Smith Fracture
What is Smith Fracture?
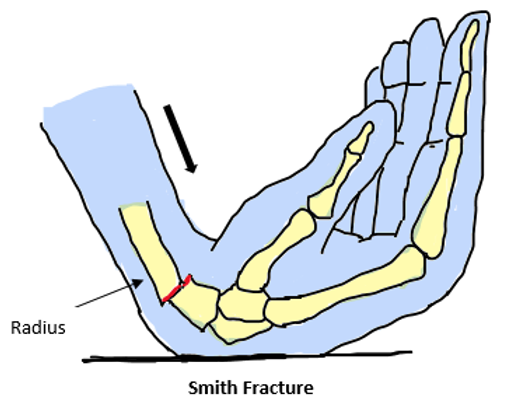
A fracture that involves volar displacement or distal radius angulation is referred to as a Smith fracture. It usually occurs from a fall onto the dorsum of the hand with the wrist flexed.
A Smith’s fracture, often referred to as a reverse Colles’ fracture, is the volar, or forward, displacement fracture of the distal (i.e., away from the body, towards the fingers) end of the radius, or one of the two forearm bones on the lateral, or thumb side of the forearm.
The distal radius is the most common fracture location in the upper extremities, capturing around 5% of all radial and ulnar fractures. Smith’s fractures are the name given to these fractures. Smith’s fractures are referred to as Goyrand fractures in French literature, after the French surgeon Jean-Gaspard Blaise Goyrand.
Bone fractures come in a variety of forms, and the terminology used to describe them can be confusing. As an example, Smith fractures are occasionally classified as a specific type of distal radius fracture. The radius, one of the bones in your forearm, points away from your wrist.
Epidemiology:
The upper extremity fracture that occurs the most frequently is the Smith fracture. Distal radial fractures account for more than 16% of adult fractures and 75% of forearm fractures, with over 600,000 cases happening annually in the United States alone. Smith fractures are the second most common fracture among older persons. Conversely, around 5% of all ulnar and radial fractures are Smith fractures.
The age group with the highest frequency of Smith fractures is that of young boys and elderly females. Children who fall with great energy and elderly persons with osteoporosis who fall with little energy account for nearly all cases of Smith fractures.
After hip fractures, Smith fractures are the second most common kind of fracture in the elderly population. Between the ages of 64 and 94, women are six times more likely than men to suffer this type of fracture. There appears to be a clear correlation between decreased bone mineral density and low-energy trauma-induced Smith fractures.
Causes of Smith Fracture:
The most prevalent cause of this type of fracture is a history of falls on an outstretched hand from a standing height, however, high-energy injuries account for a small percentage of fractures. When compared to people who have a history of elbow or humerus fractures, individuals who have fallen on their outstretched hand in the past are typically fitter and have better reflexes.
The strength integrity of the bone, the variety of surfaces, the impact velocity, and the hand position at the time of impact all affect the characteristics. When a distal radius fracture occurs, the wrist is often bent posteriorly between sixty and ninety degrees.
If the wrist has twisted to the ulna side, or the other way around, the radial styloid fracture will occur. A proximal forearm fracture would occur if the wrist deviated posteriorly less a carpal bone fracture would occur if the wrist deviated posteriorly more. A fracture requires greater power when bending backward. Men require greater force to fracture than women do. Increased risk of harm in individuals with osteoporosis.
Interosseous intercarpal ligament injuries, including scapholunate (4.7 percent to 46 percent of cases) and lunotriquetral (12 percent to 34 percent of patients) ligament damages, are common injuries associated with distal radius fractures. If there is a wrist joint fracture and there is an ulnar variance (difference in length between the distal end of the ulna and the distal end of the radius) of greater than 2 mm, there is an elevated risk of interosseous intercarpal injury.
Damage to the triangular fibrocartilage complex (TFCC) occurs in between 39 and 82 percent of patients. By a ratio of five, ulnar styloid process fracture increased the likelihood of TFCC injury. However, it remains unclear if triangular fibrocartilage injuries and intercarpal ligaments are associated with chronic pain and disability in persons who are involved.
