Pneumothorax Physical Therapy Treatment
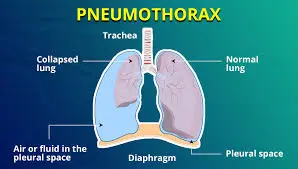
Pneumothorax, or collapsed lung, involves the accumulation of air in the pleural space, causing lung compression and impaired breathing.
Physical therapy for pneumothorax focuses on promoting optimal lung expansion, improving respiratory function, and preventing complications.
Treatment typically includes breathing exercises, gentle thoracic mobility techniques, posture training, and gradual reconditioning to restore normal function. Therapy is tailored to the individual’s condition, emphasizing safety and collaboration with the healthcare team to support recovery.
What is a Pneumothorax?
The normal expansion of the lungs is partly facilitated by the pleural layers surrounding them. The parietal pleura, which is the outer layer, lines the chest cavity’s interior. The visceral pleura, which is the counterpart of this layer, covers the lung’s outer surface.
A small quantity of fluid exists between these pleural layers to minimize friction as they move against one another. This very slim space between the pleural layers operates as a closed system under negative pressure.
Consequently, when the chest wall rises and expands, it effectively pulls the lung wall upward and outward, promoting an increase in lung volume during inhalation. The lungs naturally deflate easily during exhalation due to their elastic recoil.
A pneumothorax occurs when the negative pressure in the pleural space is disrupted, allowing gas (typically air) to enter the area between the pleural layers. In the absence of the negative pressure pull, the two pleural layers cease to move in synchronization, and the lung tissue collapses due to its elastic recoil. The extent of this collapse is influenced by the size of the breach and the volume of air that enters the pleural space.
Types of pneumothorax
Pneumothorax can be categorized into three main types based on their cause:
- Traumatic – caused by blunt or penetrating trauma to the chest. Most pneumothorax cases are of this type.
- Iatrogenic – resulting from interventions performed by healthcare providers, such as the insertion of central lines. a subset of traumatic pneumothorax, occurs when an injury results from a medical procedure or intervention (e.g., insertion of a central line).
- Spontaneous – occurring without any obvious cause or triggering event. primary spontaneous pneumothorax occurs in individuals without preexisting lung conditions or an initiating event, while secondary spontaneous pneumothorax happens in those with significant underlying lung disease and arises from a specific triggering event, such as the rupture of a bleb.
- Catamenial – a type of non-traumatic pneumothorax that arises in females during their menstrual cycle. Although the underlying mechanism is not completely understood, it is thought to be linked to endometriosis of the pleura.
Pneumothorax can also be further classified into the following types based on their physiological effects:
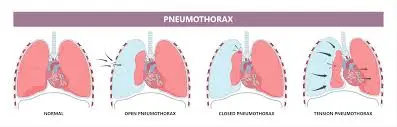
- Simple – occurs when the air within the pleural space does not connect with the outside atmosphere, and there is no shift in the mediastinum or hemidiaphragm. An example would be a pleural laceration from a fractured rib.
- Communicating – takes place when there is an opening in the chest wall, such as from a gunshot wound, that creates a direct link to the external atmosphere. This loss of chest wall integrity can lead to an air-sucking phenomenon and paradoxical lung collapse, resulting in considerable respiratory issues.
- Tension – characterized by a continuous accumulation of air in the pleural cavity that displaces the mediastinum to the opposite side, leading to the compression of the vena cava and other major vessels, reduced diastolic filling, and ultimately impaired cardiac output. This situation arises when a chest injury creates a one-way valve effect, allowing air to enter the pleural cavity but not to escape.
What signs indicate a collapsed lung, or pneumothorax?
The following are indications of a pneumothorax:
- Pain in the chest on one side, especially during breathing.
- Coughing.
- Rapid breathing.
- Elevated heart rate.
- Fatigue.
- Difficulty breathing (dyspnea).
- A bluish shade of the skin, lips, or nails is called cyanosis.
