Pulmonary Function Test
What is a Pulmonary Function Test?
The performance of your lungs is assessed by pulmonary function tests. They control how much air enters and exits your lungs, how much air enters your bloodstream, and how well your lungs function while you exercise. A few days later, you will receive a call from your healthcare practitioner with your results.
A variety of breathing tests are part of pulmonary function tests (PFTs), which evaluate how well your lungs exchange air. Your lungs facilitate the inhalation and exhalation of air.
PFTs come in a variety of forms. Some also assess the impact of exercise on the lungs and the efficiency with which oxygen is absorbed into the circulation.
PFTs are noninvasive and safe, requiring no tools or procedures to be inserted into your body by a medical professional.
Lung function tests are another name for pulmonary function tests.
Which pulmonary function test is most frequently used?
The most used kind of pulmonary function test is spirometry.
PFTs can be used in many circumstances and are typically arranged as follows:
- When patients exhibit respiratory symptoms, such as coughing, wheezing, cyanosis, or dyspnea, look for signs of respiratory disease.
- Check for any signs of lung disease development.
- Assess the effectiveness of a particular treatment.
- Assess patients before surgery.
- Keep an eye out for any potentially harmful side effects from certain medications, such as the antiarrhythmic medication amiodarone.
Types of Pulmonary Function Tests
Spirometry

- Determines lung size and measures airflow rate.
- The individual will breathe through a tube that is attached to a computer several times while exerting constant maximum effort.
- The necessary breathing effort can make some people feel dizzy or exhausted.
- Forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and the ratio of the two (FEV1/FVC) are the most often used measures; in healthy patients, these should be around 80%.
- Obstructive lung disease is indicated by an FEV1/FVC < 80%, whereas restrictive lung disease is usually characterized by a normal or elevated FEV1/FVC. Measures of flow, such as peak expiratory flow (PEF) and peak inspiratory flow (PIF), are additional valuable information obtained from spirometry.
Lung Volume Tests
The most precise method of determining how much air the lungs can store is through lung volume tests. Two methods exist for measuring lung volume:

- Body plethysmography is the most precise method. You sit in what appears to be a phone booth—a clear, sealed enclosure. You are asked to breathe in and out through a mouthpiece by the technician. The lung volume is determined in part by changes in the pressure inside the box.
- Inhaling nitrogen or helium gas through a tube for a certain period of time can also be used to assess lung volume. The lung volume is estimated by measuring the gas concentration in a chamber that is connected to the tube.
Lung Diffusion Capacity
- The lung’s diffusion capacity measures how well oxygen from the air you breathe enters your blood. For a very little period of time, usually only one breath, the patient inhales an indicator gas, which is a harmless gas.
- The gas’s concentration in the air you exhale is measured. How well gas moves from the lungs into the blood is determined by the differential between the amount of gas breathed and expelled.
- An estimate of how well the lungs transfer oxygen from the air into the bloodstream is given by this test.
Oximetry
- Oximetry is the process of using an oximeter to measure the proportion of oxygen-saturated hemoglobin in the blood.
- A reading below 90% could be a sign of an illness or impaired lung function. Noninvasive pulse oximetry measures the oxygen saturation in arterial blood using light waves and a tiny instrument placed on the fingertip or earlobe.
- A probe will be used on the finger or another skin area, like the ear, for this test. It has few or no dangers and doesn’t hurt.
Arterial Blood Gas
- The amounts of gases, including carbon dioxide and oxygen, in your blood are directly measured by arterial blood gas examinations.
- Although they can be conducted at a physician’s office, arterial blood gas tests are typically carried out in hospitals.
- Blood will be drawn for this test from an artery, typically the wrist. The amount of nitric oxide in the air you exhale is measured by fractional exhaled nitric oxide testing.
- The client will exhale into a tube attached to the portable equipment for this test. Breathing must be steady but not forceful. There aren’t many or any risks.
To evaluate lung function, further tests could be required, such as
Diffusing Capacity of Carbon Monoxide and Oxygen (DLCo):
- The lungs’ ability to diffuse gas into the blood is measured by their diffusing capacity.
- The most effective gas-to-blood diffusion occurs in the lungs when the gas may be absorbed by the blood and there is a large surface area available for transfer.
- The main use of the diffusing capacity is to differentiate between different forms of obstructive lung disease.
- For instance, in asthma, the diffusing capacity is often normal or elevated, whereas in emphysema, it is reduced.