Risk Factors of Smith Fracture:
Smith fractures can happen to anyone because they are typically the result of trauma or an accident.
One significant risk factor is osteoporosis. If you have osteoporosis, your bones are more likely to break. Anyone can get HIV, but women are four times more likely than men to do so. In addition, people over 50 have an increased risk of developing osteoporosis.
Symptoms of the Smith Fracture:
Pain, edema, reduced range of motion, and a distal forearm deformity may be observed during the physical examination; however, it is difficult to determine the direction of volar angulation visually. The diagnostic criteria for Smith’s fracture include a deformed wrist with obvious swelling on the volar side and the prominence of the ulna along the wrist’s dorsum.
Apart from the volar displacement of the distal fragment, there is often a disruption of the triangular fibrocartilage complex and the distal radioulnar joint. Fractures of the ulnar styloid base may also be related.
Evaluating the affected extremity’s neuro-vascular status is essential. Up to 15% of Smith’s fractures may exhibit signs of acute carpal tunnel syndrome due to compression of the median nerve, according to a study. Compression of the ulnar and radial nerves occurs less frequently. Acute forearm compartment syndrome is another symptom of Smith’s fracture.
Signs of the Smith Fracture:
A distal forearm deformity is a common manifestation of Smith’s fractures, albeit it can be difficult to detect the direction of displacement without radiography. Edema, reduced range of motion, and wrist pain are common side effects of Smith’s fractures.
Less frequently, the neurovascular system in the wrist and hand is compromised due to the compression of one or more nerves from the broken bone. The person may experience tingling, numbness, or weakness in the hand or wrist areas that are innervated by the damaged nerve if the neurovascular system is impaired.
A pinched median nerve can result in symptoms of acute carpal tunnel syndrome in the thumb, index, middle, and ring fingers. Radial nerve compression is an uncommon condition that can affect the thumb and index finger on the radial side of the hand. In a rare instance, ulnar nerve compression may also impact ulnar side fingers, including the ring and pinky fingers.
It is also possible to experience acute compartment syndrome of the forearm, which manifests as paresthesia, or “pins and needles,”
- severe pain.
- Wrist pain increasing sensitivity
- Not being able to move your wrist without pain
- Discolorations or injuries in the wrist area
- A bump or other irregularity that isn’t ordinarily there on your wrist.
Staging of Smith Fracture:
Three forms of Smith fractures are distinguished according to the extent of articular involvement:
- Type I: Distal radius is the only bone affected by an extra-articular distal radial fracture. Approximately 85% of instances are related to this disease.
- Type II: Intra-articular oblique fracture: This type of fracture, which affects the dorsal radial articular surface, is sometimes referred to as the reverse Barton fracture. Approximately 13% of instances involve this type of injury.
- Type III: An oblique fracture extending into the radiocarpal (wrist) joint, known as a Juxta-articular fracture. Less than 2% of cases are of this most severe but least common variation.
The complexity of Smith fractures often affects therapy and patient outcomes.
Diagnosis:
The first step in diagnosing a Smith’s fracture is typically a thorough medical examination of the patient, which includes a history of any present illnesses, a review of past medical records, and an evaluation of signs and symptoms. Next, a physical examination is conducted. After examination, AP and lateral X-rays are often obtained to help distinguish between Colle’s and Smith’s fractures.
Additional radiographs or more complex imaging methods, such as a CT scan, an X-ray with an oblique view, or traction, may be used to look for soft tissue damage. A CT scan may also be used to diagnose severe comminuted fractures, fractures consisting of three or more sections, or intra-articular fracture patterns.
History and Physical Examination:
Trauma is a common cause of Smith fractures. Before starting a thorough workup, emergency conditions need to be promptly ruled out, just like in any other trauma case. For emergency surgery, open fractures, and compartment syndrome, for instance, call for an orthopedic specialist’s prompt referral. After ruling out emergencies, the clinician may move forward with a focused evaluation.
