as an outlet for the spinal cord.
The vertebral body is the name given to the anterior arch. Discs allow the spine to move and protect it from large loads by joining the vertebral bodies together. About 80% of the weight on the spine is supported by the discs and vertebral bodies together.
The posterior arch is made up of pedicles, laminae, and process.
Two little bony cylinders that protrude from the vertebral body are called pedicles. Nerve roots originate from the spinal cord between the pedicles of two vertebrae and travel out into the body. The pedicles can compress the nerve root and result in pain or numbness if the spine becomes unstable.
The posterior arch’s walls are made up of two flattened plates of bone called laminae. The laminae may thicken with time, a condition known as stenosis. Pain or numbness is caused by the thickening compressing of the spinal cord and/or nerves.
The laminae are the projection points for the articular, transverse, and spinous processes. Tendons and ligaments are attached to the processes. Posteriorly, the articular processes connect the vertebrae together.
Intervertebral Discs
Each vertebra from C2-C3 to L5-S1 has an intervertebral disc between them. They add up to one-fourth of the spinal column’s height. The discs allow the spine to move by acting as shock absorbers to the loads applied to it. There is little range of motion at a single disc level, but there is a considerable range of motion when the vertebrae and discs are connected.
The annulus fibrosis and the nucleus pulpous comprise the two halves of the intervertebral disc. The annulus fibrosis is the name for the disc’s outermost layer. It is made up of layers, or lamellae, of collagen and proteins.
The inner gel substance that the annulus fibrosis surrounds is known as the nucleus pulpous. It comprises roughly 40% of the disc. The lamellae contain this ball-shaped gel. Water, proteins, and loose collagen fibers compose the bulk of the nucleus. At birth, the nucleus contains over 90% water; by the time a person reaches their fifth decade, that percentage drops to roughly 70%.
The nucleus pulpous may be partially or totally squeezed through the annulus fibers as a result of injury or aging of the annulus fibrosis, causing the disc to bulge and allowing disc material to exit the disc. Pain may be caused by compression of the spinal cord or nerves by the protruding disc or nucleus material.
The discs are supplied by blood during their early years of life. Discs progressively stop receiving blood in their second and third decades, at which point they become avascular. The disc starts to age, or degenerate, at this point. More than 95% of persons will have disc degeneration by the time they are 50 years old. The disc starts to get smaller and lose water. There is a reduction in the spine’s capacity to absorb trauma and range of motion. This could cause damage to the vertebrae and nerves, and the aging disc itself could cause pain.
Nerve Roots and the Spinal Cord
The brain and spinal cord are the two parts that constitute the central nervous system. The brain stem is directly below the spinal cord. It passes through the opening at the base of the skull known as the foramen magnum.
The spinal cord is a complex structure that carries data from the body’s external components—skin, muscles, ligaments, and joints—to the brain, the body’s central “computer,” via the sensory tracts. There, data are broken down, and fresh information—like the ability to move muscles—is transmitted via the spinal cord’s motor tracts.
The caudal equine, a group of nerves that go from the conus medlars to the sacrum, is where the spinal cord branches off at the L1 vertebral level, where the conus medullar is located. For the purpose of taking a spinal fluid sample or injecting drugs, anesthetics, or radiologic materials for an MRI, CT scan, or x-ray, a needle can be safely placed into the conus medullaris nerve region since the nerves swim freely in spinal fluid.
Causes of Lordosis
Posture
Long periods of sitting or standing in an unnatural position can cause poor posture, which in turn can lead to lordosis. It overstresses the natural curves of the spine, resulting in excessive lower back arch and an exaggerated inward curve called lumbar lordosis.
Osteoporosis
The presence of diseases or disorders affecting the integrity of the vertebrae itself, such as osteoporosis, can weaken the spine’s bones and risk its structural integrity.
The condition known as osteoporosis, which causes a loss of bone density, primarily affects women as they age and experience changes in hormone levels and bone density associated with menopause.
Trauma
Abnormal spinal curvatures like lordosis can be caused by trauma, such as accidents or traumas. The spine’s alignment can be disrupted by a severe impact or fractures that change the vertebral structures, which can result in excessive or insufficient curvature.
