Ulna Bone
Introduction
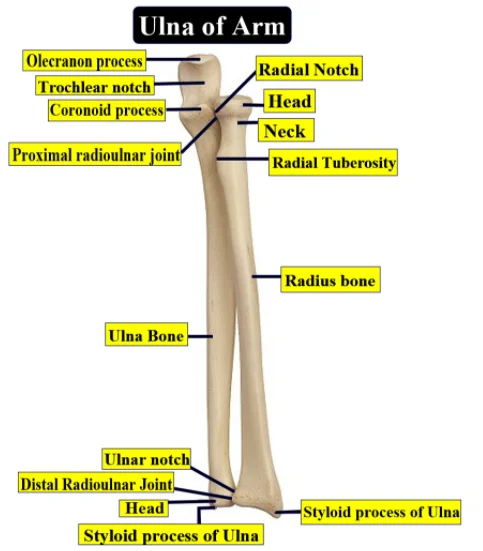
The ulna bone is one of the two bones in the forearm, the other bone is the radius. It is located on the medial side of the forearm when in the anatomical position (with the palms facing forward). The ulna is primarily responsible for forming the elbow joint with the humerus and articulates with the radius to allow for the movements of the forearm and wrist.
Because some fractures are diagnostic based on where they occur within the ulna and where the broken segments end up, common disorders have a connection to the bone.
Structure and Function
The olecranon process, a bony structure on the ulna, begins near the elbow. Its proximal and posterior ends have severe curvatures, and it is curved forward. The “hinged” ulnohumeral component of the elbow joint is formed by the articular surface of the proximal ulna, a notch in the olecranon along the volar surface. The olecranon and olecranon fossa work together to control forearm flexion and extension while preventing hyperextension.
A point from the proximal and anterior sides of the ulna is called the coronoid process. It inserts into the humerus’s coronoid fossa with a small upward arch. The brachialis muscles may now be inserted because of the coronoid process’s surfaces. The most medial position of the medial ulnar collateral ligament attachment to the anterior bundle of the coronoid process is known as the sublime tubercle. The articulating surface of the radius is headed by the radial notch, a little depression lateral to the coronoid process. The forearm’s supination and pronation are facilitated by the proximal radioulnar articulation, which also permits the radial head to rotate the proximal ulna.
As it descends distally, the ulna’s body features many surfaces and boundaries. This border is the source of the flexor digitorum profundus and the pronator quadratus muscles. The pronator quadratus and the flexor digitorum profundus originate from this boundaryThe dorsal border starts posterior to the olecranon process and continues down to the styloid process.
The flexor digitorum profundus and the pronator quadratus originated from the volar, or anterior, surface of the ulna, which is larger proximally than distally. Between the middle and upper thirds of the ulna is a gap that is referred to as the nutrient canal. Here, a network of blood veins extends into the medullary cavity and crosses the bone’s shaft. The dorsal surface, consisting of the bone’s posterior and lateral sides, is where the anconeus and supinator muscles are implanted in the attachments of the extensor indicis, supinator, abductor pollicis longus, and extensor pollicis longus. Only the flexor digitorum profundus has an extra origin location on the medial surface of the ulna.
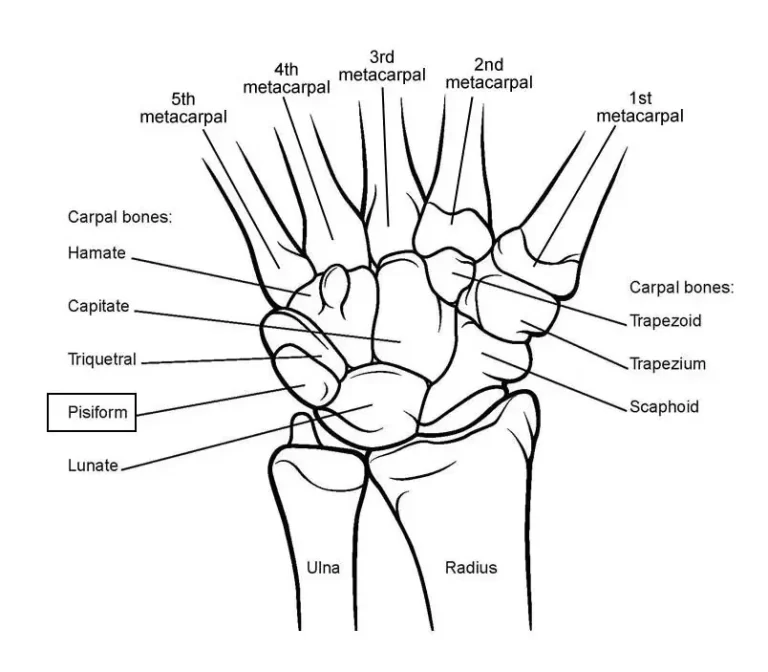
The distal end of the ulna is composed of two projections: the styloid process and the ulnar head. The ulnar notch and groove, (ulna head points downward) is the radius’s articulating surface. Supination and pronation movement of the distal forearm and wrist occur mainly due to the lateral or radial limit of the distal ulna. This serves a similar purpose as the proximal radioulnar joint, however in the opposite direction.