If you experience indications of a collapsed lung, seek immediate assistance at the nearest emergency department. Urgent care may be necessary.
Pneumothorax has three primary causes: medical conditions, injuries, and lifestyle factors.
Medical conditions:
- Asthma.
- Pneumonia.
- Chronic obstructive pulmonary disease (COPD).
- Collagen vascular diseases.
- Cystic fibrosis.
- Emphysema.
- Idiopathic pulmonary fibrosis.
- Lung cancer.
- Lymphangioleiomyomatosis.
- Tuberculosis.
- Acute respiratory distress syndrome (ARDS).
Injuries:
- Blunt force trauma.
- Gunshot wounds.
- Stab wounds.
- Medical procedures, including nerve blocks, lung biopsies, the placement of central venous lines, or mechanical ventilation.
Lifestyle Factors
- Use of drugs, particularly inhaled substances.
- Smoking habits.
- Traveling by air with significant fluctuations in air pressure.
- Scuba diving or deep-sea diving activities.
Epidemiology
The occurrence of non-traumatic pneumothorax ranges from 7.4 to 18 per 100000 individuals annually.
This rate is considerably higher among smokers (12% compared to 0.1% lifetime risk).
Primary spontaneous pneumothorax typically affects young males, often tall and slender, usually smokers. The likelihood of recurrence is between 20 to 60% within the first three years following the initial incident.
Secondary spontaneous pneumothorax can also affect patients with pre-existing lung diseases, leading to significant variation in epidemiology.
Catamenial pneumothorax is seen in young women who are of childbearing age.
What Are the Symptoms of a Pneumothorax?
The symptoms of pneumothorax can vary widely depending on the original cause and severity. Mild cases may show no signs and can only be identified during examinations for related issues. In more severe instances, common symptoms can include:
- breathing difficulties brought on by a decreased lung capacity.
- Shallow and potentially rapid breathing as a compensatory mechanism for decreased volume.
- Sharp, stabbing chest pain during respiration.
- Reduced chest expansion on the side affected by the pneumothorax.
- Increased heart rate as compensation for lowered blood oxygen levels.
- Feelings of anxiety, decreased alertness, and confusion.
- When examined with a stethoscope, normal breath sounds may be notably faint or absent on the side where the pneumothorax has occurred.
How Is a Pneumothorax Diagnosed?
A healthcare professional can diagnose pneumothorax through a thorough investigation of your symptoms, medical background, and specific tests to exclude other potential conditions. Auscultation with a stethoscope for breathing sounds is an effective diagnostic tool to identify a pneumothorax.
If you believe you may have pneumothorax, it’s crucial to seek medical help without delay. If not treated, a severe pneumothorax could cause a displacement of the heart and aorta, leading to irregular pressures and possible heart failure.
Once diagnosed and stabilized, an evaluation of your current lung function can be performed to tailor appropriate treatments.
Imaging
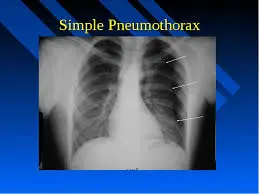
Chest X-rays will subsequently be employed to confirm the pneumothorax diagnosis. In a supine chest X-ray, a deep sulcus sign is indicative, characterized by a low lateral costophrenic angle on the affected side. Additionally, the presence of air outside normal lung airways and the movement or displacement of organs away from the air leak within the thoracic cavity will suggest a pneumothorax.
Ultrasound scans can also aid in diagnostic assessment.
What Would a Physiotherapy Assessment for a Pneumothorax Involve?
During your initial appointment, our physiotherapists will conduct an assessment consisting of two components:
Subjective
A conversation between you and the physiotherapist to determine the symptoms you are experiencing and the impact of your condition on your lifestyle.
Objective
An evaluation to identify any pain, your current breathing pattern, respiratory rate, lung volume, and several specific tests to assess mucus retention and lung function impairment.
There can be significant variation in displayed symptoms, influenced by the progression of the condition and any complicating factors. The assessment process will be critical in identifying your current symptoms and needs, allowing for targeted and effective treatments.
