Supracondylar Fracture of Humerus
What is a Supracondylar Fracture of Humerus?
A supracondylar humerus fracture is an injury to the humerus, or upper arm bone, at its thinnest point, just above the elbow. Supracondylar humeral fractures are a common elbow injury in children, but they are uncommon in adults.
Most commonly incidence peaks age between 5 to 7. Dropping onto an outstretched hand when the elbow is amplified is the most frequent way to get an injury (particularly landing onto a flexed elbow has a low risk).
Compared to adult patients, children patients get elbow fractures more frequently. When they fall, children often use their outstretched arms as a safety mechanism, which raises the possibility of elbow fractures. Supracondylar humeral fractures account for up to 18% of all pediatric fractures and 60% of elbow fractures.
When treating supracondylar humerus fractures, even accomplished trauma surgeons feel nervous and uneasy, as noted by Dr. Gartland in 1959. Despite improvements in the diagnosis and management of these fractures, orthopedic doctors still confront significant challenges in their practice Guidelines for treatment for the supracondylar humerus It is common practice to portray break designs utilizing the adjusted Gartland classification. These injuries can be highly dangerous because of the possibility of brain injury, vascular injury, and compartment syndrome. Inadequate reduction and fixation may lead to malunion and deformity. Nonetheless, a malunion may eventually allow some individuals to function well.
Due to the close affection of neighboring neurovascular structures, injuries are frequent and require a thorough and thorough examination. Not every case calls for surgery. In certain situations, a firm cast could be enough to promote recovery.
Relevant anatomy:
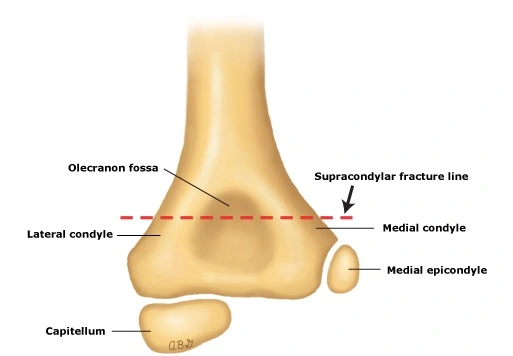
Anatomy of Supracondylar Humerus
Your forearm may rotate because the elbow joint bends like a hinge. In your elbow, there are three primary bones. Both articular and non-articular characteristics can be found on the humerus’ distal end. Your elbow’s muscles, tendons, and ligaments hold each bone in alignment.
There are various types of elbow fractures. There are some big ones. One of these situations is a humeral supracondylar break. Some are smaller than others. An epicondylar fracture, which only affects the point of the elbow, is an example of this. Any sort of break can cause extreme harm to ligaments, muscles, and nerves if cleared out untreated.
supracondylar fracture is a sort of break that most commonly happens in the humerus. The thick bone the fact that joins your elbow and shoulder is this one. The fracture occurs close to the area just above the joint.
Supracondylar breaks happen when the humerus breaks fair over the elbow joint at its distal end. The transverse portion of the humerus is fundamentally round, but it becomes flatter as it descends to meet the distal end of the humerus.
Both articular and non-articular characteristics can be seen on the humerus’ distal end. The non-articular structure comprises a front coronoid, spiral fossa, back olecranon fossa, average and sidelong epicondyles, front coronoid, and outspread fossa. On the other hand, the articular structure comprises the average trochlea that is expressed with an ulna and the horizontal capitulum that verbalizes with the spiral head.
The common root of the lower arm flexor musculature is found in a groove on the back of the average epicondyle, where the ulnar nerve travels. The common genesis of the forearm’s extensor muscles is the lateral epicondyle. Because of the association of these muscles, the distal part moves and pivots. Permit the front perspective of the distal humerus to be navigated by the brachial supply route and middle nerve.
Located very superficially to the brachialis muscle along the anteromedial portion of the distal humerus, the brachial artery is often involved in supracondylar humeral fractures. The radial nerve travels between the brachialis and brachioradialis muscles before entering the supinator muscle and traveling into the elbow.
Epidemiology:
The distal humerus’s supracondylar region is the most often fractured elbow in youngsters. Children between the ages of five and seven are typically affected. The median age is roughly six years old, and the incidence gradually declines with age. research shows that the prevalence is higher in men than in women, however, some research suggests a higher frequency in women. Nonetheless, a recent epidemiological analysis found no discernible gender disparities.
Extension-type fractures, which are significantly more prevalent than flexion-type fractures, can occur from falls on outstretched wrists.
Elbow hyperextension in children with ligamentous laxity raises the possibility of extension-type fractures. It has also been demonstrated that these fractures happen more often throughout the summer and on weekends. Children who are elderly are more prone to fractures of the flexion type. These wounds typically affect the upper extremity that is not dominant. Open supracondylar fractures take place in around 1% of cases.
Pathophysiology:
The distal humerus is approximately triangular in the coronal plane, with the medial epicondyle, trochlea, capitellum, and lateral epicondyle forming the base. The slender bone plate located at the intersection of the olecranon and coronoid fossas gives it a dumbbell-like form in the axial plane. The majority of fractures happen when a kid falls on an outstretched arm, causing the elbow to become hyperextended. The distal humerus experiences a significant load as a result of the olecranon process engaging the olecranon fossa. Under stress, the anterior humeral cortex compresses, fracturing the bone at its weakest point.
There may be intact periosteum and posterior cortex. Up to 95% of supracondylar fractures are of the extension-type fracture type, which has this mechanism of damage. Although far less often, flexion-type fractures happen when someone falls on a flexed elbow.
