Ulnar Nerve
Introduction
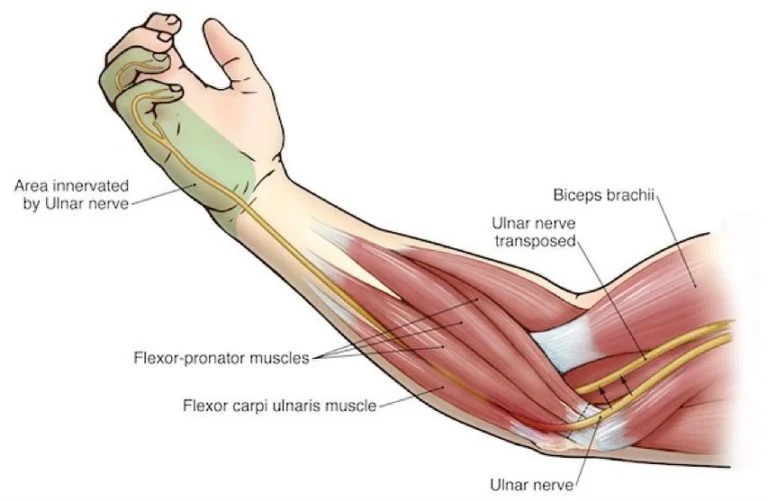
The ulnar nerve is a major peripheral nerve that runs from the neck down to the hand, playing a crucial role in movement and sensation. It controls fine motor functions in the hand and provides sensation to the ring and little fingers. Often referred to as the “funny bone” nerve, it is vulnerable to compression, especially at the elbow or wrist, leading to conditions like ulnar neuropathy.
The ulnar nerve travels distally from its origin into the hand via the axilla, arm, and forearm. It is a mixed nerve that supplies sensory information to the hand’s skin and motor innervation to several forearm and hand muscles.
Since the ulnar nerve innervates the great majority of the intrinsic hand muscles, it can be generically referred to as the nerve of the hand. Its superficial route and clinically evident significance in hand function make it one of the upper limb’s most clinically significant nerves.
You can move your hand, forearm, and several fingers thanks to the ulnar nerve. From the elbow to the hand, your forearm is extended. Additionally, the brain receives sensory data from the ulnar nerve, including touch, temperature, and pain.
When the ulnar nerve is under pressure, ulnar nerve entrapment happens. It may result in weakness and discomfort in the hands and fingers.
Ulnar nerve root value
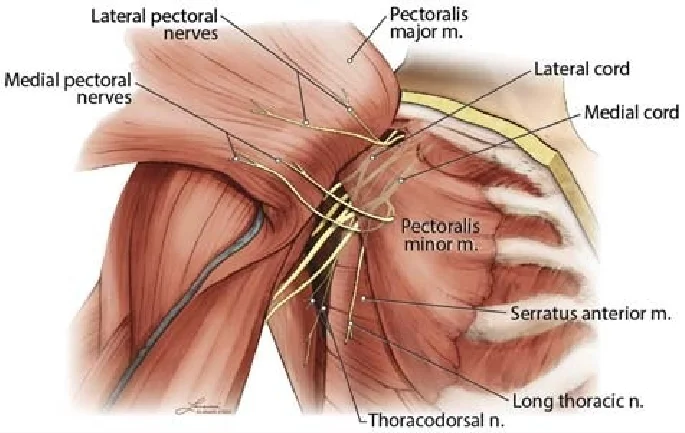
The ulnar nerve originates from the C8 and T1 nerve roots of the brachial plexus, specifically from the medial cord. It provides motor and sensory functions to parts of the forearm and hand, including intrinsic hand muscles and the medial aspect of the hand (ring and little fingers).
Structure
Most of the hand and a portion of the forearm are motor innervated by the ulnar nerve. It provides the medial forearm, medial wrist, and medial one-and-a-half fingers with sensory cutaneous innervation. The hypothenar muscles (opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi brevis) and the flexor carpi ulnaris and flexor digitorum profundus in the forearm receive motor innervation from the ulnar nerve and its branches. The third and fourth lumbricals, dorsal interossei, palmar interossei, adductor pollicis, flexor pollicis brevis, and palmaris brevis are all motor innervated by the ulnar nerve in the hand.