Muscular Dystrophy
Over time, muscles degrade and become weaker due to genetic conditions such as muscular dystrophy. It may have an effect on posture, movement, and muscle tone, which may change the curvature and alignment of the spine.
Spondylolisthesis
When one vertebra slips over the other, usually forward over the one below, it is called a spondylolisthesis. This may have an effect on the position of the spine, changing its curvature possibly resulting in lordosis.
Obesity
As previously mentioned, some lifestyle decisions, including not maintaining a healthy weight, can eventually have negative effects on the spine.
Not only does carrying excess weight apply strain on the spine’s joints, but it can also lead to people leaning backward excessively in an attempt to improve their balance, which often has an adverse effect on posture and the proper positioning of the spine.
Surgery
Lordosis may be unintentionally caused or made worse by spinal surgery. Surgical procedures can cause abnormal curvatures in the vertebrae, which may change spinal posture and perhaps result in disorders like lumbar lordosis.
Lifting Heavy Objects The Wrong Way
You may have heard the saying, “Lift with your legs, not your back.” It’s sound advice. Poor lifting techniques can strain the back, causing problems with the muscles, spine, and other physiological systems. As overstressed muscles constrict, they may lose flexibility, develop poor posture, and cause pain. Your spine’s structure may also be affected by tight muscles pulling against it.
Discitis
A herniated intervertebral disc may be the cause of lordosis. In particular, an infection of the discs—typically from bacteria that have been introduced to other bodily parts—causes discitis. It usually happens after surgery or an injury.
Types of lordosis
1. Lumbar lordosis
The term lumbar lordosis describes the natural curvature of the lower spine; however, when it becomes exaggerated or straightened, resulting in symptoms such as back curvature, it becomes important to understand the meaning and treatment options for lumbar lordosis, particularly for those with severe lordosis seeking to correct the condition.
A lumbar lordosis definition is typically used to identify this medical condition, which is defined by an exaggerated inward curve of the lower spine and can arise from a number of different causes. It’s crucial to know how to treat hyperlordosis, or excessive lumbar lordosis, for the purpose of managing the symptoms and selecting the best course of action for reducing pain while improving spinal alignment.
2. Hyperlordosis
The possible causes of hyperlordosis include obesity, discitis (infection-related inflammation of the intervertebral disc area), benign juvenile lordosis, and hyperkyphosis (a spine curvature disorder characterized by an unusually rounded thoracic curvature). Rare disorders such as Ehlers-Danlos syndrome (EDS), in which certain joints throughout the body are problematically far more flexible than normal, often to the point of partial or full dislocation, may also be contributing causes. Because of this hyper-extensibility, it is also rather typical, if not the usual, for some of the muscles around an unstable joint to contract in an attempt to counteract the instability.
Swayback typically refers to an almost opposite postural misalignment that can first look quite similar. Other names for excessive lordotic curvature, or lumbar hyperlordosis, include “hollow back” and “saddleback” (after a sickness that resembles it and affects some horses). Pregnancy, high visceral fat, and tight lower back muscles are common causes of lumbar hyperlordosis. Lumbar hyperlordosis can be brought on by vitamin D deficiency in youngsters known as rickets.
3. Hypolordosis
Hypolordosis arises from the Greek terms “lordosis,” which means “bending backwards,” and “under.” The natural lordosis of the spine flattens in a person with hypolordosis. Adverse spinal tension develops when the spine loses one or more of its normal curves, placing strain on the frontal plane of the spine (discs and vertebrae).
An excessively flat spine unnaturally elongates the posterior back muscles; it can also shorten the hamstrings and pull on the anterior hip flexor muscles, elongating them unnaturally. This can lead to pelvic tilt, a condition in which the front of the pelvis lifts up while the back of the pelvis is lowered. Adverse spinal tension compresses the discs and vertebrae.
The body might try to keep its balance as unnatural structural changes occur by means of muscular contractions and relaxations that occur throughout the body. This is the body’s natural response to uneven stresses brought by spinal diseases such as hypolordosis.
4. Cervical lordosis
The term “cervical lordosis” describes the cervical spine’s natural curvature in the neck. A healthy cervical spine develops a soft “C” at the top of a healthy spine, which forms a “S” shape from top to bottom.