The patient’s history will show that they fell on their flexed hand. Soon after the injury, symptoms such as pain, edema, deformity, and restricted joint movement appear. Hand weakness or numbness that goes along with it indicates nerve involvement.
Physical examination can identify a distal forearm deformity, but it may be difficult to see whether the angulation is dorsal (Colles) or volar (Smith). Exam results also show a limited range of motion, pain, and swelling. Two of Smith’s early diagnostic criteria were the prominence of the ulna along the wrist’s dorsum and a deformed wrist with obvious swelling on the volar side.
Along with the volar displacement of the distal fragment, dislocation of the distal radioulnar joint (DRUJ) and the triangular fibrocartilage complex (TFCC) are frequent occurrences. Fractures of the ulnar styloid base may also be related Evaluating the affected extremity’s neurovascular condition is crucial.
To reach a compromise, immediate closed-reduction measures would need to be taken. Up to 15% of these fractures may result in symptoms of acute carpal tunnel syndrome (ACTS) due to compression of the median nerve. Compression of the radial and ulnar nerves is less common yet nonetheless presents neurological complications. Another cause of neurovascular dysfunction seen in Smith fractures and other distal radius fractures is acute compartment syndrome of the forearm..
Investigation:
X-ray:
Both AP and the lateral radiograph of the wrist can be used to diagnose the fracture. It can display a distal radial fracture with volar angulation’s location (extra-, juxta-, or intra-articular), as well as its degree of angulation, displacement, and existence.
Additionally, it can offer an understanding of carpal misalignment, carpal fractures, and the articulation of the radio-lunate and radio-scaphoid joints. Additional wrist radiographs, such as fossa lateral, traction, and oblique views, may provide essential details about the associated soft tissue injuries.
Ct-scan:
In cases of comminuted or intra-articular fractures, a CT scan not only helps determine the pattern of injury but also assists the surgeon in developing an operative reduction strategy. A CT scan can help define and evaluate the pattern of damage in these cases.
Enhancing Healthcare Team Outcomes:
For the best results, a multidisciplinary team is the best resource for managing Smith fractures. This team’s members consist of the following individuals:
- The majority of patients with Smith fractures initially visit the emergency room, according to emergency medicine physicians. The first medical professional these patients see is the emergency medicine doctor. The initial imaging tests and therapies for the patient will be ordered by the emergency medicine physician. When the patient is stabilized, these healthcare professionals will work with the radiologist to interpret imaging tests correctly and send them to an orthopedic surgeon.
- Radiologist: This healthcare professional will assess the results of imaging tests and, if necessary, suggest additional diagnostic imaging.
- Orthopedic surgeon: Patients with Smith fractures will receive both nonsurgical and surgical care from this specialist.
- Pain management specialist: During reductive operations, this expert will administer the proper pain relief technique. If patients need more effective pain management, they could also be consulted after surgery.
- Vascular surgeon: If there is a significant vascular injury along with the Smith fracture, referrals to these specialists may be required.
Differential diagnosis:
The following is a list of differential diagnoses for trauma-related forearm deformity and pain:
- Extra-articular distal radius fracture with dorsal displacement or angulation is known as a Colles fracture.
- Intra-articular distal radius fracture with dorsal displacement or angulation is known as a Barton fracture.
- Intra-articular distal radius fracture with volar displacement or angulation is known as a reverse Barton fracture.
- Die-punch fracture- radial articular surface fracture with lunate facet depression
- Chauffer’s fracture – fracture of the styloid avulsion.
- DRUJ interference- damage to the lunate facet and the sigmoid notch of the radius
- Damage to the cartilaginous structure on the ulnar aspect of the wrist is known as a TFCC tear.