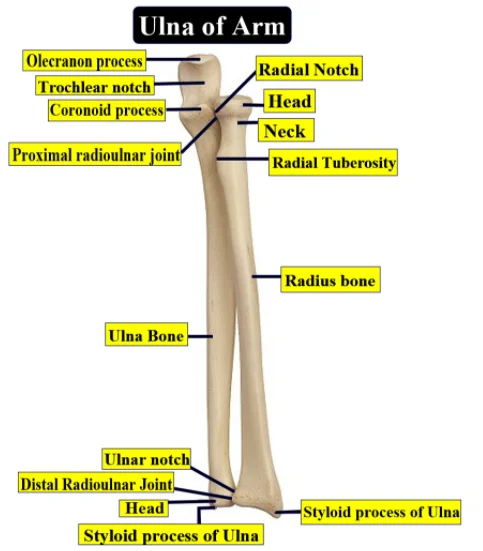
Sensory and motor fibers from the C8 and T1 dorsal rami are carried via the ulnar nerve. Through the medial intermuscular septum, also known as the arcade of Struthers, the nerve travels down the medial arm from the anterior to the posterior compartment. The internal brachial ligament, medial intermuscular septum, and medial head of the biceps combine to produce the arcade. After passing posterior to the humerus’ medial epicondyle, it releases its first branch, which gives the elbow joint proprioception.
The ulnar nerve crosses Osbourne’s ligament (retinaculum between the two heads of the flexor carpi ulnaris muscle) at the distal elbow. It extends superficially to the flexor retinaculum, passing via the forearm’s flexor and pronator muscles and into the wrist. Guyon’s canal, a fibro-osseous tunnel created by the pisiform and hook of the hamate, is where the ulnar nerve enters the hand. The palmar cutaneous (nerve of Henle) and dorsal cutaneous branches originate from the ulnar nerve in the hand. To provide sensation to the dorsal hand, the dorsal cutaneous nerve splits into radial and ulnar branches.
Function
Almost all of the hand’s tiny muscles are controlled by the ulnar nerve. Despite starting in the armpit, the ulnar nerve doesn’t accomplish anything until it reaches the forearm.
As a motor (moving) nerve, the ulnar nerve activates muscles in the forearm, hand, and fingers so you can:
- Straighten and bend the ring and pinky fingers.
- Hold and grasp objects.
- Use your fine motor skills to write with a pen, button a blouse, or flip through magazine pages.
The ulnar nerve is a sensory nerve that provides sensation to the;
- The pinky finger.
- The ring finger’s side nearest to the pinky finger.
- The pinky side of the hand’s palm and back.
Course & Innervation
Arm
The ulnar nerve travels distally from the medial cord through the axilla, medial to the axillary artery. It descends on the arm’s medial aspect, medial to the biceps brachii muscle and the brachial artery. The nerve enters the posterior compartment in the midsection of the arm by penetrating the medial intermuscular septum. Here, the nerve passes beneath the arcade of Struthers in 70–80% of individuals and goes anterior to the medial head of the triceps brachii muscle. From the medial head of the triceps to the medial intermuscular septum, there is a narrow, aponeurotic band.
The ulnar nerve then enters the anterior compartment of the forearm through the groove between the medial epicondyle and olecranon. Subcutaneous and easily perceptible, the ulnar nerve is located posterior to the medial epicondyle. In this area, it is frequently referred to as the “funny bone”. In the arm, the ulna nerve normally has no branches.
Forearm
The cubital tunnel, which is superficial to the posterior and oblique bands of the ulnar collateral ligament, is where the ulnar nerve exits the arm. The olecranon, medial epicondyle, and an arcuate ligament—a fibrous band connecting the two heads of the flexor carpi ulnaris muscle—all encircle this cubital tunnel. Here, the elbow joint receives articular branches from the nerve. Between the humeral and ulnar heads of the flexor carpi ulnaris, the ulnar nerve extends into the anterior compartment of the forearm.
Over the flexor digitorum profundus muscle and deep to the flexor carpi ulnaris muscle, the ulnar nerve descends on the medial surface of the forearm. The ulnar artery, which runs lateral to the nerve, exits lateral to the flexor carpi ulnaris near the wrist. Both structures, which are solely covered by skin and fascia, enter the hand just lateral to the pisiform bone and travel superficially to the flexor retinaculum (transverse carpal ligament).