This curve allows appropriate neck movement and bending in addition to supporting the head’s weight and keeping it balanced over the body. It also helps in shock absorption and helps the spine remain stable and structural. Exaggeration of this curve can have an effect on the neck’s tendons, ligaments, muscles, bones, nerves, and spinal cord. If you want to avoid harm and other issues, you need to take care of the condition.
When there is either a clear lack of curvature (hyperlordosis) or an abnormal, excessive inward curve (hyperlordosis), the condition is referred to as “cervical lordosis.” The cases where the curve is growing in the incorrect direction are less frequent. Reverse cervical lordosis is the term for this disorder. These cases also include a bend, either to the left or right.
5. Postural Lordosis.
This is frequently caused by being overweight and having unconditioned stomach and back muscles. Excessive weight in the front (stomach region) causes the back to go forward. The spine curves forward due to the force of weight when the back and stomach muscles are weak and unable to maintain the spine.
6. Congenital Lordosis
A shock or damage to the spine’s connecting links (pars) might cause it to break (fracture), resulting in pain in the lumbar spine. Children frequently get them from sports-related accidents. Children who are struck by cars or who fall from high places may show this.
There may also be a defect in the way the links develop during growth, resulting in them being misshaped and weak. They may experience a spondylolysis, or break in the bone connection, as a result of repeated actions that strain these weak linkages.
Whatever the cause of the break, it requires rest and limited movement to heal. If not, the vertebrae (spine blocks) may shift forward over time, pinching nerves in the spine. Leg pain, tingling, numbness, weakness, and dysfunction can happen from this.
7. Post-surgical lordosis
An abnormal curvature of the spine that results from surgery, usually involving the spinal column, is called post-surgical lordosis. The natural alignment of the spine can be changed by surgical operations, leading to an excessive or insufficient curvature. Pain, discomfort, and a reduction in spinal function may result from this.
Adequate rehabilitation, follow-up, and post-operative care are essential for monitoring and controlling any changes in spine curvature, ensuring the best possible outcome, and reducing risks.
8. Neuromuscular lordosis
Serious spinal disorders such as spina bifida or severe muscular dystrophy are associated with neuromuscular lordosis or NML. Bracing or postural adaptation is unlikely to be effective in treating NML; instead, invasive surgery is needed.
The majority of the time, an underlying genetic disease that causes the pelvis to deviate from its natural vertical alignment and lie flat is the cause of neuromuscular lordosis.
Those who believe they may have neuromuscular lordosis should get medical attention right away because of the severe symptoms connected to this type of lordosis.
Symptoms of Lordosis
Depending on where they are located, the stomach and buttocks may protrude due to lordosis. A person’s appearance may change due to lordosis, however symptoms are rarely present. But in more severe cases, lordosis symptoms may involve the following:
- Pain in the muscles in the shoulders, neck, and upper back
- neck or back pain
- swayback appearance (exaggerated posture with a more pronounced belly and buttocks)
- a space between your lower back and the floor when you’re on your back
- numbness
- tingling
- Weakness
- Difficulty maintaining muscle control (the curve makes the neck or back muscles work harder).
- Sciatica, or pain radiating into the feet and legs
- Weakness in bladder or bowel control
- electric shock pain
Lordosis in Children
Children frequently develop lordosis for unknown reasons. This condition is known as benign juvenile lordosis. It occurs as a result of weak or tight muscles surrounding your child’s hips. As your children become older, benign juvenile lordosis usually goes away on its own.
Lordosis may also indicate a hip dislocation, particularly in children who have experienced a car accident or fallen.
Other disorders of the neurological system and muscular issues are typically linked to lordosis in youngsters. These uncommon conditions consist of:
- cerebral palsy
- myelomeningocele, a hereditary disorder in which the spinal cord sticks through a gap in the backbones.
- muscular dystrophy, a group of hereditary conditions that result in weakened muscles.
- A genetic disorder called spinal muscular atrophy results in involuntary movements.
- arthrogryposis, a condition affecting the joints that is present from birth which restricts their range of motion.
