Superior Gluteal Nerve
Introduction
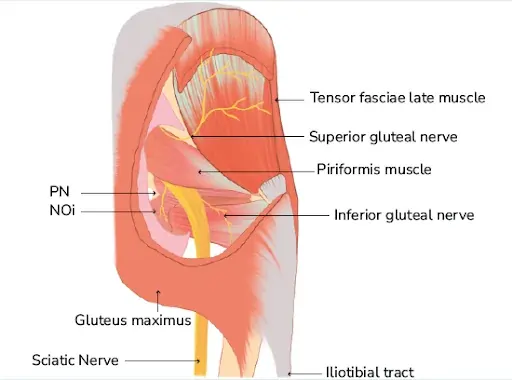
The superior gluteal nerve, a motor branch of the sacral plexus, originates from the posterior divisions of the L4, L5, and S1 anterior roots. The superior gluteal nerve and vessels travel through the greater sciatic foramen before passing superiorly to the piriformis muscle.
From there, the nerve splits into its superior and inferior branches, the former of which innervates the gluteus medius muscle and the latter of which innervates the gluteus minimus and the tensor fasciae latae muscle.
Structure
The superior gluteal nerve innervates the muscles of the gluteus medius, gluteus minimus, and tensor fasciae latae. With the gluteus minimus and tensor fasciae latae, the gluteus medius is in charge of hip joint abduction.
Because of its anterior component, the gluteus minimus is essential for the medial rotation of the thigh in addition to facilitating hip abduction. In contrast, the tensor fasciae latae helps in hip extension by providing traction on the iliotibial tract through the gluteus maximus muscle. The abductor mechanism, which enables foot clearance during the swing phase of gait and stabilizes the pelvis during the single leg phase, is made up of these three parts.
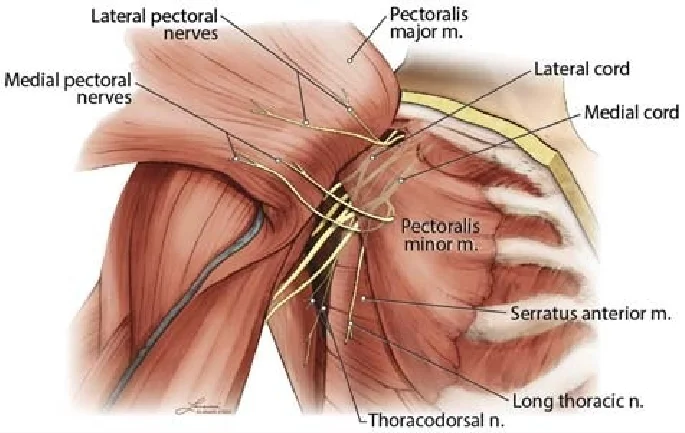
Alongside the inferior gluteal nerve, sciatic nerve, and coccygeal plexus, the superior gluteal nerve emerges from the posterior divisions of the L4, L5, and S1 nerve roots of the sacral plexus. After that, the nerve moves posterolaterally before exiting the pelvis through the superior gluteal vessels and the larger sciatic foramen.
Being the sole nerve to leave via the larger sciatic foramen above the piriformis muscle, the superior gluteal nerve is special. The pudendal nerve, inferior gluteal nerve, sciatic nerve, and all other nerves that leave through the larger sciatic foramen are inferior to the piriformis. The tensor fasciae latae muscle is where its branches end. It then enters the gluteal area, passes across the inferior aspect of the gluteus minimus, and then moves anteriorly and laterally inside the plane between the gluteus medius and gluteus minimus muscles.
Function
The superior gluteal nerve splits into superior and inferior branches above the piriformis muscle. The superior division innervates the gluteus medius and, on occasion, the gluteus minimus. It follows the top segment of the deep division of the superior gluteal artery. An estimated 5 cm above the tip of the greater trochanter, the superior gluteal nerve runs over the deep aspect of the gluteus medius.
In contrast, the inferior branch of the superior gluteal nerve crosses the gluteus minimus and innervates both the gluteus medius and the lower part of the deep division of the superior gluteal artery. The inferior branch finally culminates in and innervates the tensor fasciae latae muscle.