The ulnar nerve in the forearm produces two muscular branches: the ulnar (medial) portion of the flexor digitorum profundus and the flexor carpi ulnaris. The median nerve supplies the remaining muscles of the anterior compartment of the forearm as well as the lateral half of the flexor digitorum profundus muscle. Furthermore, the palmar cutaneous nerve and the dorsal cutaneous nerve are two cutaneous branches that originate from the ulna nerve in the forearm. The hand receives sensory innervation from these nerves.
Hand
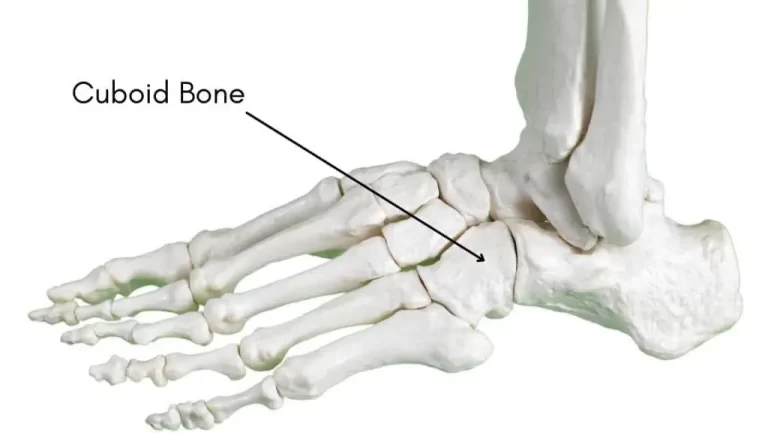
The Guyon’s canal, also known as the ulnar canal, is a groove between the pisiform and the hook of the hamate that is crossed by the palmar carpal ligament and the point at the wrist where the ulnar nerve and artery enter the hand.
Here, the nerve divides into superficial and deep branches to innervate the hand both sensory and motor.
Innervation
Motor Innervation
forearm
- FCU
- FDP ring and small
thenar
- adductor pollicis
- deep head of flexor pollicis brevis (FPB)
fingers
- interossei (dorsal & palmar)
- 3rd & 4th lumbricals
hypothenar muscles
- abductor digiti minimi
- opponens digiti minimi
- flexor digiti minimi
Sensory Innervation
- sensory branches of the ulnar nerve
- dorsal cutaneous branch
- palmar cutaneous branch
- superficial terminal branches
Muscle supplies
The flexor muscles of the forearm, such as the flexor carpi ulnaris and flexor digitorum profundus, are innervated by the ulnar nerve. Additionally, it innervates the hand’s intrinsic muscles, such as the lumbricals, palmaris brevis, interossei, and hypothenar. The palmaris brevis muscle, the ulnar proper nerve, the fourth common digital nerve, and the hypothenar muscles are all innervated by the superficial branch of the ulnar nerve in the hand. The third and fourth lumbrical muscles, the adductor pollicis, the medial head of the flexor pollicis brevis, the hypothenar muscles, the opponens digiti minimi, and the interosseous muscles are all innervated by the deep branch.
Branches
There are often no significant branches of the ulnar nerve in the arm. The articular and muscular branches, as well as the palmar and dorsal cutaneous branches, are produced by the nerve in the forearm. The ulnar nerve in the hand has two terminal branches: the superficial branch and the deep branch.
Articular branches
The ulnar nerve produces articular branches that innervate the elbow joint as it travels through the cubital tunnel between the medial epicondyle and olecranon.
Muscular branches
In the proximal forearm, the ulnar nerve gives rise to two muscular branches. The medial half of the flexor digitorum profundus and the flexor carpi ulnaris receive motor innervation from these.
Palmar cutaneous branch
Around the middle of the forearm, the ulnar nerve gives birth to the palmar cutaneous branch. This nerve penetrates the deep fascia in the distal forearm after traveling via the ulnar artery. The skin at the base of the medial palm, which is situated above the medial carpal bones, receives sensory innervation from it.