Embryology
The ulna bone is created by causing the lateral plate mesoderm. It then develops into the somatic mesoderm, which gives birth to all of the limbs’ bones, tendons, ligaments, connective tissue, and blood vessels. Hyaline cartilage that was previously put down can be converted into bone by endochondral ossification. Three components make up the ossified ulna. It starts at the ulnar tube’s body first. To properly calcify the bone template, the chondrocytes in the ulna’s center lay down collagen and fibronectin during week eight of pregnancy. The ends of bones are not ossified at birth; instead, they are still cartilaginous.
It starts at the ulnar tube’s body first. To properly calcify the bone template, the chondrocytes in the ulna’s center lay down collagen and fibronectin during week eight of pregnancy. The ends of bones are not ossified at birth; instead, they are still cartilaginous. An ossification center appears in the middle of the ulnar head at the age of four, and it eventually encircles the styloid process. Around age sixteen, the development of the epiphysis takes place, whereas a second center starts to emerge in the olecranon around age ten. The ossification centers surrounding the elbow grow in regular order, and recognizing traumatic injuries to the elbow requires an awareness of these developmental stages.
Blood Supply and Lymphatics
The ulnar artery provides the blood to the ulna.
The ulna’s lymphatics drain directly to the nearby cluster of axillary lymph nodes or indirectly to the supratrochlear lymph node.
Nerves
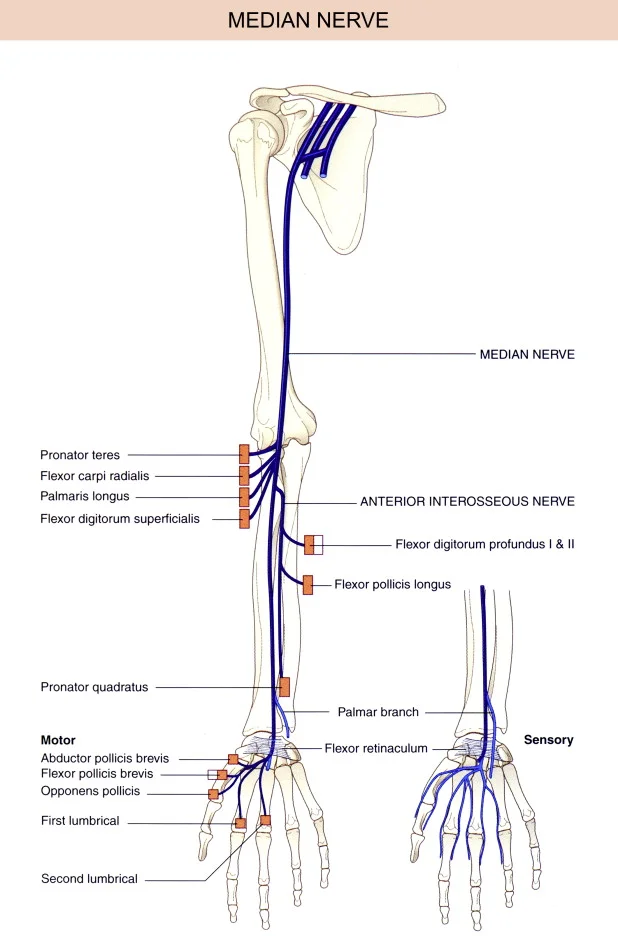
Near the ulna, the three main nerves that cross the forearm are the radial, ulnar, and median nerves. The muscles that control the flexion of the wrist and fingers (digits 1 through 3 and the radial portion of the fourth finger) are innervated by the median nerve, which runs anterolaterally. More anteromedially, between the flexor digitorum profundus and flexor digitorum superficialis, is where you’ll find the ulnar nerve. This nerve is necessary for the ulnar aspect of the fourth and entire fifth fingers, as well as for the bending of the wrist and fingers.
The anterior interosseous nerve: It is a significant branch of the median nerve. One of the prominent clinical findings associated with anterior interosseous nerve impingement or entrapment is weakness related to the “pincer” The muscles that extend the forearm, wrist, and fingers are located behind the ulna and radius and are supplied by the radial nerve.. Weakness associated with digit extension is caused by posterior interosseous nerve impingement or entrapment in the radial tunnel area.
Muscles
Many different muscles with a wide range of functions attach to the ulna.
the following muscles are inserted:
Triceps brachii: the lower portion of the olecranon’s superior surfaceOlecranon-AnconeusBrachialis: the coronoid process’ volar surface
- Extensor pollicis longus – dorsal shaft
- The coronoid process’ medial surface is known as the pronator teres.