What Would Physiotherapy Treatment for a Pneumothorax Involve?
Indications for physiotherapy in cases of pneumothorax include:
- Lung collapse
- Sputum retention
- Ventilation/perfusion (V/Q) mismatch
- Increased effort in breathing
- Abnormalities in blood gases
- Post-operative care in an intensive care unit (ITU)
Goals for Physiotherapy
The objectives of physiotherapy management are as follows:
To enhance ventilation and elevate PaO2 levels
- Participate in physical activities such as climbing stairs, walking, and engaging in moderate-intensity aerobic exercise.
- Perform active cycles of breathing exercises.
- Utilize techniques for sputum removal, including percussion and cough assistance.
- Employ Positive Expiratory Pressure (PEP) devices.
- Practice incentive spirometry.
- Use non-invasive ventilation (NIV).
To aid in sputum elimination
- Implement postural drainage techniques.
- Carry out active cycles of breathing exercises.
- Apply percussion, shaking, and vibrations.
- Use PEP devices.
- Engage in physical activities such as stair climbing, walking, and moderate-intensity aerobic exercise.
- Practice coughing and huffing (forced expiratory breathing).
- Conduct airway suctioning.
To lessen the work of breathing
- Optimize body positioning.
- Practice techniques for breathing control.
- Use relaxation methods.
- Employ strategies for utilizing accessory muscles.
To enhance exercise capability
- Initiate early mobilization and proper positioning.
- Adhere to a structured exercise regimen.
- Engage in breathing exercises.
- Physiotherapy Outcome Evaluation:
- Monitor respiratory rate.
- Track O2 saturation levels.
- Evaluate arterial blood gases.
- Identify any additional O2 needs.
- Conduct auscultation.
- Examine chest X-ray.
- Assess mobility status.
Pneumothorax Physical Therapy Treatment Includes
Grasping the concept of pneumothorax is vital for physiotherapists, especially those preparing for the APC exam. The ability to recognize and manage this condition allows physiotherapists to facilitate better recovery for patients.
After identifying and treating the cause of the pneumothorax, and reducing or eliminating the trapped air, rehabilitative care can commence. Depending on the severity and duration of your condition, your treatment may include:
Secretion clearance:
Techniques for effective or productive coughing.
Postural drainage while sitting and lying down.
Manual assistance methods, such as percussion, vibrations, and shaking.
Breathing technique retraining:
- Managing respiratory rate.
- Practicing diaphragmatic breathing.
- Controlling or reducing breath volume.
- Conducting relaxation breathing exercises.
- Education and Advice:
- Understanding the causes and progression of the illness.
- Recognizing the impact of environmental and allergen factors.
Observation
If a pneumothorax is caused by a minor injury, it might heal on its own within a few days. Consult a doctor before engaging in flying or diving after experiencing a pneumothorax.
If you’re experiencing breathing difficulties, supplemental oxygen may be necessary. Using oxygen can also help accelerate the rate at which the lungs absorb air from the cavity.
Draining excess air
Needle aspiration and chest tube insertion are two procedures designed to extract extra air from the pleural space in the chest. These can be performed bedside without the need for general anesthesia.
In cases of significant damage or severe symptoms, surgical intervention may be required to remove the air or perform surgery.
In needle aspiration, the physician inserts a needle into the cavity and removes the air using a syringe.
For chest tube insertion, a doctor will place a hollow tube between your ribs to allow air to escape and the lung to reinflate. The tube may need to remain in place for 2 to 5 days or longer.
Surgery
A doctor may need to perform a more invasive procedure to examine the status of your lungs, such as a thoracotomy or thoracoscopy.
During a thoracotomy, your surgeon will make an incision in the pleural space for better visibility of the problem. During a thoracoscopy, also referred to as video-assisted thoracoscopic surgery (VATS), a doctor inserts a small camera through the chest wall for lung examination.