The etiology of the injury and the displacement of the fracture that comes from it also serve as guidelines for the reduction maneuver. The distal component’s posteromedial displacement preserves the medial periosteum. Because of this, the reduction is carried out in a pronated position, preventing varus malalignment by tensing the medial periosteum. Conversely, reduction is done in supination because posterolateral displacement often results in the rupture of the medial periosteum.
Mechanism of injury:
It is more common in children, especially in the age range when skeletal maturation has left the supracondylar bone cortex weak. Age causes the humerus’ distal end to ossify. Being reconstructed between the ages of 6 and 7, the supracondylar region often has a thinner, more slender cortex, making it more susceptible to fracture.
Because it is divided into two columns with a thin bone between them, the distal humerus structure is especially prone to injury and creates a weakness. Most often, falls on an outstretched hand (FOOSH), falls from a height, and falls while playing sports or relaxing cause supracondylar fractures.
The olecranon engages on the olecranon fossa when the hand falls onto the extended hand; if elbow extension is maintained, the olecranon eventually serves as a fulcrum on the fossa—An anterior periosteum dislocates and fractures as the consequence of anterior tensile strain from an anterior elbow joint capsule. Extension type injuries are more common (97% to 99%) than flexion type injuries (1-3%).
As a result, the fracture first occurs anteriorly but later shifts posteriorly. High energy levels disrupt the posterior cortex, which ultimately results in the distal fragment’s total posterior relocation. Fractures of the extension are operated in this manner.
The primary trigger of flexion-type fractures is elbow trauma. In the coronal plane, the distal component likewise has a tendency to translate.
Causes of Supracondylar Humerus Fracture:
- Almost any circumstance can result in a broken bone.
- One of three things can usually cause an elbow fracture: Your elbow strikes something: You could trip and land squarely on your elbow. On the other hand, you could unintentionally bang your elbow on anything solid. A direct blow could cause a fracture.
- Something strikes your elbow: Something in your surroundings could strike your elbow and cause it to break. This might have resulted from a car accident or a football helmet contact while the game was in progress.
- Striking your extended arm: When your arm is fully extended, the tendons and muscles are tense and flexed. If you land on your outstretched arm, there’s a chance the broken bones will drift apart.
Risk Factors:
Supracondylar fractures are more prevalent in younger children, though they are occasionally seen in older children. These are also the most common types of fractures in children that require surgery.
It used to be thought that boys had a higher risk of supracondylar fractures. However, according to recent research (Reliable Source), females are just as likely as boys to suffer this form of fracture. In a summer season where the injury is most prone to occur.
Symptoms of Supracondylar Humerus Fracture:
Because supracondylar fractures often present with accompanying forearm fractures, soft tissue damage, neurological injury, and a significant risk of developing compartment syndrome, a thorough evaluation of the entire upper extremity should be performed.
Among them are:
History:
In the traditional past history of an outstretched hand fall, pain and swelling on above the elbow, and loss of upper limb function, the onset of discomfort requires particular attention.
It is essential to ascertain if the pain is the result of a fracture or late-onset muscle ischemia.
Observation:
- A painful edema in the elbow and forearm that limits movement.
- It consists of bruising and skin puckering, which is caused by the proximal fragment “puckering” the deep dermis after crossing the brachialis muscle.
- A bleeding puncture wound suggests an open fracture.
- The so-called “S-deformity” is frequently observed in fractures of the misplaced extension type.
Vascular status evaluation:
As many as 10% to 20% of displaced fracture occurrences may result in vascular damage. One must palpate the wrist of the damaged extremity to feel for both radial and ulnar pulses. In cases of pulselessness, also known as pulseless hand, other markers of perfusion, such as color (the hand should be pink), temperature, capillary refill (less than 2 seconds), and It is necessary to look at the pulse oximeter’s oxygen saturation.
Neurologic status:
While neuropraxia normally takes two to three months to resolve, neuropraxia is more prevalent and usually does so when normal alignment and lengths are restored. It is crucial to know the extent of the nerve’s involvement and whether the symptoms could worsen or get better before and after treatment.
The Anterior Interosseous Nerve Branch (AIN) of the median nerve is more likely to be involved in the postero-lateral displacement of the distal fracture fragment.
Radial nerve impingement, which typically occurs when the distal fracture fragment is shifted posteromedially, can be evaluated by looking for a reduced feeling in the dorsal portion of the hand and weak wrist extensors.
Flexion-type supracondylar fractures cannot harm the ulnar nerve, yet hand intrinsic muscle weakening can cause loss of feeling in its distribution.
Vascular compromise, ecchymosis, anterior skin puckering, and severe pain are symptoms of compartment syndrome.