- Galeazzi fracture – fracture including disruption of the DRUJ to the distal third of the radius
It takes a careful physical examination, imaging tests, and cautious clinical judgment to distinguish between these disorders and a Smith fracture. It might be essential to consult with an orthopedic professional to ensure accurate diagnosis and suitable treatment.
Treatment of Smith fracture:
Restoring alignment and avoiding complications are the main objectives of treatment for Smith fractures. Conservative care and closed reduction are not effective for the majority of these injuries. A post-reduction X-ray with an articular step-off of 2 mm or more raises the risk of degenerative arthritis. Other indications for operational therapy include instability following first reduction, dorsal or volar comminution, intra-articular involvement, surface angulation greater than 20°, and radial shortening greater than 5 mm, in addition to significant articular step-off. Conservative treatment may be tried if none of these symptoms are evident.
Conservative Management:
The standard of care for nondisplaced, stable distal radius fractures is closed reduction followed by immobilization. In contrast to treating Colles fractures, wrist reduction, and extension splinting is necessary for Smith fractures. Procedural sedation, hematoma block, regional nerve block, intravenous regional (Bier) block, or general anesthetic are the options available for managing pain during the surgery.
There is no evidence of any variations in stable distal radius fracture splinting techniques. The application of thermoplastic braces or splints for acute distal radius fractures, however, is not supported by research. The American Academy of Orthopaedic Surgeons (AAOS) advises weekly radiographs for the first three weeks following reduction and before splint or cast removal, regardless of the splinting technique selected.
Re-reducing conservatively handled distal radius fractures did not significantly improve radiographic alignment or decrease the need for surgery, according to a retrospective cohort investigation. Conversely, re-reduction can make surgery more necessary.
Thus, before trying a Smith fracture re-reduction, other therapeutic options should be taken into account. Four weeks of immobilization by casting was proven to be an appropriate way to minimize distal radius fractures in a randomized controlled experiment.
Surgical Management:
When conservative therapy fails to reduce a Smith fracture, surgery may be considered. The size of the damage, the degree of displacement, the patient’s age, occupation, and general health all influence the surgical method that is used.
Closed reduction with percutaneous pinning (CRPP) is the initial strategy. For two or three-segment fractures, Kirschner wires are an inexpensive, minimally intrusive treatment option that often results in good functional outcomes. This method is not advised, although, in cases of comminuted fractures or when bone-weakening diseases like osteoporosis are present.
Soft-tissue damage, pin migration, fracture settlement, and pin site track infection are among the complications. External fixation is the second alternative. Ligamentotaxis is a technique used in this procedure that aligns fracture pieces by applying tension to the surrounding soft tissues.
Since the development of ORIF, the use of external fixation has been restricted to the early therapy of open fractures involving severe tissue loss or the reduction of fractures in patients with numerous traumas (polytrauma). However, because of the volar displacement of the distal portion, treating Smith fractures with external fixation is difficult. Pin-track infection, pin loosening, and complex regional pain syndrome (CRPS), which could be brought on by carpal over-distraction, are among the possible side effects of this surgery.
The third alternative is ORIF, which is now the Smith fracture surgery that is carried out the most frequently. The optimal treatment option for an unstable or irreducible Smith fracture is ORIF with locking plates acting as implants Internal fixation may be fragment-specific, volar, or dorsal. Neither AAOS nor Cochrane reviews favor one approach over another.
However, because volar plating maintains metaphyseal circulation and lowers the likelihood of extensor tendon rupture, it seems to be the best option for managing Smith fractures.
Dorsal plating is not relevant to the treatment of Smith fractures. On the other hand, because fragment-specific fixation customizes the fixing technique to unique fracture patterns, it is usually more time-consuming and more difficult to perform.
One consequence of a Smith fracture is carpal tunnel syndrome. According to one study, 4.2% of carpal tunnel release (CTR) procedures use distal-radius ORIF. Male gender, advanced age, and underweight are associated with reduced CTR rates, but intra-articular fractures with many pieces are linked to greater CTR rates.