Dorsal cutaneous branch
The dorsal cutaneous branch of the ulnar nerve enters the distal forearm, near the wrist. This nerve enters the medial portion of the hand’s dorsum by passing through the deep fascia and traveling posteriorly, deep to the flexor carpi ulnaris. It divides into two or three dorsal digital nerves here to supply feeling to the skin on the medial side of the hand’s dorsum as well as the proximal areas of the little finger and half of the ring finger, which are the medial 1½ digits.
Superficial branch of ulnar nerve
The superficial branch of the ulnar nerve provides sensory innervation to the medial palmar skin and the front part of the ulnar 1½ digits, which includes the little finger and half of the ring finger. Additionally, it provides motor innervation to the palmaris brevis muscle in the hypothenar area of the hand. It frequently splits into two palmar digital nerves after emerging from the ulnar nerve immediately distal to the pisiform bone.
Deep branch of ulnar nerve
The ulnar nerve’s superficial and deep branches both come from the same area of the nerve. It runs beside the deep palmar branch of the ulnar artery between the hypothenar region’s muscles and into the deep aspect of the plan. The great majority of hand muscles are motor innervated by this nerve. These consist of the deep heads of the flexor pollicis brevis and adductor pollicis, the medial two lumbricals, all three palmar and four dorsal interossei, and the hypothenar muscles (abductor, flexor, and opponens digiti minimi).
All of the intrinsic hand muscles, except for the LOAF muscles (lateral two lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis), as well as the medial half of the flexor digitorum profundus, receive motor innervation from the ulnar nerve.
The following parts of the hand get sensory input from the ulnar nerve:
the palmar and dorsal surfaces of the neighboring palm and medial 1½ digits.
cutaneous layer on the hand’s medial side.
Examination
Depending on where the injury occurs along the nerve’s path, ulnar nerve injury can be caused by various factors, most frequently near the elbow. Compression at Guyon’s canal of the wrist can cause motor and sensory deficiencies in the hand, damage at the elbow can cause cubital tunnel syndrome, and proximal injury to the lower trunk of the brachial plexus can cause Klumpke palsy.
A brachial plexus injury to the lower trunk manifests as Klumpke palsy. An upward force on an infant’s arm or upward traction on an adult’s arm are the most frequent causes of lower trunk injuries. A heavy birth weight baby or a short birth canal may cause traction of the baby’s abducted arm during a traumatic vaginal delivery, which can also result in injury. A full claw hand is a clinical manifestation of Klumpke palsy, which is characterized by a functional impairment of the intrinsic hand muscles. Clinical observations include wasting of intrinsic hand muscles (lumbricals, interossei, thenar, and hypothenar muscles) with flexion of the distal and proximal interphalangeal joints, hyperextension of the MCP joint due to flexor loss, and radial deviation of the wrist due to flexor carpi ulnaris loss. Strap hanger’s syndrome is another name for this condition.
Loss of sympathetic input from T1 can result in Horner syndrome, which includes ptosis, miosis, and anhydrosis. Unopposed parasympathetic input to the eye causes pupil contraction.
The area close to the elbow is where ulnar nerve injuries occur most frequently. Anatomical injury from an elbow joint synovitis, soft tissue mass, osteophyte infection, or medial epicondyle fracture might result in nerve disease. Compression from extended elbow flexion, such as during sleep, exercise, driving, typing, or phone conversations, can also harm the nerve. Cubital tunnel syndrome is a peripheral neuropathy brought on by repeated trauma or chronic compression of the ulnar nerve at the elbow between the olecranon process of the ulna and the medial epicondyle of the humerus.
The cubital tunnel retinaculum has congenital laxity, which causes the ulnar nerve to become hypermobile. When the elbow is flexed, this may result in anterior dislocation and recurrent subluxation. Because of the frequent contact across the medial epicondyle, repetitive stress at this site may cause inflammation.
Additionally, ganglion cysts, external nerve compression, Guyon’s canal compression, and local trauma can all result in ulnar nerve impingement at the wrist. Guyon’s canal is a fibro-osseous tube created by the pisiform and hook of the hamate. Within the canal, the ulnar nerve splits into deep and superficial branches. Bicyclists who experience excessive pressure from their handlebars and prolonged compression while typing at a desk can also induce nerve compression at the wrist.