If you have experienced recurrent episodes of pneumothorax, you might need minor surgery to repair weak areas in the lung where air is leaking. The doctor may also perform pleurodesis, which involves attaching the lung to the chest wall.
Other surgical options include:
- Suturing blisters closed,
- Sealing air leaks,
- Or resecting the collapsed part of your lung, known as a lobectomy.
- These procedures can minimize the likelihood of recurring pneumothorax.
How can I schedule a physiotherapy evaluation for pneumothorax?
If a doctor has diagnosed you with pneumothorax and you are facing symptoms that affect your breathing and lung clearance, it would be beneficial to seek an assessment from one of our skilled respiratory physiotherapists.
How severe is a punctured lung?
The severity of a punctured lung varies based on its cause and the extent of lung collapse. Certain cases are not serious, while others may pose medical emergencies. A healthcare provider can assess how much of your lung is affected and suggest appropriate treatment options.
What can I anticipate if I have a pneumothorax?
If you suffer from a collapsed lung, you might need to stay in the hospital for a few days or longer for treatment and monitoring. This ensures that your healthcare provider can assess your condition and provide oxygen if needed.
How long does it take for a punctured lung to heal?
Typically, a punctured lung can heal within several days to two weeks. Your body will reabsorb the excess air surrounding your lung, allowing it to reinflate.
Is it possible to fully recover from a punctured lung?
Most individuals with a punctured lung recover without significant medical intervention. However, there is a possibility of recurrence. It’s advisable to discuss your chances of recurrence with your healthcare provider and inquire about steps to take if symptoms return.
Is pneumothorax life-threatening?
Certain instances of pneumothorax can be life-threatening. A healthcare provider should always monitor a collapsed lung.
Living With
How can I take care of myself?
After returning home from the hospital, it’s essential to follow your provider’s suggestions for self-care. They might advise you to rest and limit or avoid specific activities, including:
- Smoking.
- Air travel.
- Scuba or deep-sea diving.
- Ensure you attend all your follow-up appointments with your provider after leaving the hospital.
When should I contact my healthcare provider?
Reach out to your provider if your symptoms return or worsen. If you have experienced a pneumothorax in the past, you might be at greater risk of it occurring again.
When should I visit the ER?
Seek emergency care if you have signs of a collapsed lung. You might require immediate medical attention.
What questions should I pose to my doctor?
It may be beneficial to ask your provider:
- What led to my collapsed lung?
- What treatment options are available to me?
- If I require a chest tube, how long will I need it?
- Will I need supplemental oxygen?
- Will I have to remain in the hospital?
- What kind of care will I require post-treatment?
- What kind of care will I need once I leave the hospital or clinic?
- What should I refrain from doing after my treatment?
Complications
Misdiagnosis is a common complication of pneumothorax. Various factors, such as an incomplete or insufficient medical history or physical examination, low clinical suspicion, failure to get a chest X-ray, or failure to identify a pneumothorax on a chest radiograph, can contribute to this misdiagnosis. Such errors can result in a lack of treatment for the pneumothorax and, in certain situations, could lead to severe consequences, such as:
- Progression to tension pneumothorax
- Hypoxemic respiratory failure
- Shock
- Respiratory arrest
- Cardiac arrest
- Empyema
- Re-expansion pulmonary edema
- While most collapsed lungs recover without complications, some individuals may experience serious issues. These can include:
- Damage or infection resulting from the treatment.
- Iatrogenic complications from needle decompression or thoracostomy procedures – such as failure of the lung to re-expand, lung laceration, infection at the insertion site and within the pleural space, tearing of intercostal vessels or the internal mammary artery, hemothorax, ongoing air leaks, or damage to the intercostal neurovascular bundle.
- Chest tube-induced arrhythmia
- Pneumomediastinum – air from the pneumothorax may migrate into the mediastinum, visible on a chest X-ray as air lucency around the heart. Also, a crunching sound could be heard during a cardiac examination. This phenomenon, known as Hamman’s crunch, is best detected while lying in the left lateral decubitus position.