Test for bronchodilators:
- Your lungs’ airways’ sensitivity can be evaluated via a bronchial challenge test. It helps in the diagnosis of individuals who could have asthma.
- An airway provocation test is another name for the bronchial challenge test. It includes breathing in progressively higher dosages of a drug that can restrict and irritate the airways. A far smaller dosage of this drug will have an impact on those with sensitive lungs than on those with healthy lungs. To ensure its safety, the test is conducted with great care.
- An increased sensitivity of the airways to various stimuli is one of the most common symptoms of having asthma. The diagnosis of asthma, exercise-induced asthma, or eucapnic voluntary hyperpnea may be made with the help of bronchial hyperresponsiveness if the patient has normal lung function but intermittent episodes of coughing, dyspnea, or wheezing.
Test of Cardiorespiratory Exercise:
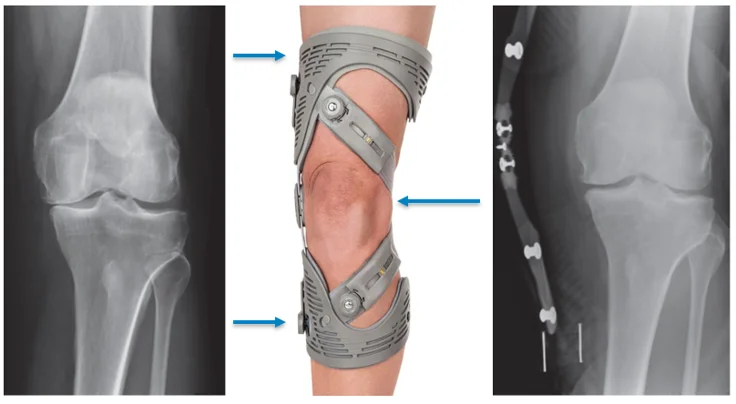
- It may be more difficult to perform daily tasks if you have lung issues. Tests of exercise capacity can be utilized to evaluate an individual’s abilities.
- The tests might assist in explaining why someone’s capacity for exercise is diminished. Anesthetic teams may also employ exercise capacity tests to determine a patient’s level of fitness, which is crucial when evaluating patients for major surgery.
- Walking tests can be used to assess the effectiveness of pulmonary rehabilitation and determine whether a client requires oxygen when walking.
Test of Respiratory Muscle Function:
- The amount of pressure that the breathing muscles can produce when an individual inhales or exhales is measured by respiratory muscle testing.
- Maximal inspiratory and expiratory pressures (MIP/MEPs) are determined by measuring the static pressures produced when the patient exerts maximal inspiratory and expiratory effort against a closed valve.
- In order to determine whether going from an upright position to a lying-down position causes a decrease in lung capacity of more than 30%, the lung specialist may additionally ask the client to perform a spirometry test while in this position. Muscle weakness is indicated by this.
Respiratory Disease Patterns
Obstruction Pattern
FEV1/FVC decrease, normal or reduced FVC, and decreased FEV1
Classically, these are the people with asthma, chronic bronchitis, or emphysema.
PFTs can assist in further differentiating the three mentioned above:
- Response to bronchodilators: a 12% rise in FEV1 after using a bronchodilator indicates asthma.
- When methacholine, histamine, or adenosine monophosphate is used to induce asthmatic blockage of reactive lower airways, bronchial provocation occurs.
- In individuals with emphysema, DLCO will drop, while in patients with asthma, it may increase or remain normal.
The difference between upper and lower airway blockage
While upper airway obstruction has impaired inspiratory capacity, which is seen on the flow volume loop (shown as flattening of the inspiratory arm), lower airway obstruction usually has reduced expiratory capacity.
Restrictive pattern
- Low DLCO, normal FEV1/FVC, and decreased TLC, FEV1, and FVC
- These individuals usually have diaphragmatic paralysis, significant skeletal deformities, or interstitial lung disease.
- Despite having reduced lung capacities, the flow volume loop appears to be normally normal.
Radiology
- Important quantitative data regarding lung function is provided by pulmonary function tests (PFTs), which can also be used to determine the pathologic conditions causing respiratory symptoms, evaluate the severity and progression of the disease, and determine whether a patient is a good candidate for lung transplantation and when.
- To reach a particular diagnosis, they are usually utilized together with chest imaging and other auxiliary information. The radiologist may be able to diagnose and grade a wide range of lung illnesses using PFTs.