Course
Through the larger sciatic foramen, which is located above the piriformis muscle, it leaves the pelvis. Additionally, the superior gluteal vein and artery accompany it.
Alongside the deep branch of the superior gluteal artery, it travels laterally between the gluteus medius and gluteus minimus muscles. It splits into two branches: superior and inferior.
The tensor fasciae latae muscle is where the inferior branch ends after continuing to travel between the two muscles.
Muscle Supply
The superior gluteal nerve innervates the gluteus minimus, gluteus medius, and tensor fasciae latae muscles. Since they offer a substantial stabilizing force during the terminal swing phase, the gluteus medius and gluteus minimus muscles are both functionally essential to the gait cycle.
The Trendelenburg or gluteal gait is a distinctive loss of motor function caused by damage to this nerve that manifests as a crippling gluteus medius limp. In this condition, the center of gravity shifts to the unaffected leg due to the weakening of the gluteus medius muscle. A waddling gait is frequently the outcome of bilateral superior gluteal nerve injuries.
The thick, fan-shaped gluteus medius muscle originates from the middle gluteal nerve inferiorly, the gluteal line posteriorly, and the outside portion of the ilium superiorly from the iliac crest. After that, the muscle moves inferolaterally in the direction of the greater trochanter’s lateral surface. To enable powerful hip abduction, the gluteus medius collaborates with the gluteus minimus and tensor fasciae latae.
The anterior fibers of the gluteus medius facilitate medial rotation of the thigh as well. Walking and running are made possible by the functional cooperation of the gluteus medius muscle, gluteus minimus, and tensor fasciae latae. The contraction of the contralateral gluteus medius, gluteus minimus, and tensor fasciae latae prevents the lower extremity limb that is not in contact with the ground from tilting downward when walking or running.
The gluteus minimus, which originates from the lateral portion of the ilium between the inferior and intermediate gluteal lines, is also a fan-shaped muscle situated deep in the gluteus medius. Inferolaterally, the muscle fibers move in the direction of the greater trochanter’s anterior surface. Similar to the gluteus medius, the gluteus minimus is in charge of hip abduction and the thigh’s medial rotation.
The tensor fasciae latae is a little muscle that originates from the outside portion of the iliac crest and is located between the iliac tubercle and the anterior superior iliac spine. Encased in a sheath made of the iliotibial tract of the fascia lata on the lateral thigh, the muscle moves inferiorly and posteriorly. To help the gluteus maximus with hip and knee extension, the tensor fasciae latae provides traction on the iliotibial tract. To keep the knee in a fully extended posture, this motion is essential.
Anatomical Variation
However, a more frequent variation was the distribution of the nerve around the greater trochanter. Additionally, cadaveric dissections have shown that the superior gluteal nerve divides into the typical two branches in 86.20% of cases, while it further subdivides into three branches in 13.8% of cadavers.
Variations have been documented in the course of the superior branch of the superior gluteal nerve, specifically that of the superior branch traversing below the inferior branch of the superior gluteal nerve, that descended inferolateral and entered the tensor fasciae latae.
It has been noted that the piriformis muscle has an abnormal double belly composition, with the superior gluteal nerve stuck between the two muscular bellies. This finding points to a distinct anatomical variation that might be the uncommon source of unidentified persistent gluteal discomfort and piriformis syndrome.
Clinical Importance
The standing leg’s little gluteal muscles aid in maintaining the pelvis’ coronal plane stability during normal walking. A weak abduction of the affected hip joint may arise from muscular paralysis or weakness caused by damage to the superior gluteal nerve. The Trendelenburg gait is the name given to this kind of gait impairment.
Abduction of the ipsilateral hip joint should raise the opposing pelvis higher while the patient is standing on one leg. The positive Trendelenburg sign is caused by the pelvis sagging when the abductors are weak because of superior gluteal nerve paresis. The pelvis sags towards the swing leg, which is the typical unsupported side, in a patient with a positive Trendelenburg sign. The Duchenne limp is a deficiency that arises when the reverse happens, causing the pelvis to rise on the swing side.