Lordosis in pregnant women
Back pain is common in pregnant women, and they can also show lordosis symptoms, such as a protruding abdomen and buttocks. However, research indicates that lordosis during pregnancy is actually your spine realigning to reposition your center of gravity.
Your body’s altered blood flow could be the cause of your overall back pain, which will most likely go away following delivery. muscular dystrophy, is a group of hereditary conditions that result in weakened muscles
Diagnosis of hyperlodosis
It might be difficult to measure and diagnose lumbar hyperlordosis. The traditional approach of measuring segmental lumbar lordosis may become more challenging if interbody fusion obliterates vertebral end-platemarkers. Finding a reliable and accurate method to measure segmental lordosis at the L4–L5 and L5–levels is important since these levels are frequently involved in fusion surgeries or arthrodesis and they also contribute to normal lumbar lordosis. An unusually large lower back arch and the appearance of bulging up the buttocks and stomach are outward signs of hyperlordosis.
A physical examination and imaging tests are usually used in the diagnosis of lumbar hyperlordosis.
History and Physical Examination
During a physical examination, your doctor may ask you to do specific movements to measure your range of motion and flexibility in addition to looking for indications of an atypical curvature of the lower back.
Physical examination findings associated with lordosis may include:
- Visible spine curvature: Whether the patient is seated or standing, an excessive lordotic curve may be visible.
- Pelvic tilt: A patient with lordosis may have a forward-tilted pelvis that is noticeable when they stand.
- Difficulty performing particular movements: Lordosis can make it difficult to perform movements that require bending forward or backward, such as reaching or lifting.
Imaging tests
X-ray
X-rays are used to measure lumbar curvature. Stagnara et al. proposed a typical range of 20° to 60° for the lordotic curvature on a lateral X-ray, measured from the inferior endplate of T12 to the inferior endplate of L5. A measurement range of 40° to 60° between the upper endplate of Th12 and the upper endplate of S1 has been suggested by the Scoliosis Research Society.
Individual research has indicated normal ranges up to about 85°, even with different reference sites.In general, it is more noticeable in women. Through puberty and the early adult years, it remains largely unchanged, but in older adults, it declines.
Bone scans.
Nuclear imaging techniques such as bone scans are used to evaluate degenerative and/or arthritic changes in the joints, identify tumors and diseases of the bone, and establish the underlying cause of bone pain or inflammation. The purpose of this examination is to rule out fractures and infections.
Magnetic resonance imaging, or MRI.
This diagnostic process creates highly detailed pictures of the body’s organs and structures using a computer and big magnets. The purpose of this test is to rule out any related disorders of the nerves and spinal cord.
CT (computerized tomography) scan.
X-rays and computer technologies are combined in this diagnostic imaging process to create horizontal, or axial, images (commonly referred to as slices) of the body. A CT scan produces detailed images of any region of the body, such as the bones, muscles, fat, and organs. more information may be seen with CT scans than with regular X-rays.
Treatment
Chiropractic treatment for lordosis
The pull on the muscles and the balance of the joints can be significantly changed by realigning the spine with chiropractic adjustments. This may significantly improve function and dynamics while also greatly relieving any lordosis-related pain. Patience and physical activity can eventually reduce the strain on hyperlordosis.
Postural changes are required to help make Chiropractic adjustments last longer. Lordosis is a chronic, long-term condition, thus this is necessary to rebalance the stresses on the spine. The Alexander Technique is a very useful way to learn about the changes in the pelvis caused by lordosis. It can also assist in learning how to balance more easily and with less strain on the spine, as well as when to rest the spine because lordosis will cause the back to wear out more rapidly.
Bracing
The process of bracing involves the use of specialized equipment to support and adjust lordotic spinal curvature. Braces are designed to correct posture, reduce pain, and stop abnormal curvatures from getting worse. They are prescribed based on the patient’s needs and the severity of the disease. When braces are used consistently under the supervision of a professional, they can help control lordosis and improve spinal health.
The Boston brace is an external plastic brace designed to reduce disc strains resulting from herniated discs. It can be built with a minor amount of lordosis. If Ehlers-Danlos syndrome (EDS) is the cause, getting fitted appropriately for a personalized brace could help prevent strain and reduce the frequency of instability.