Risk factors for Pneumothorax
The risk factors differ between traumatic and spontaneous pneumothorax.
Risk factors for a traumatic pneumothorax include:
- Contact sports, such as football or hockey
- Jobs where there is a risk of falls or other injuries
- Medical procedures involving the chest or lung area
- Ongoing assisted respiratory care
Individuals at increased risk for non-traumatic pneumothorax include those who:
- Smoke
- possess an underlying lung disease, such as COPD or asthma.
- Have a family history of pneumothorax, suggesting possible genetic factors
- Possess tall, lean body types, as this can influence the pressure at the top of the lung
- Experience inflammation in the small airways
- You might have a higher risk of a collapsed lung if you:
- Are pregnant.
- Have a tall, thin physique, particularly as a man.
- Have Marfan syndrome.
- Have endometriosis.
Summary
Pneumothorax is a condition characterized by air accumulation between the lungs and the chest cavity. It may resolve on its own in some cases, while in others, it can be life-threatening. The severity depends on the size and cause of the issue.
There are various forms of pneumothorax. Traumatic pneumothorax occurs as a result of injury to the chest wall or lungs. Non-traumatic pneumothorax can impact individuals with COPD and other lung disorders but can also affect those without respiratory conditions.
Treatment focuses on removing the air and allowing the lungs to re-expand. In certain situations, surgical intervention may be necessary to repair the lungs. Pneumothorax can represent a life-threatening emergency. Anyone experiencing symptoms like sharp, stabbing chest pain should seek immediate medical assistance.
FAQs
Is exercising advisable for pneumothorax?
There is no evidence linking physical activity to pneumothorax, so you can resume activity as soon as your symptoms have resolved. However, it’s wise to wait until you have fully recovered and attended your follow-up appointment before engaging in intense workouts or contact sports.
What is the most effective treatment for pneumothorax?
Pathophysiology of Pneumothorax
In pneumothorax, air enters the pleural cavity either from the external environment or from the lung itself through mediastinal tissues or direct perforation of the pleura. The increase in intrapleural pressure leads to a reduction in lung volume.
What is PT for a collapsed lung?
Chest physical therapy
Engaging in deep-breathing exercises using an incentive spirometer, followed by forceful coughing to assist in clearing the lungs… Adjusting your position so that your head is lower than your chest… Gently tapping on your chest over the affected area to help loosen mucus.
What exercise is good for the lungs?
Physical exercise to improve breathing
Some examples of beneficial physical activities include: Walking – begin with a few minutes each week and gradually increase the duration. Stretching – maintain flexibility in your muscles. Weight training – utilize small hand-held weights.
What is the physiopathology of a pneumothorax?
Pathophysiology of Pneumothorax
In pneumothorax, air enters the pleural cavity either from the external environment or from the lung itself through mediastinal tissues or direct perforation of the pleura. The increase in intrapleural pressure leads to a reduction in lung volume.
References
- Pneumothorax (Collapsed lung). Healthline. https://www.healthline.com/health/collapsed-lung
- (n.d.) https:/www.physio-pedia.com/Pneumothorax
- Pneumothorax – restrictive – conditions – respiratory – what we treat – physio.co.uk. (n.d.). https://www.physio.co.uk/what-we-treat/respiratory/conditions/restrictive/pneumothorax.php
- (n.d.). https://www.ncbi.nlm.nih.gov/books/NBK538316/.
- https://www.ncbi.nlm.nih.gov/books/NBK538316/
- Cnsc, B. J. D. M. M. F. F. (n.d.). Pneumothorax treatment & management: approach considerations, treatment based on risk stratification, options for restoring Air-Free pleural space. https://emedicine.medscape.com/article/424547-treatment
- Pneumothorax Essentials for Australian Physiotherapy Council APC Exam. Academically
- Australia. https://academically.com/blogs/pneumothorax-essentials-for-australian-physiotherapy-council-apc-exam/
- Pneumothorax (Collapsed lung). (2025, February 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15304-collapsed-lung-pneumothorax