Psoriatic Arthritis
Psoriatic Arthritis: What Is It?
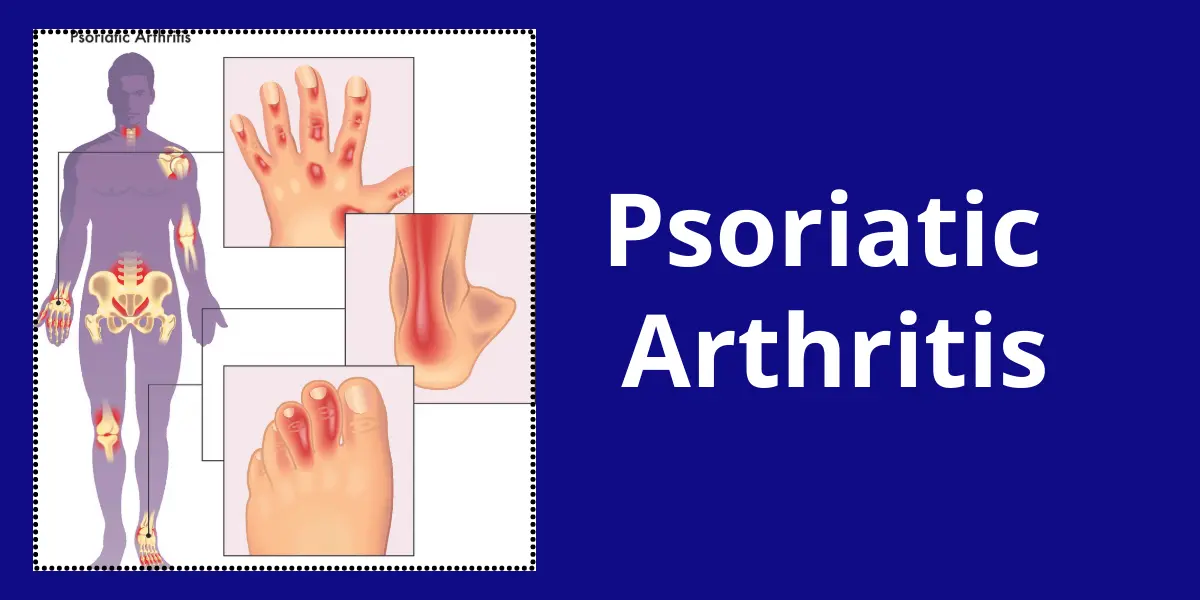
Psoriatic Arthritis (PsA) is a chronic inflammatory condition that combines joint inflammation (arthritis) with skin lesions of psoriasis. It is an autoimmune disorder where the immune system mistakenly attacks healthy tissues, leading to joint pain, stiffness, and swelling, often in the fingers, toes, and spine.
One frequent condition that affects your joints is arthritis. It makes the area surrounding your joints painful and inflamed. Psoriasis causes inflammation of the skin. Scale-covered areas of discolored skin are known as psoriasis rashes. Plaques are these thick, scaly patches. Additionally, it may cause your toenails and fingernails to thicken and seem pitted or flaky (covered with small indentations).
Psoriasis and arthritis are both autoimmune diseases. You might develop an autoimmune illness when your immune system unintentionally targets your body rather than defending it. When you experience joint inflammation and psoriasis symptoms on your skin, you have psoriatic arthritis.
The skin and joint symptoms of psoriatic arthritis often flare up and subside throughout these intervals. A medical professional will provide therapies to alleviate your symptoms during a flare.
If you have any new skin problems or joint pain, edema, or stiffness, see a doctor.
Causes of Psoriatic Arthritis:
When your body’s immune system targets healthy cells and tissue, psoriatic arthritis develops. The immunological reaction results in an excess of skin cells and joint inflammation.
This immune system response appears to be influenced by both environmental and genetic variables. Many psoriatic arthritis sufferers have a family history of the condition or psoriasis. Certain genetic markers that seem to be connected to psoriatic arthritis have been found by researchers.
People with a genetic predisposition to psoriatic arthritis may develop it as a result of environmental factors, such as bacterial or viral infections, or physical trauma.
Which five types of Psoriatic Arthritis exist?
A medical professional may categorize psoriatic arthritis according to the joints it affects or the side of the body where symptoms are felt. The following are the five types of psoriatic arthritis:
Distal interphalangeal predominant psoriatic arthritis: The joints close to the tips of your fingers and toes (phalanges) are affected by distal interphalangeal predominance psoriatic arthritis. Your fingernails and toenails are affected by the most prevalent kind of psoriatic arthritis. Your nails may appear pitted, flaking, or discolored.