Indication
- Examination of a patient exhibiting signs and symptoms of respiratory issues, such as coughing, crackles, wheezing, and abnormal chest x-rays, among other symptoms. Tracking the course of respiratory conditions and how well they respond to treatment.
- Assessment of the level of cardiorespiratory impairment
- Preoperative assessment for patients undergoing abdominal and thoracic surgery
- Patients at risk for pulmonary problems are monitored. Regular evaluation of those who are exposed to a lot of lung-hazardous agents, such as dust, fumes, and asbestos.
Contraindication
- Myocardial infarction in the last month
- Unstable Angina
- Recent thoracic and abdominal surgeries
- Recent ophthalmic surgery
- Abdominal, thoracic, and cerebral aneurysms
- Active Hemoptysis
- Pneumothorax
Risks
- Although testing for pulmonary function is a safe technique, there is reason to be concerned about adverse reactions, and the importance of the test results should be balanced against the risks.
- Shortness of breath, coughing, dizziness, pneumothorax, and triggering an asthma attack are a few of the problems.
Test Details
How do tests for pulmonary function work?
A test for pulmonary function is not too complicated. A PFT includes a mouthpiece, soft nose clips, a clear, airtight box, and a tiny electrical device called a spirometer that measures your airflow.
How can I get ready for a test of pulmonary function?
Your doctor can ask you to do the following prior to your pulmonary function test:
- For a brief time, stop using your breathing medications.
- Dress comfortably and loosely so that it doesn’t tighten your chest.
- Be clear of strenuous exertion right before the test.
- Avoid use of tobacco products prior to your test.
- Taking these procedures will help guarantee that your PFT yields accurate results.
Before a pulmonary function test, is it okay to eat?
- A large meal should not be had prior to your PFT. Caffeine should also be avoided.
What can I expect on the day of the pulmonary function test?
- In a hospital or outpatient clinic, you will take a PFT at a pulmonary function lab. Your healthcare provider will take certain personal data prior to the test, such as your height, age , weight, gender, and intercourse.
What can I hope for from a pulmonary function test?
Your healthcare professional will record your information, then send you to a room with PFT equipment and offer you instructions based on your test results.
Spirometry
- First, a medical professional will apply gentle clips to your nose. Breathing through your mouth rather than your nose is ensured by the nose clamps. A mouthpiece that is connected to a spirometer is what you will put your lips around.
- After that, the healthcare provider will instruct you on how to breathe in and out. You can inhale and exhale deeply. You can also inhale deeply and exhale as forcefully and quickly as you can.
Body Plethysmography
- You will sit in the transparent box while a medical professional puts on your nose clamps. The door will be closed by your provider. For around five minutes, the door stays closed. Inform the medical professional if you have claustrophobic discomfort in small areas.
- They might make you feel more comfortable throughout the exam. The provider will offer you instructions on how to breathe in and out while you wrap your lips around the mouthpiece. The spirometer measures the volume of your lungs by detecting variations in pressure or volume in the box while you breathe.
Gas Diffusion Study
- Your nose clips will be placed by your healthcare professional. A medical professional will instruct you on how to breathe in and out a tiny, safe quantity of carbon monoxide once you have placed your lips around the mouthpiece.
- The spirometer tracks the amount of carbon monoxide you exhale while you breathe. This measurement shows the amount of gas that was absorbed by your lungs.
Cardiopulmonary exercise test
- A medical professional will connect you to devices that take your blood pressure, oxygen levels, and heart rate. After that, you’ll either ride a stationary bike or move on a treadmill. Throughout the test, the machines will measure different parts of your heart, lungs, and muscles.
How long does a pulmonary function test take?
It could take 15 to 45 minutes to finish a PFT. If you feel fatigued throughout the test, let the doctor know. Between sections of the test, you are free to take breaks. Does testing for pulmonary function hurt? Testing for pulmonary function is not painful.
After pulmonary function testing, what can I expect?
You can resume taking any medications your doctor advised you to stop after testing. You can also resume your regular routine, which includes working out. The medical professional will keep an eye on you until your symptoms subside and you are able to return home if you had lightheadedness or dizziness during the test. When to expect your test results will be communicated by the healthcare practitioner.
The Future for PFTs
When it comes to conditions like interstitial lung disease, asthma, and COPD, pulmonary function testing is a crucial diagnostic expertise. Pulmonary function tests should become more important in detecting and measuring the physiologic changes caused by both the disease and the treatment as new and improved treatments for a variety of pulmonary disorders become available.
