Introduction
Craniosacral therapy (CST) is a complementary and different medicine that explores gentle touch to detect rhythmic movements in the bones of the head and produce a healing effect. Because of its methods, some have referred to CST as quack medicine and pseudoscience.
Medical studies have not discovered convincing proof that cranial osteopathy (CST) provides any health benefits. Attempting to reconstruct the bones of the skull is dangerous, especially in infants and young children. The fundamental presumptions of CST are false, and clinicians diagnose patients in ways that contradict and are mutually incompatible.
Effectiveness and safety
There is no extra essential training program, no professional organization to manage the treatment, and it is not supervised.
According to Ernst, this is an indication that “CST leaders have less control over taxpayers”. The fundamental presumptions of CST are false, and clinicians diagnose patients in ways that contradict and are mutually incompatible.
CST experts say that they are effective in treating many diseases, including cancer treatment and drugs. Doctors strongly recommend the use of CST in young patients. As per records of the American Cancer Society, children under the age of two are not eligible to receive CST. Doctors have expressed concern about CST’s direct bad effects on infants and toddlers.
There is no such proof that CST is effective for people with autism, and might be turning out harmful. As of 2018, there are two deaths related to the manipulation of the CST landmass. In small studies, CST may increase symptoms in people who have experienced headaches. Moreover, choosing CST as a treatment for serious illnesses can be dangerous. As a result, the American Cancer Society encourages patients with cancer or various major illnesses to talk to their doctor before starting manual therapy.
As per the records American Cancer Society, while craniosacral therapy (CST) may relieve stress or tension symptoms, as well presently inadequate scientific evidence to support claims that CST is useful for the treatment of carcinoma or other diseases. Mirroring criticisms have been levied for cranial osteopathy; a 1990 paper stated that none of the claims made by the practitioners examined had any scientific foundation.
There is a dearth of data supporting CST, and no physiologically viable mechanism has been established. Without thorough, thoughtfully planned randomized controlled trials, It is pseudoscience, and quackery is what it practices. Tests reveal that CST practitioners are unable to recognize the claimed differences in the patient’s findings. A craniosacral practice is not demonstrated scientifically.
Regulation
According to Edzard Ernst, a pamphlet was released in 2005 by Prince Charles’s organization in the United Kingdom named CST as one of the numerous well-liked complementary treatments but acknowledged the therapy was unmanaged and lacked both professional organization oversight and a well-defined training program.
History
In the 1930s, William Garner Sutherland pioneered cranial osteopathy, which proceeded CST. While examining a disarticulated skull, Sutherland observed that the cranial sutures of the temporal bones where they meet the parietal bones were “beveled, resembling fish gills, suggesting they could function in a respiratory mechanism.”