Symmetric polyarthritis: Polyarthritis that affects five or more joints simultaneously is known as symmetric polyarthritis. The same joints on both sides of your body are impacted by symmetric polyarthritis. For instance, both of your elbows and both of your knees. This kind of psoriatic arthritis is among the most prevalent.
Asymmetric oligoarticular psoriatic arthritis: One knee and one elbow, for instance, are affected by asymmetric oligoarticular psoriatic arthritis, which affects two to four joints on both sides of the body. Along with symmetric polyarthritis, it is the other most prevalent kind of psoriatic arthritis.
Spondylitis: The vertebrae (plural of vertebra) are the 33 bones that make up your spine. Inflammation and other symptoms in the joints between your vertebrae are caused by spondylitis. Additionally, it may result in shoulder and hip discomfort.
Arthritis mutilans: Your hands and feet may experience significant symptoms from arthritis mutilans. Usually, the inflammation is so severe that it results in osteolysis or bone loss. This kind of psoriatic arthritis is the rarest. Arthritis mutilans affect less than 5% of psoriatic arthritis patients.
What are the symptoms of Psoriatic Arthritis?
Any joint in your body may be impacted by psoriatic arthritis. There may be minimal indications of psoriasis on your skin, along with moderate discomfort and stiffness. In addition to causing bigger psoriasis patches on your skin, more severe flare-ups of psoriatic arthritis can make it difficult or impossible to move and utilize joints.
The following are the most typical signs of psoriatic arthritis:
- Joint pain.
- Stiffness.
- Redness or discoloration of the area around your affected joints.
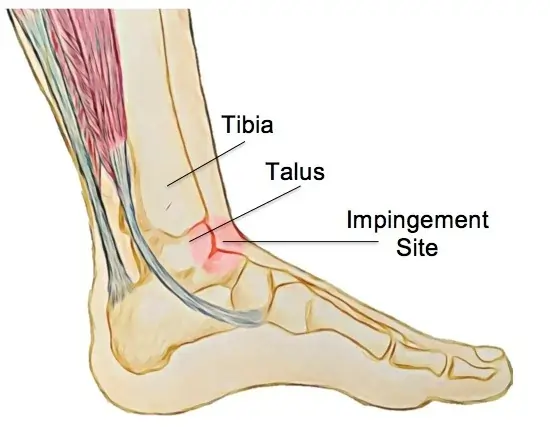
- Where tendons and ligaments connect to your bones, such as close to your Achilles tendon, you may experience pain or soreness.
- Dactylitis, sometimes known as “sausage fingers,” is swelling in your fingers and toes.
- Silver or grey scaly areas on your skin, particularly on your scalp, elbows, knees, and lower back, are known as psoriasis rash.
- Discoloration or pitting on your fingernails or toenails are signs of nail psoriasis.
- Exhaustion.
How often does it occur?
Psoriatic arthritis affects less than 1 percent of the population. However, those who have psoriasis are far more likely to have it. Psoriatic arthritis affects around 30% of individuals with psoriasis at some time in their lives.
Diagnosis:
Throughout the examination, your physician may:
- Look for indications of soreness or swelling in your joints.
- Examine your fingernails for any irregularities, such as pitting or flaking.
- To feel for any sore spots, apply pressure to the soles of your feet and the region surrounding your heels.
A diagnosis of psoriatic arthritis cannot be verified by a single test. However, certain tests can rule out other conditions like gout or rheumatoid arthritis that can cause joint discomfort.
Imaging examinations:
X-rays. These can assist in identifying joint abnormalities that are specific to psoriatic arthritis but absent from other arthritic diseases.
MRI. This creates fine-grained pictures of your body’s soft and hard tissues using radio waves and a powerful magnetic field. An MRI can be used to look for issues with your lower back and foot tendons and ligaments.
Laboratory tests:
Rheumatoid factor (RF). People with rheumatoid arthritis frequently have rheumatoid factor (RF), an antibody, in their blood, whereas those with psoriatic arthritis typically do not. Your doctor can use this test to help you differentiate between the two disorders.
Joint fluid test. The doctor may take a little sample of fluid with a needle from one of your affected joints, usually the knee. If you have crystals of uric acid in your joint fluid, you may have gout instead of psoriatic arthritis. Additionally, psoriatic arthritis and gout can coexist.