Classification:
- Class I: Radial, warm, crimson, and well-perfused pulse
- Class II: adequately perfused but without a radial pulse
- Class III: no radial pulse, pale or cool blue color, and inadequate perfusion
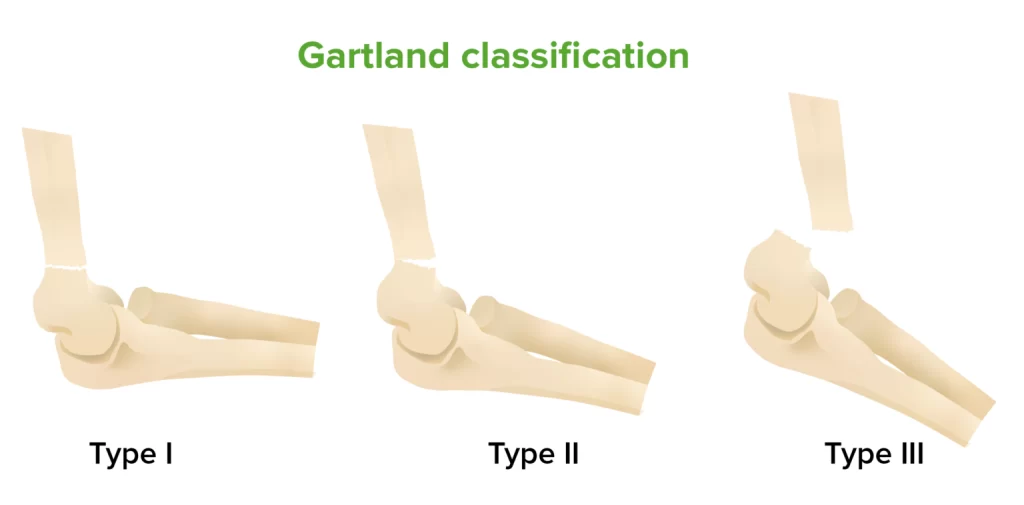
Gartland Classification of Supracondylar Fracture:
Based on Gartland’s system, supracondylar fractures in children have been classified. Fractures can be either extension- or flexion-type injuries, depending on the mode of damage and how the distal fragment is displaced. The most prevalent type of fractures are extension type fractures, whereby the distal fragment is longer than the proximal fragment. Extension injuries were originally divided into three categories: nondisplaced, moderately displaced, and severely displaced.
Wilkins added a division of type II injuries based on whether or not a rotational deformity was present to Gartland’s initial classification. In order to demonstrate multiplanar instability with a damaged periosteum, Leitch included the IV type of fracture. This subtype of fracture is detected intraoperatively when there is complete instability of the fracture.
The modified Gartland classification is as follows:
- Type I: There is very little displacement (less than 2 mm) or no fractures at all.
- Type IIA: Unbroken posterior hinge and fractures that have moved (>2 mm)
- Type IIB: A posterior hinge that remains intact in spite of displacement fracture and malrotation
- Type III: Fractures that are fully displaced and cause the posterior periosteum to be disrupted
- Type IV: Multidirectional unstable fully displaced fractures are categorized
Diagnosis:
Physical Examination:
An extension-type break may have happened sometime recently from falling on an expanded arm or flexed elbow. Even though they are uncommon, non-accidental injuries must be checked out because they account for less than half of all fractures. The kid or caregiver may provide a history of discomfort, swelling, or deformity in the affected limb. Youthful children may refuse to utilize the harmed limb. Carefully assessing the damaged limb’s distal neurovascular condition and the soft tissue envelope’s integrity is necessary. It is also necessary to thoroughly evaluate and record any assist wounds.
The arm may be bigger, deformed, and bruised. Any bleeding in the vicinity of the elbow needs to be examined since it can point to an open fracture. A typical twisting for an “off-ended” Gartland III hurt is an S-shaped distortion. A “pucker sign” in the antecubital fossa may indicate that the proximal piece penetrated the brachialis muscle, which indentations the deep dermis.
Given that it denotes a high-energy injury, the attending doctor should be alerted to the likelihood of a brachial artery or median nerve injury. These structures could become caught between the fracture fragments, so the surgeon should proceed with caution when conducting reduction. These people also have an increased chance of getting compartment syndrome.
The radial, ulnar, anterior interosseous, and median nerves’ functions need to be carefully evaluated and recorded. It is best practice to record the motor and sensory capacities of each neuron. There have been reports of brain harm in as numerous as 49% of cases. Vascular impedance has been depicted in 10–20% of uprooted supracondylar humerus fractures.
Similarly, traumatic neurapraxia has been observed in around 11% of fractures, with the most common nerve affected in flexion-type injuries being the ulnar nerve, and the most common nerve involved the anterior interosseous nerve in extension-type fractures.
Brachial course damage may happen in up to 38% of cases of uprooted Gartland III fractures. Verifying the limb’s perfusion in the region distal to the fracture is vital. It is essential to evaluate the ulna and radii beats. Note the warmth and color of the ipsilateral hand in addition to measuring the capillary refill time. It is necessary to distinguish between the “pulseless, pale, cold hand” and the “pulseless, pink, perfused hand.”
Some youngsters have a perfused hand but no pulse, which can be explained by good collateral circulation from the elbow. Both instances require emergency care, but because the latter has evidence of an ischemic limb, surgery is necessary. Vascular compromise and entrapment that involves an artery and a nerve within the fracture site are likely to occur if there is neurological impairment and a hand without a pulse.
Likewise, following every intervention, a comprehensive neurological evaluation is required and ought to be conducted again. Although doing a comprehensive nerve assessment on children can be challenging, certain games, including rock, paper, scissors, and ok, can aid in the evaluation of motor skills. To assess the motor function of the ulnar nerve, the kid is asked to abduct their fingers (scissors), the median nerve is tested by having them make a fist (rock), and the radial nerve is tested by having them stretch their fingers (paper). Lastly, they sign “ok” to indicate that the anterior interosseous nerve has been assessed.
Radiographic Evaluation:
To make the diagnosis, basic elbow radiographs are needed. Verification of the fracture type (flexion versus extension), degree of displacement, malrotation, and comminution requires anteroposterior and lateral views. The elbow is mainly cartilaginous in children. The capitellum is, to begin with, an epiphyseal center to shape at one year of age.