Bilateral injury to the superior gluteal nerve causes a gluteal gait, or “waddling.” Additionally, as the leg swings forward during ambulation, the patient may elevate the foot of the unsupported side, resulting in a steppage gait. When the foot on the unsupported side swings out laterally, this is known as a swing-out gait.
Surgical Importance
Hip dislocation, hip fractures, hip arthroplasty, and intramuscular injections into the buttocks can all cause damage to the superior gluteal nerve. Hip discomfort can have several causes, including fractures, tendinitis, bursitis, and arthritis. Over the past few years, surgical treatment for hip osteoarthritis has changed.
The anterior side of the gluteus medius and vastus lateralis are separated and reflected forward as a single sheet using innovative surgical reconstructive procedures, and this sheet is then reattached to the greater trochanter. Nevertheless, there are risks associated with these treatments, including infections and harm to neurovascular structures. Crucially, there is a higher chance of harm to the superior gluteal nerve and superior gluteal vasculature if the gluteus medius muscle splits more than a few centimeters (usually 5 cm) above the greater trochanter’s apex.
The route and branching pattern of the superior gluteal nerve mostly determines the likelihood of damage. Determining the superior gluteal nerve’s safe zone and the distance between it and the greater trochanter are crucial when making approaches to the hip joint. For the anterior third of the gluteus medius, the safe distance for the superior gluteal nerve after hip surgery is 4 cm from the tip of the greater trochanter, and for the posterior and middle third, it is 5 cm. Furthermore, it was shown that the greater trochanter’s average distance from the gluteus medius innervation site varies with body height.
Therefore, a straight lateral approach, sometimes referred to as the Hardinge approach to the hip, increases the risk of neurological damage during hip surgeries.
Additionally, abduction weakness and limping are frequent side effects of closed antegrade femoral nail insertion, and they are most likely caused by iatrogenic damage to the gluteus medius and the superior gluteal nerve. However, the risk of damage to the gluteus medius and the superior gluteal nerve is reduced by increasing the degree of hip flexion and adduction during femoral nail insertion.
Higher degrees of hip flexion and adduction can be achieved using either the lateral position on a fracture table or the “sloppy” lateral position on a regular table, depending on how the hip is positioned.
Drugs are also frequently administered in the gluteal area, especially when quick action is needed if the medicine is not viable when taken through the intestines. To avoid the branches of the sciatic nerve and superior gluteal nerve, which are normally found in the lower quadrants of the buttock, the injection should be given in the superolateral quadrant.
FAQs
What are gluteal nerves?
The superior gluteal nerve innervates the muscles of the gluteus medius, gluteus minimus, and tensor fasciae latae. Alongside the superior gluteal artery and vein, the nerve leaves the pelvis through the larger sciatic foramen, which is located above the piriformis muscle.
Is walking good for buttock pain?
Lower back disc degeneration may cause discomfort in the thighs and buttocks. This discomfort can worsen when you sit, bend, or lift anything. Walking is one form of movement that helps alleviate it.
How long can gluteal pain last?
Minor strains often heal in a few days to a week. Mild strains may recover completely in two to three weeks, but severe strains may take four to six weeks or longer.
What is the best exercise for buttock pain?
Hip and buttock pain physiotherapy
This information is to help you learn more about hip and buttock problems and some basic exercises that can help. …
Hip abduction and clam. …
Hip flexor stretch. …
Hip flexion, external rotation, and bridging. …
Piriformis stretch. …
Split squat lunge. …
Chair squats/squats. …
Quads and hamstring stretch.
Is buttock pain serious?
If the buttock pain is severe, persistent, or accompanied by other symptoms such as numbness, tingling, difficulty walking, or bladder or bowel dysfunction, it is advisable to seek medical attention promptly. These might point to a more serious underlying condition that needs to be evaluated and treated by a specialist.
References
- Gluteal nerves. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/gluteal-nerves
- Gluteal nerves. (2023, August 14).StatPearlshttps://www.ncbi.nlm.nih.gov/books/NBK535408/
- Wikipedia contributors. (2024a, February 11). Superior gluteal nerve. Wikipedia. https://en.wikipedia.org/wiki/Superior_gluteal_nerve