Treatment of Psoriatic Arthritis:
There is no recognized cure for psoriatic arthritis. Treatment focuses on controlling skin involvement and lowering inflammation in the affected joints to prevent joint pain and disability. Among the most popular treatments are prescription medications referred to as disease-modifying antirheumatic medicines (DMARDs).
The way you are treated depends on the extent of your disease and the affected joints. You might need to try a few different therapies before you discover one that suits you.
Medication:
The following medications are used to treat psoriatic arthritis:
NSAIDs. For those with moderate psoriatic arthritis, nonsteroidal anti-inflammatory medications (NSAIDs) help decrease inflammation and alleviate discomfort. Ibuprofen (Advil, Motrin IB, and others) and naproxen sodium (Aleve) are examples of nonsteroidal anti-inflammatory medications (NSAIDs) that are accessible without a prescription. Prescriptions are available for stronger NSAIDs. Liver and kidney damage, cardiac issues, and stomach discomfort are possible side effects.
Conventional disease-modifying antirheumatic medications (DMARDs). These medications can prevent irreversible damage to joints and other tissues by slowing the course of psoriatic arthritis.
Methotrexate is the most widely used disease-modifying antirheumatic medication (DMARD) (Trexall, Otrexup, etc.). Sulfasalazine (Azulfidine) and leflunomide (Arava) are two more. Liver damage, bone marrow suppression, lung inflammation, and scarring (fibrosis) are possible side effects.
Biologic agents. This type of DMARD, sometimes referred to as a biological response modifier, targets several immune system pathways. Ustekinumab (Stelara), secukinumab (Cosentyx), ixekizumab (Taltz), guselkumab (Tremfya), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), adalimumab (Humira), certolizumab (Cimzia), and abatacept (Orencia) are examples of biologic drugs. These medications may make infections more likely.
Targeted synthetic DMARDs. If biologic medicines and traditional DMARDs have not worked, tofacitinib (Xeljanz) may be taken. Increased tofacitinib dosages may raise the risk of cancer, major heart-related events, and pulmonary blood clots.
Newer oral medication. Apremilast (Otezla) reduces the body’s activity of an enzyme that regulates cell-level inflammation. People with mild to severe psoriatic arthritis who cannot or do not wish to use DMARDs or biologic medicines are treated with apremilast. Headaches, nausea, and diarrhea are possible adverse effects.
Therapies
Occupational and physical therapy may reduce discomfort and facilitate daily activities. Consult your physician for recommendations. Additionally, massage treatment may assist.
Surgery and other procedures:
Steroid injections. Inflammation can be decreased using injections into the affected joint.
Joint replacement surgery. Artificial joints composed of plastic and metal can be used to replace some joints that have been badly destroyed by psoriatic arthritis.
Risk factors of Psoriatic Arthritis:
Your chance of developing psoriatic arthritis can be raised by several variables, such as:
- Psoriasis. The single biggest risk factor for psoriatic arthritis is having psoriasis.
- Family history. Many psoriatic arthritis sufferers have a sibling or parent who also has the condition.
- Age. Psoriatic arthritis can strike anybody, however, most usually strikes people between the ages of 30 and 55.
What are the Complications of Psoriatic Arthritis?
Psoriatic arthritis patients have an increased risk of developing other medical disorders, such as:
- High blood pressure (hypertension).
- High cholesterol (hyperlipemia).
- Obesity.
- Diabetes.
- Depression.
- Anemia.
- Muscle weakness.
Symptoms of psoriatic arthritis can make using your joints unpleasant or challenging. Getting adequate exercise may become difficult as a result. Discuss low-impact workouts that relieve joint strain with your healthcare professional. You may exercise without putting too much strain on your joints by doing yoga, walking, or aqua therapy.
How do I control my symptoms?
In addition to taking prescription medicine, there are other things you may do to assist reduce your symptoms.
Keeping active
Having arthritis might make it difficult to stay active. Many people are afraid of injuring themselves or causing more joint injury. However, the fact is that maintaining an active lifestyle may alleviate your symptoms.
Maintaining an active lifestyle will strengthen your muscles, increase joint mobility, and lessen pain and tiredness. It’s also beneficial to your emotional well-being.
Your first few workouts may be a little sore if you’ve never worked out before or haven’t done it in a long time. However, it will become easier if you persevere.
Remember that any activity is better than none at all, so start small. Because your body is made to move, taking too much time off can damage your joints and the tissues that surround them.