Physicians and technicians who are highly motivated and well-trained, who are ready to try new and better approaches to improve patient outcomes, and who pay close attention to the details of laboratory quality assurance are all necessary for this.
Interpretation
Step 1: FEV1/FVC ratio
< 70% (or below the typical lower limit) Obstructive Pattern (asthma, COPD)
≥ 70%: Restrictive or normal illness
Step 2: The obstruction’s severity (GOLD Criteria for COPD)
FEV1 anticipated to be 80–100%: Gentle (Stage 1)
FEV1 anticipated at 50–80%: Moderate (Stage 2)
FEV1 30-less than 50% expected: Extreme (Stage 3)
Predicted FEV1 < 30 percent: Extremely serious (Stage 4)
Right-sided heart failure with an FEV1 < 50%: Extremely serious (Stage 4)
Severity of obstruction
FEV1 over 70% predicted: MILD
FEV1 60-70% predicted : MODERATE
FEV1 50-60% predicted: MODERATELY SEVERE
FEV1 35-50% predicted: SEVERE
FEV1 < 35% predicted: VERY SEVERE
Step 3
≥12% increase AND an absolute improvement of at least 200 ml after inhaling a beta agonist.
FEV1 or FVC is seen as a significant reaction.
Step 4: Total Lung Capacity (TLC) (Normal range: 80-120% of predicted)
TLC > 120 = Hyperinflation
TLC < 80% = restrictive disease (ATS criteria for severity)
70-80% predicted: MILD
60-70% predicted: MODERATE
50-60% predicted: MODERATELY SEVERE
<50% predicted: SEVERE
Step 5: RV/TLC ratio (normal range: <35% or < predicted)
RV/TLC > 35% or > predicted indicates Air trapping
Step 6: DLCO (Normal range: 80-120% of predicted)
- In obstructive disease:
- Decreased in Emphysema
- Normal in chronic bronchitis
- Normal or increased in asthma
- In restrictive disease:
- Decreased in parenchymal disease
- Normal in non-parenchymal (e.g., chest wall) restriction
FAQs
What is the test for pulmonary function?
In order to identify and manage lung disorders, a series of examinations known as pulmonary function tests (PFTs) measure your lungs’ capacity, airflow, and gas exchange.
What does a typical PFT score mean?
An FEV1/FVC ratio of more than 0.70 and both FEV1 and FVC above 80% of the expected value are considered normal spirometry data. TLC above 80% of the predictive value is considered normal if lung volumes are performed. Additionally, a diffusion capacity above 75% of the expected value is regarded as typical.
Which three components make up a pulmonary function test?
The test consists of three parts:
Spirometry: You’ll hold your breath and exhale quickly. To evaluate your maximal effort, spirometry is performed at least three times.
Diffusion: For ten seconds, you will hold your breath.
Lung Volume: You will inhale various air mixes.
Does a PFT test hurt?
Although pulmonary function tests (PFTs) usually don’t hurt, you may have some short-term discomfort or adverse effects, such as coughing, lightheadedness, or dizziness, during or after the test.
A low PFT score: what is it?
To pass the PFT, you must have a minimum overall score of 150. 300 is the highest possible score. Because of the way event scoring is set up, passing the PFT requires more than just achieving the minimal score in each event; you also need to score extra points in at least one event to reach the passing threshold overall.
Is it possible for PFT to identify pneumonia?
The doctor may suggest one or more pulmonary function tests to assess how well your lungs are supplying oxygen to your body because pneumonia directly affects the lungs. Pulse oximetry is one kind of pulmonary function test that determines whether your blood has adequate oxygen.
Can cardiac issues be detected by PFT?
Prior to surgery or other procedures, lung function can be assessed using PFTs. People who smoke, have heart or lung issues, or have other medical disorders may have this procedure. PFTs are also used to evaluate the course of treatment for chronic lung conditions such as emphysema and asthma.
References
- Professional, C. C. M. (2025, March 19). Pulmonary function testing. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/17966-pulmonary-function-testing
- Ponce, M. C., Sankari, A., & Sharma, S. (2023, August 28). Pulmonary function tests. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482339/
- Wikipedia contributors. (2024, November 2). Pulmonary function testing. Wikipedia. https://en.wikipedia.org/wiki/Pulmonary_function_testing