With a comprehensive history, musculoskeletal examination, and neurological examination, ulnar nerve damage can be diagnosed. Nonetheless, nerve conduction tests and EMG might be utilized as a supplement to identify and pinpoint the lesion.
The following clinical characteristics can be used to describe ulnar nerve damage.
flattening of the forearm’s medial border and loss of feeling at the fourth and fifth digits’ distal interphalangeal joints
reduction in hypothenar prominence
lack of thumb adduction and loss of finger abduction
pronounced clawing of the fourth and fifth fingers
minor trophic, vasomotor, and sensory alterations in the fourth and fifth digits
Neuro exam
Weakness:
- Flexion of the wrist
- The little finger’s flexion
- The index and little fingers are abducted.
- Thumb adduction.
Reduced feeling
- The medial 1-and-a-half fingers’ palmar surface
- The dorsal side of the medial 1-and-a-half fingers
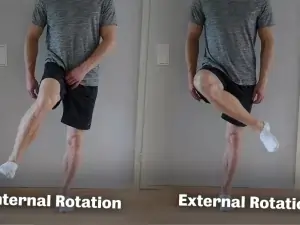
Neurodynamic
The patient is placed in a supine position for the ulnar nerve upper limb neurodynamic test (ULNT3). Until symptoms appear, the joints are gradually pushed to the end of their range. Patients should be told to report any pain, tingling, or strain that appears anywhere in the arm or neck.
The sequencing of ULNT3:
- Girdle depression of the shoulders
- Abduction of the shoulders
- External rotation of the shoulders
- Extension of the wrist and fingers
- Flexion of the elbow
- Abduction of the shoulders
Froment’s Sign
A test for ulnar nerve palsy, especially adductor pollicis paralysis, is called Froment’s sign:
By holding a piece of paper between their thumb and index finger, the patient is instructed to pull the paper away.
With a thumb adduction, they ought to have no trouble holding the paper there.
When the patient is unable to adduct the thumb, the test is considered affirmative. Instead, in an attempt to keep their grip on the paper, they bend their thumb at the interphalangeal joint.
Clinical Importance
Ulnar Nerve Palsy
Elbow damage
Medial epicondyle-level trauma (such as a single medial epicondyle fracture or a supracondylar fracture) is the mechanism of injury. The cubital tube might compress it as well.
Motor functions:
It affects every muscle that the ulnar nerve innervates.
Wrist flexion is still possible, although it is accompanied by abduction (since the medial half of the flexor digitorum profundus and the flexor carpi ulnaris are paralyzed).
Because the interossei are paralyzed, fingers cannot be abducted or adducted.
The paralysis of the medial two lumbricals and hypothenar muscles impairs the movement of the fourth and fifth fingers.
Because the adductor pollicis is paralyzed, the patient will have a positive Froment’s sign and impaired thumb adduction.
Sensation loss will occur throughout the regions innervated by the ulnar nerve as all sensory branches are impacted.
Characteristic indicators include hypothenar eminence wasting, positive Froment’s sign, and the inability of the patient to hold the paper between their fingers.
Damage to the Wrist
The mechanism of injury involves lacerations on the anterior wrist.
Motor functions:
The hand’s intrinsic muscles are the only ones impacted.
Because the interossei are paralyzed, fingers cannot be abducted or adducted.
The paralysis of the medial two lumbricals and hypothenar muscles impairs the movement of the fourth and fifth fingers.
Because the adductor pollicis is paralyzed, the patient will have a positive Froment’s sign and impaired thumb adduction.
Sensory functions: The dorsal branch remains intact, while the palmar and superficial branches are typically cut off. There is just a sensory loss on the palmar side of the medial one-and-a-half fingers.
When your ulnar nerve becomes inflamed or compressed (squeezed) near the inside of your elbow, it is known as Cubital Tunnel Syndrome.
Compression of the distal ulnar nerve at the wrist level as it passes through the ulnar tunnel, also known as the Guyon canal, is known as Guyon canal syndrome.
Characteristic indicators include hypothenar eminence wasting, positive Froment’s sign, and the inability of the patient to hold the paper between their fingers.