To appropriately interpret elbow radiographs for children, one must have a sufficient understanding of the ossified distal humerus with the age of look and fusion of all epiphyseal centers, such as the proximal radius or ulna.
Anteroposterior (AP) View:
A transverse or short oblique fracture line is sometimes visible in the distal humerus’ supracondylar region. They may even go undetected in nondisplaced fractures because they might be difficult to identify.
Baumann’s point is often referred to as the humerocapitellar point when viewing the coronal plane. It is the angle created by a line parallel to the humerus’ longitudinal axis and a tangential line that crosses the capitellar physis. A distance of 64 to 81 degrees from the longitudinal axis line is typical. An elevated Baumann’s angle indicates a cubitus varus malformation. Baumann’s angle is a precise way to measure coronal plane alignment.
Radiocapitellar Line: In each view, a line drawn along the radius’s long axis should intersect the capitellum. Unless a radial head/neck fracture is present, this is typically intact in situations of supracondylar fractures.
Lateral View:
Sign of the Posterior Fat Pad: When the elbow is bent, the posterior fat pad is located next to the olecranon fossa. Each intra-articular bone fracture in the elbow results in bleeding at the location of the fracture. The fat pad separates from the olecranon fossa as a result of the hematoma or effusion that occurs. This comes about in the generation of a positive back fat cushion sign. Numerous scholarly research efforts have highlighted the significance of recognizing the existence of a posterior fat pad sign when diagnosing nondisplaced or hidden intra-articular elbow fractures.
Anterior Humeral Line: A straight line drawn longitudinally on the lateral view along the anterior humeral cortex should divide the middle third of the capitellum. In children younger than four, the line may extend across the anterior third of the capitellum. When the line is positioned anterior to the capitellum, it indicates a fracture pattern consistent with the extension type.
Angiography:
Angiography is not recommended before a decline in the frequency of cases of vascular compromise. The Pediatric Orthopedic Society of North America (POSNA) does not recommend arteriography prior to reduction since it delays treatment.
Differential Diagnosis:
Differential diagnoses include the following:
- fractures of the radius head.
- fractures that affect the distal humerus’s medial or lateral condyles
- Transphyseal fractures of the distal humerus are another differential diagnosis to rule out in situations such as these; these injuries should not be mistaken for unintentional harm.
- The history typically points to a pulled elbow, and in these cases, radiographs are rarely obtained.
Treatment of Supracondylar Humerus Fracture:
It is necessary to assess each patient by the Advanced Trauma Life Support (ATLS) recommendations. Every injury sustained by a child needs to be considered non-accidental.
Non-Surgical Treatment:
Nonoperative therapy is appropriate for nondisplaced Gartland I fractures and slightly displaced Gartland IIA fractures. There has been discussion over how to treat Gartland II fractures. For Gartland II wounds, non-operative treatment is attainable given the break arrangement is adequate. In instances of medial column comminution, malunion, and displacement may happen.
The possibility of developing a cubitus varus deformity exists with medial column collapse. It is not suggested to treat Gartland II breaks non-operatively due to three reasons: average comminution, back uprooting, and overabundance swelling.
The non-operative treatment consists of either an above-elbow cast that maintains the elbow at 80 to 90° of flexion for three to four weeks or immobilization in the neck and grasp. Excessive edema may damage the vascularity of the forearm and cause compartment syndrome. Above-elbow casts are a more effective means to alleviate pain than a collar and cuff for Gartland I fractures. One study indicated that patients with displaced fractures of the Gartland II type had favorable outcomes with cast treatment; however, some of them experienced cubitus varus. Patients should refrain from excessive flexion when they have considerable elbow edema, which may result in compartment syndrome.
Traction was once used to treat misplaced fractures. It can be applied in settings with limited resources, such as countries with low or middle incomes and limited access to surgical equipment.
Surgical Treatment:
Orthopedic intervention is recommended for fractures classified as Displaced Gartland II and I II. Patients who have neurovascular impairment, compartment syndrome, or open fractures need to see a surgeon right away. Surgical intervention for closed injuries includes K-wire percutaneous pinning and closed reduction.
Open reduction could be required for vascular exploration, irreducible fractures, and failed closure reduction. Orthopedic surgeons should confirm their capability to address complex fracture patterns that may lead to related neurovascular injuries and that a vascular surgeon is available to aid in the treatment.
Open Reduction and Percutaneous Pinning:
Open diminishment is required when the closed approach comes up short of delivering a decrease. In particular, soft tissue/neurovascular structures that become lodged at the fracture site may hinder anatomical reduction. Open reduction might be required for open fractures.
An open approach to the brachial artery needs to be investigated if perfusion is not established after fracture reduction and repair. Whether open exploration of the brachial artery should be done when the hand is perfused following reduction and fixation but there is no radial pulse is still up for contention.
For open reduction, an anterior method is recommended. Other techniques include the posterior, lateral, and medial approaches.
Closed Reduction and Percutaneous Pinning:
This is recommended for Gartland IIB and III fractures. Furthermore, it is advised for Gartland IIA fractures when non-operative treatment (such as medial column comminution) is contraindicated and a cast is unable to produce a good reduction.
The Technique of Closed Reduction:
Closed reduction entails “milking” the soft tissues alongside in-line traction when a pucker sign is observed. While traction serves to extend the fracture to its full length, “milking” assists in freeing the soft tissues. Elbow flexion is necessary to apply traction.