Fractures of the distal radius can potentially cause damage to the ulnar styloid process. Research indicates that in individuals with combined distal radial and ulnar styloid fractures, conservative and surgical therapy do not significantly vary in terms of lowering ulnar-sided wrist pain and enhancing functional results. On the other hand, nonoperative management raises the possibility of nonunion, which can have a detrimental effect on functional results.
Additionally, it was discovered that ulnar styloid nonunion could be predicted in large part by the degree of preoperative displacement. When making decisions about the treatment of combined distal radial and ulnar styloid fractures, healthcare professionals can refer to this material as guidance. For patients to regain wrist strength and function, treatment and immobilization are necessary.
Post-operative Management:
Usually, stable fractures require 4–8 weeks of immobilization. After that, the patient receives bracing and rehabilitation for a further four to six weeks, or until they can move their body pain-free and with normal strength. Unstable fractures are frequently treated with rehabilitation after 6–12 weeks of immobilization until a complete range of motion and strength is restored.
During the recovery phase following surgery, pain control is a constant worry. According to one trial, transdermal buprenorphine and codeine-acetaminophen post-ORIF improved treatment compliance and functional recovery by offering better pain control than celecoxib. Nonetheless, doctors ought to make an effort to restrict the use of opioids after surgery. While managing pain during the postoperative phase, an interprofessional approach involving the operational team and primary care physician may be used.
Patients Education:
Reducing the chance of falls or other traumatic accidents that could cause this kind of wrist fracture is the first step in preventing a Smith fracture. Although traumatic situations cannot always be avoided, medical professionals can teach patients safety precautions that can help lower their chance of suffering trauma-related ailments.
The first is to put fall prevention techniques into practice at home. Some actions that may be helpful are putting handrails on stairs, utilizing non-slip flooring, making sure there is enough lighting, removing trip hazards, and encouraging family members to wear suitable footwear. The second is to follow workplace safety regulations. It’s crucial to wear the proper protective gear, stay out of dangerous situations, and adhere to machine operation safety procedures. Those who play high-risk sports have to move carefully throughout events and condition their bodies in between.
Maintaining bone health comes in third. Weight-bearing activities combined with a healthy diet can help you develop bone endurance. Assessment of the environment comes in fourth. Patients need to stay away from places and activities that could injure them. To reduce complications, patients should be counseled to seek treatment for traumatic injuries very away as a secondary preventive measure.
Physical Therapy:
Stable fracture patients are permitted to regain normal strength and range of motion gently after undergoing immobilization for four to eight weeks along with rehabilitation activities and bracing. Restoring after 6 to 12 weeks of immobilization is often necessary to restore range of motion and strength in cases of unstable fractures.
While Immobilised:
Cryotherapy and elevation are two useful methods of pain relief.
To maintain mobility and improve lymphatic drainage, encourage finger movement.
It is advised to perform exercises to increase elbow and shoulder range of motion.
After The Cast Remove:
Whether it comes from paraffin wax or a heat pack, heat can be a helpful tool for increasing the range of motion and decreasing discomfort. Cold therapy is alternated with it to improve the venous return.
Two advantages of massage include its ability to mobilize scar tissue and reduce edema.
Strength and range of motion can be enhanced with exercises for the hands, wrist, elbow, and shoulder. Paper tearing, writing, drawing, picking up small things, typing, combing, and simple tasks like buttoning clothes are among the exercises that help increase mobility.
Exercises for strengthening the wrist include squeezing a rubber ball in the troubled wrist, training the shoulder and elbow, and isometric wrist flexors and extensors.
Prognosis:
Patients recover well following a closed reduction; six weeks is typically needed for functional recovery. There is a lack of high-quality medical data about the long-term consequences of early postoperative mobilization. Strong fixation, efficient bracing, early mobilization throughout rehabilitation, and edema management are essential for athletes to get back to competing as soon as possible.
Complication:
Smith fracture complications can include:
- Acute compartment syndrome (ACS): it can cause irreversible damage to your muscles and nerves by compressing your muscles to the point where blood cannot get to the tissue.