Anti-inflammatory Medications
Pain and inflammation associated with lordosis can be controlled using anti-inflammatory treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs). By blocking chemicals that cause inflammation, they reduce discomfort. Under medical supervision, NSAIDs that are prescribed or purchased over the counter can be utilized. However, because of possible adverse effects, prolonged use needs to be closely watched. Getting advice from a medical expert guarantees that medications are used appropriately and safely.
Lifestyle Modifications
Among the lifestyle adjustments for lordosis are:
- Maintaining good posture.
- Exercises that support the spine can help you stay active.
- Reaching and keeping a healthy weight.
- Ergonomics practice.
- Avoid spending too much time sitting down.
These changes support spinal health and reduce pain brought on by abnormal curvatures.
Surgical treatment
Surgery is usually only considered a last resort for severe cases of lordosis that have not improved with conservative measures like bracing, medication, or physical therapy. The primary objectives of lordosis surgery are to:
- Reduce the spine’s curvature
- Realign the spine.
- Improve your posture.
- Decrease pain
- Stop the curvature from getting worse.
Surgical techniques for lordosis vary based on the underlying etiology and degree of the deformity. The following are a few typical procedures:
Spinal fusion: It is the most common surgery for lordosis. Using metal implants or bone transplants, a spinal fusion procedure permanently joins two or more vertebrae. It helps in reducing the spine’s curvature and stopping the abnormal movement of the vertebrae.
Disc replacement: In certain cases, an artificial disc can be used to replace a damaged disc that is causing lordosis. This can help in returning the disc space to its typical height and functionality.
Kyphoplasty: Although it can occasionally result in lordosis, this technique is mostly done for spinal compression fractures. A balloon is introduced into the collapsed vertebra and subsequently inflated to restore its height during kyphoplasty. The vertebra is then stabilized by injecting cement into it.
Physical therapy exercises
1. Plank

Step 1: Eight hours is the world record for the longest plank. Fortunately, the workout doesn’t require you to hold it for so long in order to work! You can actually only continue for 10 to 15 seconds.
Step 2: Similar to a push-up, the plank involves bringing your elbows straight underneath your chest rather than resting on your hands.
Step 3: After kneeling, bend forward and rest your elbows on the ground just beneath your shoulders.
Step 4: Raise your knees off the ground and extend your feet backward. Keep your neck in line with the rest of your spine and make sure your back is straight. For the necessary amount of time, maintain the posture and tighten your core muscles.
2. Side plank

Step 1: Similar to the original plank, but with one side-only balance.
Step 2: Place your feet together and lie on your side on the floor, facing sideways.
Step 3: Raise your body up until your elbow, which is directly below your shoulder, is supporting your weight.
Step 4: Maintain a straight body by tightening your core muscles and lifting your hips. Your body should slope from your shoulders to your feet.
Step 5: Hold in this position without lowering your hips.
Step 6. Repeat on the other side.
3. Pelvic tilt with exercise ball
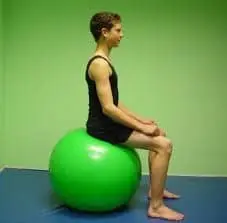
- Step 1: Position yourself on a ball so that your feet are flat on the ground and your legs are at a 90-degree angle.
- Step 2: Maintain a straight spine and rounded shoulders.
- Step 3: Flex your abdominals tightly and tilt your hips forward.
- Step 4: As you extend your tailbone, tilt your hips backward.
- Step 5: Maintain your shoulders back while you gently move back and forth.
- Step 6: Do this three sets of ten times.
4. Superman

Step 1: Stretch your arms out in front of you while lying face down on your stomach.
Step 2: To keep your hips grounded, simultaneously raise your arms, legs, and torso off the ground.
Step 3: Hold for at least two seconds.
Step 4: Slowly lower yourself back down.
Step 5: Do this three sets of ten times.
5. Crunches

Step 1: Place your feet level on the floor and bend your legs while lying flat on your back.
Step 2: Raise your head, neck, and torso off the ground by folding your arms across your chest.
Step 3: Take time to hold, then bring yourself back down.
Step 4: Repeat.