The distal fragment’s medial/lateral translation and varus/valgus angulation are subsequently performed to correct the coronal plane displacement. It can be required to pronate when applying a valgus-directed force or to lie down when applying a varus force. Additionally, these motions help to correct rotational deformities.
Pronation aids in rectifying posteromedial displacement (internal rotation) while tightening the medial periosteum, while supination can assist with posterolateral (external) rotation correction. The sagittal plane distortion in extension-type fractures is addressed by hyperflexing the distal fragment. An extension may be needed in flexion-type fractures.
The Technique of Percutaneous Pinning:
It is possible to operate on bicortical structures like lateral pins and crossing pins (medial and lateral).
Iatrogenic ulnar nerve damage is less common when lateral pin designs are used often. You can utilize one, two, or three lateral pins. When inserting pins, the ideal spacing between them—whether parallel or divergent—must be maintained. The divergent pattern is thought to be more stable than the parallel configuration.
Additionally, build rigidity for lateral pins is enhanced via a capitellar starting point rather than a straight lateral entry point. A trans olecranon fossa four-cortex purchase has been described as one technique for lateral pinning to increase construct rigidity. It has been shown that fixation stability is influenced by pin size. It is found that 1.6 mm pins are not as biomechanically strong as 2 mm pins.
The construct’s rotational rigidity is enhanced when crossing pins are utilized in place of two lateral pins, however there is a higher chance of iatrogenic ulnar nerve injury. To protect the ulnar nerve, a large enough incision must be made on the medial side before the insertion of a medial pin. It is advisable to avoid percutaneous medial pin insertion because of the possibility of nerve damage.
Extending the elbow while inserting the medial pin is another technique to lower the risk of iatrogenic ulnar nerve damage This method moves the nerve even more posteriorly.
Physical Therapy of Supracondylar Fracture:
When we examine the humerus bone’s anatomy, we find that the lower end of the bone contains two condyles that contribute to the development of the elbow joint. A fracture that occurs directly above the condyles is referred to as a supracondylar fracture. To make matters more complicated, it is occasionally linked to an intercondylar fracture of the humerus.
When someone falls on an outstretched hand or receives a direct hit to the elbow, they may get a supracondylar fracture. had to defend yourself by extending your hand when you fell. In addition to causing a fracture, direct falls on the elbow also cause the broken section to shift.
Supracondylar fractures can occur as:
Fracture displacement: Surgical reduction is frequently necessary for displaced fractures.
Undisplaced fracture: Care must be taken with caution.
In both situations, a posterior mold splint immobilizes the elbow for three to four weeks at a flexion angle of 70°. There are several difficulties associated with immobilizing the elbow joint for an extended length of time, such as restricted joint movement and muscle stiffness surrounding the elbow
Following immobilization with a joint plaster cast, we recommend physiotherapy. Exercise is a good early strategy to help lower these risks. These are the workouts you should perform while your cast is still on.
Phase 1: Distal humerus reduction fracture, weeks 0 to 3:
After surgery, one should begin exercising right away to lessen problems. We must begin shoulder and wrist joint workouts while the splint is in place. Consider that six weeks following surgery, vigorous elbow extension must be avoided. So let’s start with some range-of-motion exercises for the wrist joints.
1) Active wrist flexion-extension for an elbow fracture rehabilitation:
Exercises that promote recovery without impeding the healing process are essential during this stage. Among these exercises is angling the wrist joint while maintaining a comfortable sling over the forearm. This aids in maintaining muscular tone, encouraging normal blood circulation throughout the forearm, and preventing wrist joint stiffness.
- Put your forearm on the sling and move your wrist joint up and down as demonstrated in the illustration to complete this exercise.
- Try to complete 20 repetitions or more in each session if you are comfortable.
- This is a simple exercise to fit into your daily schedule when you have a moment to spare, such as while you’re sitting and watching TV.
2) Wrist circumduction:
Wrist circumduction will be the exercise we talk about next. This is specifically made to avoid wrist tightness. This is a simple exercise that just involves rotating your wrists, as shown in the attached illustration.
- With your forearm supported inside the sling, spin your wrist in both clockwise and counterclockwise directions to complete this exercise.
- Start by softly turning your wrist in a circle. When you do this, make sure the muscles in your wrists and forearms are stretched.
- Alternatively, you can perform this exercise while sitting or standing, whatever is more comfortable for you.
- It’s important to do as many repetitions as you can, and as you get more accustomed to the workout, you can quicken the rotations.
3) Grip strength exercise:

Grip strength deficiency is not uncommon following an extended period of immobilization. This weakness can show itself in something as basic as gripping a glass of water. For this reason, it’s critical to concentrate on grip strength training as well as any other recommended workouts. The use of a gel or sponge ball is one such activity.
- Using the affected hand, forcefully squeeze the ball.
- By increasing blood circulation around the hand, this exercise can help any fractures heal more quickly.
- To strengthen your grip muscles and aid in healing, try to complete this exercise as often as you can.
4) Shoulder adduction abduction:
Shoulder joint stiffness is another typical problem that can result from prolonged immobilization. Making exercise a priority will help you improve your flexibility and supple. There’s one standing shoulder exercise that works especially well at reducing stiffness.
- Starting from a comfortable standing position, use your other hand to support the injured forearm. This will lessen discomfort and assist in stabilizing the joint.
- After you’re in position, softly shift your shoulder from right to left without exerting too much force.