- Malunion: During the healing process, your broken bones may move out of alignment.
- Carpal tunnel syndrome: This condition, which causes pain, numbness, and weakness in the affected hand, is often brought on by improper healing following a fractured wrist.
- Osteomyelitis, or bone infection: If you suffer an open wrist fracture that is, a fracture where the bone breaks through the skin you are more likely to get a bacterial infection.
- Additional internal damage: Broken bones can cause damage to your blood vessels, tendons, ligaments, muscles, nerves, and surrounding tissue.
- Entrapment of the extensor pollicis longus (EPL) tendon: This problem is less common in surroundings that have caused trauma. In both conservative and ORIF procedures, the extensor pollicis longus (EPL) tendon is used in the trapping of the malunion. The late split of the EPL is often mentioned in the literature. Up to around 40% of fractures have been observed to have complex regional pain syndrome (CRPS).
Prevention:
Wrist breaks are, in general, practically never deliberate. Since falls are the primary cause of wrist fractures, make sure your workspace and home are free of anything that might trip you or others. Make sure the over-50-year-old adults in your life follow adequate fall prevention practices as well.
Summary:
In any injury involving a wrist joint, Smith’s fracture—an uncommon but significant fracture—should be taken into account. The diagnosis was not made in 75% of the cases in this series.
Based on the patient’s age and X-ray appearance, Smith’s fractures can be categorized into four groups.
For the duration of the six-week period that Smith’s fractures need, the hand should be treated with maximum supination while it is in an above-elbow plaster cast.
Even with adequate therapy, all patients have some degree of disability; however, this is significantly less than in cases when the fracture is misdiagnosed, treated as a Colles’ fracture, or treated with open reduction.
FAQs
What differentiates between Smith’s and Colles fractures?
A Smith’s fracture results in volar displacement, with the shattered radius fragment projecting towards the palm side of the hand, as opposed to a Colles fracture, which causes dorsal displacement, bending the bone fragment towards the rear of the hand.
Colles or Smith, which is more common
Smith fractures are the second most common type of distal radius fractures, however far less common than Colles fractures.
What conditions must be followed for a Smith’s fracture?
The diagnostic criteria for Smith’s fracture include a deformed wrist with substantial edema on the volar side and the prominence of the ulna along the wrist’s dorsum.
What differentiates Smith’s mechanism from Colle’s?
This figure shows the many mechanisms that lead to Colles and Smith fractures. A fractured collarbone can happen when someone falls on an outstretched hand. Conversely, landing on a flexed hand causes Smith fractures.
What side effects does Smith’s fracture have?
The primary problem is wrist malunion caused by insufficient reduction or shortening of the distal radius. This could result in a “garden-spade deformity” that is permanent. Osteoarthritis and carpal tunnel syndrome are also more common in patients who have previously suffered a Smith fracture.
Which nerve is damaged in the fracture of Smith?
Acute carpal tunnel syndrome (ACTS) symptoms resulting from compression of the median nerve can occur in up to 15% of cases of Smith fractures. Less frequently, after a distal radius fracture, compression of the radial and ulnar nerves may also occur. Examining this nerve distribution may reveal sensorimotor impairments.
How could a Smith’s fracture be reduced?
The forearm must be completely supinated while the elbow is secured by a helper or with the use of a Weinberg traction device to properly reduce a Smith fracture. Completely supinate the forearm and extend the wrist to 90 degrees.
What consequences might a Smith fracture cause?
Smith’s fracture complications include extensor pollicis longus rupture and complicated regional pain syndrome, which can result in carpal tunnel syndrome or malunion, which can cause a garden spade deformity.
Reference:
- Solanki, G. (2024, January 8). Smith Fracture – Symptoms, Causes, and Treatment Options. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/smith-fracture/
- Smith’s Fracture. (n.d.). Physiopedia. https://www.physio-pedia.com/Smith%27s_Fracture/