6. Quadruped arm opposite leg raises

Step 1: Lean forward, kneel on the ground, and place your hands palm down on the ground.
Step 2: A straight back, knees below hips, and palms directly below shoulders are the three things you should check.
Step 3: Raise one arm while raising the other until both are parallel to your spine and protrude straight out of your body.
Step 4: Lower your arm and leg gradually until you are back where you were before.
Step 5: Repeat with the opposite arm and leg.
7. Dead bug

Step 1: Rest your back flat on the ground.
Step 2: Raise your arms straight up out of your body and extend them through the air as well.
Step 3: Lift one leg such that it forms a 90-degree angle concerning your body.
Step 4: Lower it gradually until it reaches the beginning position.
Step 5: Repeat after switching legs.
8. Hip bridge

Step 1: With your feet flat on the ground, your knees bent and lifted, and your arms by your sides, assume a position of lying on your back.
Step 2: Try to maintain your leg in vertical alignment with your knee and maintain a hip-distance apart stance.
Step 3: Your hips should rise as a result of flexing your glutes and through your heels. Aim to draw a diagonal line connecting your shoulders and knees.
Step 4: Hold for a few seconds before descending once more.
Step 5: Do this for 3 sets of ten times each.
Complications
Spinal Stenosis: Abnormal lordosis may be a contributing factor in spinal stenosis, a condition in which the spinal cord and nerves are compressed, resulting in pain, weakness, and numbness in the limbs.
Bad Posture: An excessive amount of lordosis can aggravate pain and discomfort by placing additional strain on the spine and surrounding muscles.
Decreased motion: In severe situations, aberrant lordosis can limit spinal motion, making it difficult to carry out daily activities and decreasing quality of life.
Back pain: Prolonged lower back discomfort can result from excessive lordosis, which puts stress on the spine’s muscles, ligaments, and discs.
Muscle Imbalance: An excessively tight or weakening of some muscles can result from abnormal lordosis, which can aggravate existing pain and tension.
Degenerative Disc Disease: Pain, stiffness, and decreased flexibility are the characteristics of degenerative disc disease, which is caused by excessive lordosis and promotes the degeneration of the spinal discs.
Poor Posture: An excessive amount of lordosis can aggravate pain and discomfort by placing additional strain on the spine and surrounding muscles.
Reduced motion: Severe cases of abnormal lordosis can cause a restriction in spinal motion, which can lower the quality of life and make it harder to carry out daily tasks.
Neurological Symptoms: Abnormal lordosis can compress nerves in the spinal canal, resulting in neurological symptoms such as tingling, weakness, and loss of control over the bladder or bowels.
Impact on Breathing: Severe cases of aberrant thoracic spine lordosis may compress the chest cavity, impairing lung function and respiratory efficiency.
Differential diagnosis
Metabolic disorders: Many types of metabolic diseases, including osteoporosis and Paget’s disease of the bone, can damage the spine’s integrity and structure, resulting in an unnatural curvature.
Pregnancy: Increased lumbar lordosis to support the growing fetus and a shifting center of gravity are two reasons why the hormonal and biomechanical changes that occur during pregnancy might occasionally result in transient lordosis.
Obesity: Carrying too much weight can strain the spine and cause compensatory curvatures, such as lordosis.
Trauma: Injuries to the spine, pelvis, or lower limbs can disturb the spine’s natural posture and contribute to lordosis.
Inflammatory conditions: Rheumatoid arthritis and ankylosing spondylitis are two examples of inflammatory diseases that can impact the spine and cause abnormal curvature.
Congenital lordosis: People who are born with abnormalities in their spine or pelvis may naturally be predisposed to lordosis.
Muscle imbalances: An exaggerated lumbar curve may result from weakness or tightness in specific muscle groups, such as the hip flexors or abdominal muscles.
Spinal conditions: Spondylolisthesis (when one vertebra slips forward over the one below it), lumbar disc herniation, and spinal stenosis (narrowing of the spinal canal) can all cause aberrant spinal curvature.
Postural lordosis: Incorrect alignment when standing or sitting for extended periods of time can lead to or worsen lordosis.