- Repeat the movement 15–20 times in a session, using the given figure as a guide. This exercise can help you feel less pain and have a wider range of motion with consistent use.
5) Shoulder flexion exercise:

The first step in performing shoulder flexion extension is to use your other hand to support your forearm.
Flex your shoulder slowly and forth until it is comfortable for you to do so. The shoulder muscles are strengthened and stretched as a result.
Once your shoulder is as comfortable as possible, start slowly bringing it back.
To maximize the benefits, repeat this exercise fifteen to twenty times. This exercise can help you become more mobile and strong in your shoulders with consistent practice.
Phase-2: On Weeks 3 to 6 of reduction of distal humerus fracture:
During exercise, you can take the splint off after the third and in between the sixth week. All of the wrist and shoulder joint exercises that we covered must be repeated by you. Exercise repetitions can be increased. You should still resist moving your elbow joint, though.
- Carry out these exercises again:
- Wrist circumduction,
- wrist flexion-extension in action,
- Exercises for grip strength,
- shoulder flexion exercise,
- shoulder adduction and abduction
Phase-3: Week 6 to 10:
The posterior elbow brace will be taken off by the sixth week, at which point we should concentrate on elbow range of motion and strengthening activities. Elbow flexion, extension, forearm pronation, and supination are things we need to pay attention to.
6) Active wrist flexion-extension:
Certain exercises need to be done to restore elbow flexion and extension motion.
- Let’s begin by positioning the afflicted arm on a table and taking a comfortable seat in front of it. Elbow exercises can be performed with an adequate basis of support when the arms are kept flat on the table.
- First, straighten the elbow to the maximum extent achievable.
- After a few seconds of holding the position, gradually bend the elbow to its maximum flexion.
- At least 15 to 20 repetitions of this alternate flexion-extension exercise should be performed in a single session.
- It is important to consistently carry out this exercise to help the elbow return to its typical range of motion.
7) Stretching of wrist flexor and extensor:

This particular stretching practice is intended to assist reduce stress and improve wrist flexibility.
- Assume your initial posture and extend your arm in front of you to get started.
- Gently push the wrist to its maximum flexion and extension with the opposite hand.
- Start by slightly extending your wrist, then apply pressure on your palm with your other hand to stretch the flexor muscles.
- Maintain this position for a minimum of thirty seconds to give the muscles time to unwind and expand completely. It should not hurt to feel a slight pressing feeling in your wrist.
- Then, to stretch the muscles that make up the extensor group, perform the same motion by extending the wrist.
- Apply pressure to the posterior aspect of your hand with your opposite hand once more, and hold the position for at least thirty seconds.
8) Forearm supination, pronation exercise:
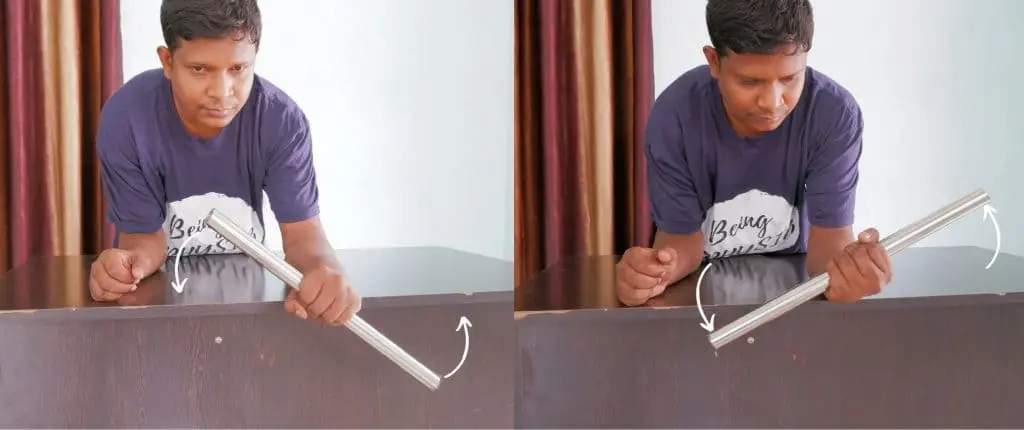
Exercises that promote forearm pronation and supination are essential for preserving elbow joint mobility during the healing process following a fracture to the shaft of the humerus. Rotating your forearm clockwise and counterclockwise while supporting it on a flat surface, such as a table, is one of the best exercises for this purpose sure your forearm is safe and solid by placing it flat on the table first.
Next, perform supination, or slowly rotating your forearm in a clockwise manner.
After a few repetitions, go on to forearm pronation, which is the rotation of your forearm in an anticlockwise manner.
You can attempt this exercise on your own after you feel more at ease with it.
On the other hand, you can rotate your forearm while holding a cane or light rod to increase the exercise’s effectiveness. This will make the activity more difficult and advantageous for your rehabilitation by adding additional resistance and velocity.
9) Shoulder forward elevation exercise for elbow fractured:
In some circumstances, it’s normal to ignore shoulder joint soreness. If, however, this issue is not resolved, it may soon become problematic. It is essential to include shoulder workouts in your regular routine because of this. The straightforward yet powerful shoulder elevation exercise is one of these.
- To begin with this exercise, take hold of your hand and slowly raise it as high as you feel comfortable going.
- After holding it there for a short while, carefully bring it back down.
- In a single session, repeat this technique fifteen to twenty times.
- Try to perform this exercise twice a day for the best results.
- Shoulder range of motion (ROM) exercises are beneficial for both preventing and treating shoulder stiffness.