Claw hand
A disease known as claw hand malformation causes the finger to bend like a claw. Depending on the source, it might impact all of the fingers or just a few. One or both hands may be affected by the malformation, which typically results in bent or twisted fingers. A hand deformity known as claw hand occurs when the intrinsic muscles of the hand weaken, causing the metacarpophalangeal (MCP) joints to hyperextension and the interphalangeal (IP) joints to flex. Patients with neurological abnormalities that weaken or paralyze their intrinsic finger muscles may try finger extension and develop claw finger deformity. After intrinsic muscular palsy, the deformity is typically not immediately noticeable.
Claw Hand deformity can be:
When it affects every finger, it is considered complete and is caused by both Ulnar and Median Nerve Palsy.
Known as an isolated Ulnar Nerve Palsy, it is incomplete or partial when it only affects the ulnar two digits.
wasting of the hypothenar and interosseous muscles.
numbness in the affected nerve.
incapacity to abduct and adduct fingers while extending the IP joints.
The lumbricals of digits 4 and 5 are paralyzed, causing the extensors and flexors digitorum profundus to contract without resistance.
Surgical Considerations
The elbow in the cubital tunnel is the most typical location for ulnar nerve entrapment. Orthopedic procedures such as cubital tunnel decompression and potential ulnar nerve transposition are very prevalent. Osbourne’s ligament (cubital tunnel retinaculum) and the deep layer of the aponeurosis of the two heads of the flexor carpi ulnaris muscle make up the cubital tunnel. The proximal ceiling of the cubital tunnel, Osbourne’s ligament, keeps the nerve from subluxing when the elbow is flexed.
Osbourne’s fascia is cut during surgical decompression for cubital tunnel syndrome to alleviate pain and paraesthesia brought on by nerve damage. Another suggested surgical procedure is to move the nerve from the arcade of Struthers to the flexor carpi ulnaris. Just proximal to the medial epicondyle of the humerus, the internal brachial ligament, medial head of the triceps, and medial intermuscular septum create the arcade of Struthers. Compression of the ulnar nerve may also occur here.
Incidental injury to the ulnar nerve during carpal tunnel release surgery is another surgical concern. A little incision is made close to the wrist crease during surgery for carpal tunnel syndrome. To release the median nerve’s compression, the surgeon will cut through the wrist’s soft tissues and down the transverse carpal ligament.
Because the deep motor branch of the ulnar nerve runs along the hamate carpal bone just medial to the carpal tunnel, damage to the branch may result from this dissection. The incision must stay in line with the ring finger’s radial border, even though ulnar nerve injury is an uncommon side effect of carpal tunnel release surgery.
FAQs
What signs point to ulnar nerve damage?
Weakness or tenderness in the hand.
tingling in the fourth and fifth fingers as well as the palm.
Sensitivity to cold.
Tenderness in the elbow joint.
What is the best treatment for ulnar nerve damage?
Ulnar Nerve Pain Relief Techniques
Medications. Nonsteroidal anti-inflammatory drugs can help reduce pain and inflammation. …
splinting. The afflicted part can be supported and immobilized by wearing a brace or splint.
Physical therapy. …
Cold or heat therapy. …
Transcutaneous electrical nerve stimulation (TENS).
What is the recovery of the ulnar nerve?
It might take up to five years to fully heal from ulnar nerve injury. When motor loss is thought to be irreversible following nerve repair, tendon transfer should be taken into consideration as a backup option.
What is the best exercise for the ulnar nerve?
Can you fix your ulnar nerve without surgery?
Surgery is typically not necessary to treat ulnar nerve compression. Your NYU Langone physician might suggest that you avoid activities that exacerbate your symptoms and rest the afflicted hand and elbow.
Referencess
- TeachMeAnatomy. (2024b, October 4). The ulnar Nerve – course – motor – sensory – TeachMeAnatomy. https://teachmeanatomy.info/upper-limb/nerves/ulnar-nerve/
- Woon, C., MD. (n.d.-b). Ulnar nerve – Anatomy – Orthobullets. https://www.orthobullets.com/anatomy/10108/ulnar-nerve
- Ulnar nerve. (2023b, July 5). Kenhub. https://www.kenhub.com/en/library/anatomy/the-ulnar-nerve
- Professional, C. C. M. (2025d, January 24). Ulnar nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/21664-ulnar-nerve


2 Comments