Neuromuscular disorders: Disorders affecting muscle tone and control, such as spinal muscular atrophy, muscular dystrophy, or cerebral palsy, may result in lordotic posture.
Prognosis
The underlying cause and degree of symptom severity determine the prognosis for lumbar lordosis. For example, children with mild lordosis may eventually recover without treatment, but those with severe lordosis may need surgery. On the other hand, successful treatments might result in a decrease in symptoms or, in certain cases, a “cure” or a return of lordosis to normal or nearly normal.
Prevention of lordosis
Often, people can avoid hyperlordosis by adopting good posture. People can avoid putting stress on their necks, hips, and legs by maintaining proper spinal alignment, which could cause issues down the road. People should heed the following advice in order to help prevent this condition:
- If the patient has worries about maintaining their weight, they need to begin a weight loss program. If people need assistance getting started, they may consult with a doctor.
- People must take short breaks throughout the day to stand up and stretch while they are sitting for extended periods of time.
- A person must occasionally shift their weight from one foot to the other or from their heels to their toes if they must stand for extended periods of time.
- Their feet have to be flat on the ground while they sit.
- When they sit, they have to support their lower back with a pillow or rolled towel.
- They have to wear low-heeled, comfortable shoes.
- They have to follow the exercise program they choose.
When should I visit my healthcare professional?
It’s a good idea to discuss your back pain with your healthcare professional.
Discuss with your clinician how frequently you will require follow-up appointments. They’ll let you know how frequently they should examine your spine’s curve to see if anything has changed.
If you experience tingling or shocks, or if you lose feeling in any of your hands or feet, you should see your doctor immediately once. These can be signs of more severe problems with your spinal cord.
Conclusion
The most suitable course of treatment for lordosis will depend on a number of factors, including the patient’s age, the severity of their disease, and the underlying reason for their excessive lumbar lordosis. The term “swayback” refers to the appearance of an exaggerated inward C-shaped curvature of the lumbar spine, which can cause the buttocks and abdomen to protrude excessively.
Since the spine plays such a significant role in human anatomy, disorders like lordosis, also known as hyperlordosis, which causes the spine’s natural curves to disappear, can cause a wide range of symptoms, especially if they are not addressed.
When it comes to maintaining spinal health and function, prevention is key. This can be achieved by leading a spine-friendly lifestyle, which includes understanding the ergonomics of heavy lifting, keeping a healthy weight and activity level, and practicing good posture.
When a spinal disorder such as kyphosis, discitis, or spondylolisthesis develops lordosis, the underlying cause of the lordosis must be treated proactively in order to treat the linked complication of excessive lumbar lordosis simultaneously.
FAQ
What is the main cause of lordosis?
Excessive weight in the front (stomach region) causes the back to go forward. The spine curves forward due to the force of weight when the back and stomach muscles are weak and unable to maintain the spine.
Is lordosis normal or abnormal?
The lumbar spine’s inward curve, or lordosis, is located directly above the buttocks. A mild case of lordosis is normal. We refer to excessive curvature as swayback.
Is lordosis painful?
Lordosis can cause symptoms in the neck and lower back. This may result in the spine being overly compressed, which would cause pain and discomfort. If left untreated, a severe case could affect your movement. The severity of the curvature and the cause of the lordosis determine how the condition is treated.
Is lordosis a birth defect?
A spine deformity is called lordosis. It occurs when the lower back’s vertebral bones flex inward more than usual. A child who is born may have lordosis. Additionally, it could develop as a result of another health problem.
What should I do if I have lordosis?
Persons of any age can be affected by lordosis. The problem may be treated conservatively with medication, physical therapy, braces, and weight loss. If the curvature is significant and producing other symptoms, surgery might be required.
What muscles are weak in lordosis?
Lordosis is generally caused by an imbalance in the muscles that surround the pelvic bones. A higher pelvic tilt can limit lower back movement. This is caused by weak hip flexor muscles, which raise the leg forward, and tight back extensor muscles, which arch the back.
Can lordosis be corrected?
Exercise are the most effective technique to relieve symptoms such as back and neck pain, but it cannot reverse the curvature or cure lordosis. Your posture can be improved by strengthening your glutes (the muscles in your butt), hamstrings, hips, and abs.