10) Stretching of elbow flexor muscle:

The flexors and extensors of the elbow, two muscle bunches fundamental to elbow development, are the center of this workout. The flexor muscles, which are found on the outside of the elbow, are in charge of allowing the elbow joint to flex. The extensor muscle, on the other hand, is found on the back of the elbow and is in charge of the elbow joint’s extension or straightening.
- To start the elbow flexor stretching exercise, extend your elbow to its maximum and place your other hand on the front of your elbow.
- Till the front of the elbow stretches comfortably, slightly overpress the area.
- To help the muscles relax and release tension, hold this stretched position for at least 30 seconds.
- It’s also time to extend your elbow extensors. You must do this by twisting your elbow and resting your other hand on the back of your elbow.
- After you feel a comfortable stretch on the back of the elbow, slightly overpress the area and hold it there for at least thirty seconds.
- It is advised to perform this procedure three to five times in a single session to avoid overdoing it and causing additional harm.
Phase-4: Weeks 10-12+ of supracondylar elbow fracture:
Return to light activities and exercise gradually. After 12 weeks, there are no further restrictions on activity.
Progressive strengthening exercises:

It’s important to gradually return to modest activity and exercise as part of your recovery. There are no further activity limitations after the first twelve weeks.
To perform this exercise, you will need a set of 1.5–2 kg dumbbells. It’s necessary to remember that this exercise should only be done if you have developed the grip strength to grasp the dumbbell firmly.
- Start by standing erect posture and using the hand on the affected side to hold the dumbbell. Hold it firmly enough that your elbow joint feels a mild stretch from the dumbbell’s weight.
- As long as it suits you, maintain this posture for one to five minutes.
- The weight of the dumbbells can be gradually increased to 5 kg as you get more used to this exercise
Home care advice:
To lessen edema during the initial two days:
- When your child is seated or sleeping, use pillows to lift their arm above their heart.
- For a few days, apply cold packs covered in a towel to the cast for 20 to 30 minutes every 3.4 hours.
- To keep the cast or splint dry, avoid placing ice directly on it.
- If your child’s physician recommends giving them pain medication, you can give them either Ibuprofen (any brand) or Paracetamol (any brand).
- To determine your child’s appropriate dosage, refer to the instructions on the medication container.
- Giving your child aspirin can result in serious consequences, so avoid doing so..
- As advised, make sure your youngster shows up for the follow-up visit.
- Make sure your youngster stays away from playground equipment, sports, gym classes, and other activities until you give the all-clear.
Daily cast or splint care:
- Remind the child to wriggle their fingers to maintain regular blood flow.
- Examine the splint’s or cast’s margins.
- Make sure the edge padding isn’t being removed or picked at by your child.
- Ensure that the child doesn’t fill it with food, toys, or other items.
- Keep powder, lotion, sand, and contaminants away from the splint or cast.
- When your child is up and moving around, make sure they are wearing the sling. The child should not sleep with the sling on.
Keep the cast dry:
- Avoid swimming.
- Give your kids sponge showers.
- Older children should bath rather than shower.
- When the child bathes, cover their arm with a plastic shield. To keep the cast or splint entirely out of the water, raise the arm up on anything.
- Use a hair dryer preset to cool and gently blow air into the cast or splint if it has accidentally spilt.
Complication:
Immediate effects associated with neurovascular involvement include the following:
Vascular insufficiency is most frequently associated with Type II and III supracondylar fractures, which are frequently observed in fractures that are displaced postero-laterally, and pink pulseless hand involvement of the brachial artery.
0.1% to 0.3% of cases may have compartment disorder. Compartment weights are expanded by elbow flexion past ninety degrees and related lower arm fractures To lower the risk of compartment syndrome, the elbow should be immobilized at a flexion of around 30° in the emergency department and 60° to 70° following surgery.
The neurologic deficit ranges from 10% to 20% of humeral supracondylar fractures and is primarily linked to Type III fractures.
Pediatric patients often have long-term difficulties due to their exceptional ability for bone growth and remodeling. As a result, the immediate post-management condition and the long-term functional outcome of a fracture may be very different.
The cubitus varus deformity, occasionally referred to as a “gunstock” deformity, is brought on by a malunion. The displacement of the medial head of the triceps, delayed postero-lateral rotatory instability (PLRI), and secondary distal humeral fractures are important problems associated with posttraumatic cubitus varus deformity.
Modern surgical methods, such as closed decrease with percutaneous sticking, have diminished the predominance of this method in children treated for supracondylar breaks from 58% to generally 3%. The disease is treated with a humeral osteotomy, which also prevents future difficulties of the same kind.
If associated ischemia is not treated right away, compartment syndrome may lead to Volkmann’s ischemic contracture. Fixed elbow flexion, forearm pronation, wrist flexion, and metacarpal-phalangeal joint extension are the characteristics of this syndrome. Infarction could also result from it.
Prognosis:
The prognosis is influenced by the patient’s remodeling potential, injury-specific factors, and bone quality.
Remodeling Factors:
Remodeled areas are subject to the following requirements:
- The age of the patient and their potential for further growth
- The distinction between a real break and a genuine
- The displacement level of the deformity plane
The humerus’s physis is accountable for 20% of the distal humerus’s longitudinal expansion. Compared to the coronal plane, the elbow’s sagittal plane distortion offers more remodeling potential. Consequently, the supracondylar area of the distal humerus has limited potential to heal after injury in situations of malunion deformity.