Exercise in a group setting or with a friend might be beneficial if you’re struggling to maintain your motivation. It may also be a fantastic opportunity to meet new people and mingle.
Nutrition
Psoriatic arthritis cannot be cured by any diet.
Your general health and wellness will benefit from eating a nutritious, well-balanced diet that is low in fat, salt, and sugar. If you have psoriatic arthritis, this is very crucial.
Being overweight will increase the pressure on your back, knees, and hips. Your heart will benefit from a nutritious diet as well.
Drinking around two liters of water each day and eating a lot of fresh fruit and vegetables are also beneficial to your health.
Complementary treatments:
Complementary therapies can be beneficial for some psoriatic arthritis sufferers, but you should always see your doctor before trying them.
There are many different historical and cultural origins for complementary therapies. They differ from mainstream or traditional medications and therapies that are provided by physiotherapists, rheumatology teams, or general practitioners.
Complementary treatments include, for example:
- Acupuncture – In acupuncture, tiny needles are placed at various body locations to activate nerves and release endorphins, which are endogenous painkillers.
- The Alexander Technique is predicated on the idea that better posture and mobility may be achieved by having a thorough awareness and understanding of the body. According to those who teach it, it relieves physical strain.
Additionally, there are alternate medications that may be administered topically or consumed as tablets. Among these are fish body oil capsules, which contain omega-3 fatty acids, which are believed to offer several health advantages, including lowering inflammation. According to some research, eating fish like salmon, sardines, and mackerel is a far better way to receive these nutrients than taking supplements.
It’s crucial to see a therapist who is fully insured, has an established ethical code, or is legally registered because certain complementary therapies might have hazards.
Consider how treatments or supplements are helping you when you choose to try them, and then determine whether to keep going based on whether you see any progress.
Sunshine
At least temporarily, psoriasis can be improved with the correct quantity of sunlight. On the other hand, excessive sun exposure and sunburn can exacerbate psoriasis.
Smoking
Smoking can exacerbate psoriasis. Additionally, it may make possible complications like cardiac issues more likely.
FAQs
Can someone with psoriatic arthritis lead a normal life?
Because PsA differs from person to person, it is difficult to predict with precision how it will impact a person’s life. Some people do have significant symptoms and early and rapid progression of the illness. Others experience PsA with slow-moving symptoms that don’t significantly affect their lives.
What causes arthritis caused by psoriasis?
These elements consist of: Genes: Researchers have discovered some of the genes that contribute to psoriatic arthritis, and many individuals who develop the condition have a family history of it. Environment: The condition may start as a result of stress, injury, infection, or obesity.
Which pain reliever works best for psoriatic arthritis?
For those with moderate psoriatic arthritis, nonsteroidal anti-inflammatory medications (NSAIDs) help decrease inflammation and alleviate discomfort. Ibuprofen (Advil, Motrin IB, and others) and naproxen sodium (Aleve) are examples of nonsteroidal anti-inflammatory medications (NSAIDs) that are accessible without a prescription.
Is it possible for psoriatic arthritis to resolve itself?
Periods of remission may alternate with flare-ups of psoriasis or psoriatic arthritis. Psoriatic arthritis does not currently have a cure. The goals of treatment are to manage symptoms and avoid joint injury. Psoriatic arthritis can be incapacitating if left untreated.
Which diet is ideal for those with psoriasis arthritis?
In addition to treating psoriatic arthritis or psoriasis, a Mediterranean diet can help lower chronic inflammation, which is linked to cancer, heart disease, type 2 diabetes, and other illnesses. Fish, lean protein, and plant-based proteins like tempeh or tofu are the ideal meals for those with psoriasis. Veggies and fruits.
What is psoriatic arthritis’s initial warning sign?
Keep an eye out for these potential early indicators of psoriatic arthritis if you have psoriasis or other risk factors for PsA, especially if you have many symptoms: scaly areas of silvery white skin or a dense, red rash. Joints that are heated, swollen, painful, and stiff—whether they are little like your fingertips or huge like your knees.
References
- Psoriatic arthritis – Symptoms & causes – Mayo Clinic. (2021, October 2). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/symptoms-causes/syc-20354076
- Psoriatic arthritis. (2024, September 9). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/13286-psoriatic-arthritis
- Psoriatic arthritis. (n.d.). Versus Arthritis. https://versusarthritis.org/about-arthritis/conditions/psoriatic-arthritis/






One Comment