References
- Lordosis. (2024, January 31). Wikipedia. https://en.wikipedia.org/wiki/Lordosis
- Spinal Anatomy – The American Center for Spine and Neurosurgery — ACSN. (n.d.). ACSN. https://www.acsneuro.com/resources/anatomy-spinal
- Brahmbhatt, B. (2023, September 6). Lordosis: Types, Causes, Symptoms & Effective Treatments. https://www.physiotattva.com/blog/lordosis-types-causes-symptoms-effective-treatments
- C. (2023, January 3). Lumbar Lordosis: What Is It & What Causes Lumbar Lordosis? CLEAR Scoliosis Institute. https://clear-institute.org/blog/lumbar-lordosis/
- Spotting the Symptoms of Lordosis | Jason Lowenstein, MD. (n.d.). Dr. Jason Lowenstein | Scoliosis & Spinal Deformities Surgeon. https://jasonlowensteinmd.com/spotting-the-symptoms-of-lordosis/
- Nalda, T. (2023, March 7). What Is Hypolordosis? Cervical and Lumbar Lordosis Treatment. Dr. Tony Nalda. https://drtonynalda.com/hypolordosis/
- Nalda, T. (2024, April 11). What Is Lumbar Lordosis? Causes, Symptoms, and Treatment. Dr. Tony Nalda. https://drtonynalda.com/lumbar-lordosis/
- Nalda, T. (2023, March 7). What Is Hypolordosis? Cervical and Lumbar Lordosis Treatment. Dr. Tony Nalda. https://drtonynalda.com/hypolordosis/
- Phillips, J. (2024, April 13). Cervical Lordosis Treatment. Scoliosis. https://scoliosisinstitute.com/cervical-lordosis-treatment/
- Lordosis. (n.d.). https://www.nationwidechildrens.org/conditions/lordosis
- What is Lordosis of the Spine, Types, Symptoms, Treatments. (2024, April 5). https://www.anahana.com/en/physical-health/what-is-lordosis
- Srivastava, S. (2022, November 14). Lordosis – Meaning, Causes, Symptoms, Pictures, Treatment. https://www.hexahealth.com/condition/lordosis#symptoms-of-lordosis
- Gabbey, A. E. (2023, April 24). What Causes Lordosis? Healthline. https://www.healthline.com/health/lordosis#in-children
- Harrison, D. (2023, September 26). Lumbar Lordosis: Definition, Causes, Symptoms, Diagnosis, and Treatment. Spine Info. https://www.spineinfo.com/conditions/lordosis/lordosis-definition-causes-symptoms-diagnosis-and-treatment/
- Philadelphia, C. H. O. (n.d.). Lordosis. Children’s Hospital of Philadelphia. https://www.chop.edu/conditions-diseases/lordosis
- Lumbar lordosis or hyperlordosis – Back Care Clinic. (2023, March 19). Back Care Clinic. https://backcareclinic.co.uk/lumbar-lordosis-or-hyperlordosis/
- U. (2020, February 12). Lordosis Exercises: Back Relief & Core Strength – UPRIGHT Posture Training Device. UPRIGHT Posture Training Device. https://www.uprightpose.com/blog/lordosis-exercises-back-relief-core-strength/
- Davis, C. P. (2023, July 20). Lordosis Causes, Symptoms, Treatment, Prevention. MedicineNet. https://www.medicinenet.com/lumbar_lordosis_lower_spine/article.htm#what_is_the_prognosis_for_lordosis
- A., & Doctors, A. (2022, December 6). Hyperlordosis : Exercises, Symptoms, Causes, Treatment and Prevention. Apollo Hospitals Blog. https://healthlibrary.askapollo.com/hyperlordosis-exercises-symptoms-causes-treatment-and-prevention/
- Gabbey, A. E. (2023, April 24). What Causes Lordosis? Healthline. https://www.healthline.com/health/lordosis#when-to-see-a-doctor
- Nalda, T. (2024, April 16). Lordosis Treatment: Can It Be Corrected? [BEST TREATMENT]. Scoliosis Reduction Center. https://www.scoliosisreductioncenter.com/blog/lordosis-treatment