Younger patients have more possibility for remodeling because they still have more growth in them, but only for sagittal plane deformity. Coronal plane deformity does not remodel.
Injury-Specific Factors:
- Damage level
- Enough reduction and fixation
- The neurovascular state of the leg
Taking a proper treatment at the right time improves the long-term prognosis for many injuries. However, comes about can be made strides with anatomical lessening, steady obsession, and suitable care of the delicate tissues, counting neurovascular wounds and compartment disorders, higher-grade wounds may have a more awful prognosis.
Non-displaced Gartland I breaks more often than not mend well without any problems. Cubitus varus needs to be recognized, minimized, and stabilized if it appears in Gartland II fractures with medial comminution. Even in spite of the fact that Gartland III and IV wounds have a higher chance of neurovascular harm, opportune and fitting treatment can lead to effective comes about.
Summary:
In the time frame of the ages of five and eight, the most frequent type of fracture in children is a supracondylar fracture of the humerus. The most visited mode of harm for a humeral supracondylar break is FOOSH.
Preoperative and postoperative neurovascular evaluations are crucial. For displaced fractures without neurovascular involvement, closed reduction with percutaneous pinning is the advised medical procedure. It is recommended that children with elbow fractures engage in physical activity as opposed to passive care.
FAQs
What nerve damage is typical in fractures of the supracondylar humerus?
While ulnar nerve palsy is the most frequent postoperative consequence, anterior interosseous nerve injury is the most frequent starting injury.
What is the name for a supracondylar fracture?
Your child’s humerus fractured near the elbow, just above the joint. The term supracondylar (pronounced soo-pruh-kaan-duh-lr) refers to this kind of humeral fracture. The most prevalent kind of elbow fracture, affecting kids less than eight, is this one.
What surgical procedure is used to treat supracondylar fractures?
Treatment for supracondylar humerus fractures in children (SHFC) can result in iatrogenic brain injury, functional deficiency, and residual deformity. The conventional treatments include closed reduction and various configurations of percutaneous Kirschner wire fixation.
What symptoms indicate a supracondylar fracture?
severe arches in both forearms and elbows. Swelling in your elbow. You can’t extend your arm because of tingling in your hands and a loss of elbow function.
How is a pediatric supracondylar humerus fracture treated?
The recommended courses of therapy for the majority of displaced supracondylar fractures include closed reduction and percutaneous pinning (with two or three lateral pins). Medial pin implantation is necessary in some fracture patterns, and surgical procedures are described to minimize damage to the nerves.
What is the healing period for a supracondylar humerus fracture?
Supracondylar humerus fractures often heal in 4 weeks after therapy (casting or surgery). It can take your child four weeks to be able to move their elbow normally when their cast is taken off. Your youngster will receive a sling or a removable long-arm splint if they have pins in their arm.
Is surgery required for all supracondylar fractures?
Patients with non-displaced type 1 traumas (bones that shattered but did not move) are placed in a long arm cast for protection while the arm recovers. In type 2 and 3 injuries, the bone shifts or displaces, therefore surgery is usually necessary to realign the bones.
How should someone with a supracondylar fracture sleep?
When your child is seated or sleeping, use pillows to lift their arm above their heart. For a few days, apply cold packs covered in a towel to the cast for 20 to 30 minutes every 3.4 hours. Ice should not be applied directly to a cast or splint because they need to be dry.
How is a supracondylar fracture detected?
Anteroposterior (AP) and lateral x-rays of the distal portion of the humerus (not the elbow) should be obtained if a supracondylar fracture of the humerus is suspected. ADVICE: Refrain from wearing a short, fragile backslab.
What deformity follows a supracondylar fracture most frequently?
The elbow deformity known as cubitus varus (red arrow) may be caused by a supracondylar humeral fracture that is not healing properly. The forearm deviates towards the midline and the arm’s typical carrying angle is reversible when the elbow is stretched.
In what way does a supracondylar fracture harm?
The symptoms of a supracondylar fracture include severe, excruciating elbow and forearm pain. a pop or snap at the moment of harm. swelling in the elbow’s surrounding area.
What is the name of a supracondylar fracture?
Supracondylar fractures occur into two categories: flexion (<5%) and extension (95–98%). Supracondylar fractures of the extension type usually originate from falls onto an overextended elbow.
What does a supracondylar fracture angle mean?
if evaluating supracondylar fractures, or distal humeral fractures, Baumann’s angle is utilized. By drawing a line across the center of the humeral shaft, the trochlea, and finally a line perpendicular to the humeral shaft line, one can determine the angle.
Where is the supracondylar region?
The upper arm’s long bone is called the humerus. A fracture of this bone’s lower portion, at the elbow, is called a supracondylar fracture. Especially in younger children, it is one of the most frequent fractures we find.
Reference:
Solanki, G. (2024d, January 27). Supracondylar Humerus Fracture – What You Need to Know. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/supracondylar-humerus-fracture/
Hope, N., & Varacallo, M. (2023b, August 4). Supracondylar Humerus Fractures. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560933
Ekka, S. S. (2024, March 4). 9 Easy Supracondylar Fracture Humerus Physiotherapy Exercises| Elbow Fracture. Physiosunit. https://physiosunit.com/supracondylar-humerus-fracture-treatment-physiotherapy/
Sidra Medicine. (n.d.). https://www.sidra.org/patients-visitors/patient-family-education/education-resources/emergency-department-education-material/how-care-your-child-supracondylar-fracture-type-1







One Comment