- Olecranon process – flexor carpi ulnaris
- Coronoid process -flexor digitorum superficialis
- Anterioromedial surface of the flexor digitorum profundus
- Pronator quadratus: anterior shaft, distal
- The extensor carpi ulnaris :’ posterior border
- Supinator – proximal ulna
- Abducor pollicis longus: its posterior aspect.
- Extensor indicis – posterior distal shaft.
Physiologic Variants
An uncommon congenital fusion of the proximal radius and ulna, known as radioulnar synostosis, causes limited forearm pronation and supination. Even still, 60 to 80 percent of cases are bilateral when it does occur. Early detection of this deformity is typical; children between the ages of two and five are the most typically affected. Cleary and Ismail have devised a system of classification that describes four separate types of malformations with different forms of synostosis and osseous hypoplasia. Depending on the type of malformation and the age at which it presents, there are several treatment options, ranging from conservative to surgical.
Surgical Considerations
In people with industrial accidents, medial wrist discomfort is frequently caused by ulnar impaction syndrome (UIS). Henry Milch originally recognized UIS in 1941. Patients with overuse injuries, chronic degeneration, or acute damage to the ulnar side of the wrist are affected by it. Patients may also exhibit bone changes, such as subchondral sclerosis and bone edema, as well as changes to the wrist’s cartilage and ligaments. The need for quicker and more reliable ways to treat the symptoms is critical, as the prevalence of the condition is growing rising. Orthopedists have turned to ulnar shortening osteotomy (USO) as a surgical procedure after immobilization and nonoperative NSAIDs have failed to relieve symptoms.
The patient has comfort from this treatment because the ulna is shorter, which lessens the strain on the triangular fibrocartilage complex, which supports the carpal bones. Recent research has demonstrated that USO can both lessen pain and increase disability. However, some research has indicated that following the procedure, the joint’s range of motion was limited.
Clinical Significance
The majority of ulna-related diseases result from different fractures and fracture-dislocations. The interosseous membrane and ligaments bind the radius and ulna together to form a ring-shaped structure in the forearm. When one bone is broken or injured, there should be a greater clinical concern for the other bone or any related dislocation. A radial fracture often occurs with an ulnar fracture. First and foremost, a comprehensive history and physical examination are necessary for the diagnosis of an ulna fracture. Including the right radiographic images is also necessary to create a treatment plan that works.
Common ulna fractures include the following
- Nightstick fracture- is a break in the ulna’s central shaft, excluding further fracture sites.
- Monteggia fracture: A break in the proximal third of the ulna that is followed by a dislocation of the radial head.
- Galeazzi Fracture: The main signs are a dislocation of the distal radioulnar joint and a break in the distal radius.
- Distal ulna fracture: Most frequently connected to a dist.
FAQs
What is the ulna bone?
The two long forearm bones, the radius and ulna, make up the antebrachium. The Ulna bone situated on the medial side of the forearm reaches from the elbow to the wrist.
What is the joint of the ulna?
With the humerus in its most proximal position, the ulna’s hinge joint forms the elbow. The humerus’s trochlea inserts in the ulna’s semi-lunar notch to form this joint.
What is the ulna bone attachment?
The ulna and its attachments distinguish the anterior and posterior forearm divisions. On both ends, the antebrachial fascia is connected to the subcutaneous boundary, which is situated posteromedially.
What is the function of the ulna?
Among its numerous essential roles is assisting your wrist and forearm’s movement, flexion, and rotation, retaining the position of more than twelve muscles. support the remaining part of your hand, wrist, and arm.
Reference:
- Hullett, A. (2020, October 26). How Can You Get Rid of Back Fat? 11 Tips for the Gym and Your Plate. Greatist. https://greatist.com/health/how-to-get-rid-of-back-fat#upper-back-fat-exercises
- Shenai, A. (2023, September 6). Back Fat Exercises: Say Goodbye To Back Bulges: HealthifyMe. HealthifyMe. https://www.healthifyme.com/blog/back-fat-exercises/
- Cpt, B. R. M. M. (2023, March 3). 15 Easy Back Fat Exercises You Can Do At Home (No Equipment). Postpartum Trainer, MD. https://postpartumtrainer.com/back-fat-exercises/
- Watson, K. (2023, March 27). How to Lose Back Fat the Healthy Way. Healthline. https://www.healthline.com/health/how-to-get-rid-of-back-fat#causes-of-back-fat
- Lawton, R. (2014, June 1). The dynamic Coleman block test: a novel examination technique for cavo-varus feet. http://www.research-journal.net/en/The-dynamic-coleman-block-test-a-novel-examination-technique-for-cavo-varus-feet.html
- Coleman Block Test. (n.d.). Physiopedia. https://www.physio-pedia.com/Coleman_Block_Test
- Coleman Block Test. (2020, July 22). Wheeless’ Textbook of Orthopaedics. https://www.wheelessonline.com/bones/foot/coleman-block-test/