From 1975 to 1983, independent reviews by Ernest W. indicated that the research findings did not support the validity or effectiveness of the skull bone theory.
A research team was formed to explore the claimed pulse and to further investigate Sutherland’s theory regarding cranial bone movement. However, independent assessments of this research concluded that the findings did not validate the existence or effectiveness of the proposed movement of cranial bones.
Overall, independent evaluations of this study determined that the results did not substantiate the concept of skull bone movement.
How is craniosacral treatment administered?
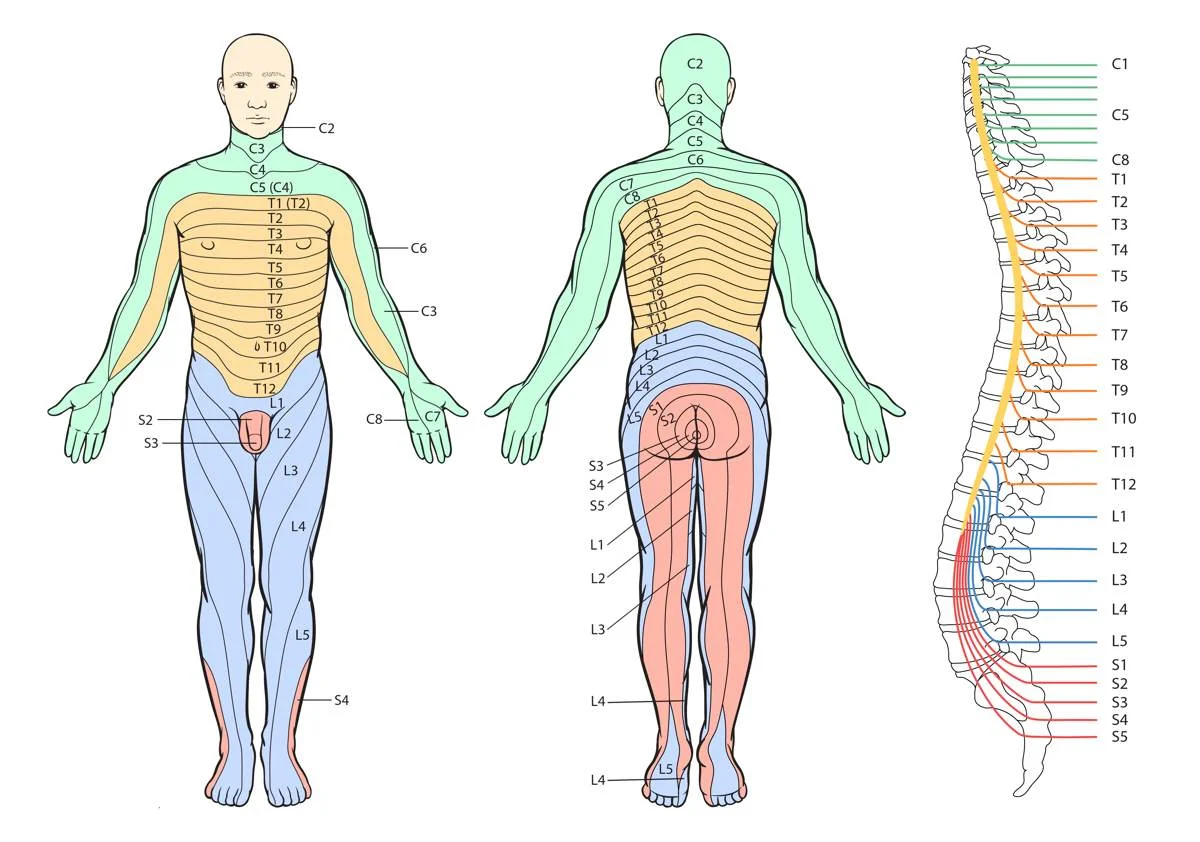
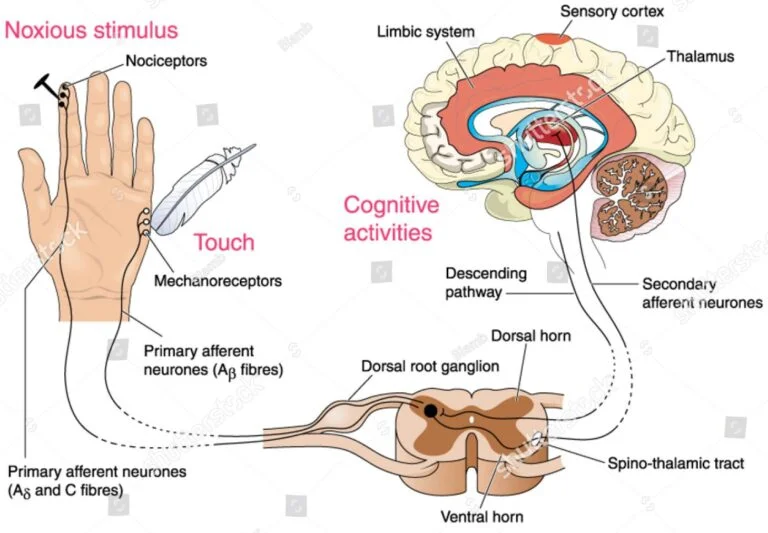
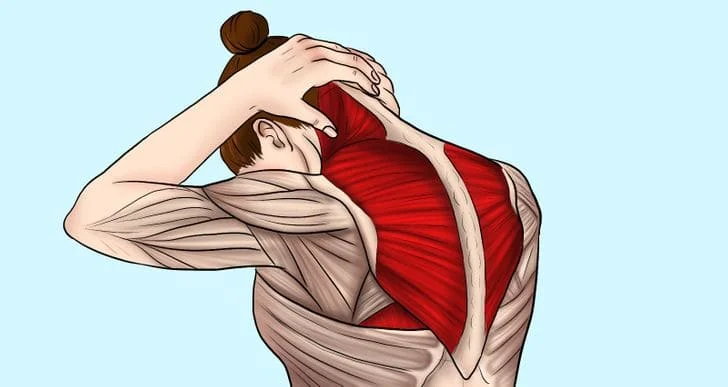
The goal of CST is to assist relieve tension in your body’s connective tissue by gently placing your hands on certain areas. We call this “fascia” (pronounced “fash-ee-uh”). The Latin word for band is facia. Your body is made up of casings that house your blood vessels, brain, spinal cord, muscles, glands, organs, and nerves. Throughout the body, the fascia weaves a web of connective tissue.
The human body’s physiological and anatomical parts are interrelated. This implies that there may be an impact on one bodily part from another. CST aims to relieve tension (fascial This may improve the way that other interconnected bodily components operate by:
- self-discipline.
- Self-rectification.
- self-repairing.
Which are the conditions that can be managed through craniosacral therapy?
Applying craniosacral therapy to address the following disorders might assist in symptom management:
- Chronic pain.
- Complex regional pain syndrome.
- Fibromyalgia.
- Headaches like migraines.
- Neuralgia.
- Post-concussion syndrome.
- Scoliosis.
- Stroke.
- Temporomandibular joint syndrome.
Your healthcare professional should advise craniosacral therapy in addition to other forms of treatment.
Is craniosacral treatment appropriate for all patients?
Craniosacral therapy can help patients of all ages, including adults and children…
Your healthcare practitioner may decide to postpone craniosacral therapy until you are well enough to receive treatment if you have recently encountered any of the following:
- thrombi.
- a head injury.
- Brain enlargement.
- cerebral aneurysm.
- Chiari malformation.
any disease that causes a build-up, leakage, or pressure of CSF fluid.
If you meet the requirements for CST, a medical specialist will notify you.
Procedure Details
What takes place in a craniosacral therapy session?
Massage treatment and a craniosacral therapy session differ mainly in that you remain fully clothed throughout the process. The environment is often designed to enhance relaxation, featuring soft music and dim lighting.
Before the session starts, your experienced therapist will have a conversation with you. They will inquire about your medical history, current condition, and the goals of the session.
During the treatment, you’ll lie on a massage table, although you might sit in a chair if needed due to specific circumstances. Your therapist will continuously monitor your comfort throughout the session.
To ensure you are informed, they will explain the process before making any physical contact. If anything feels uncomfortable, don’t hesitate to let your therapist know.
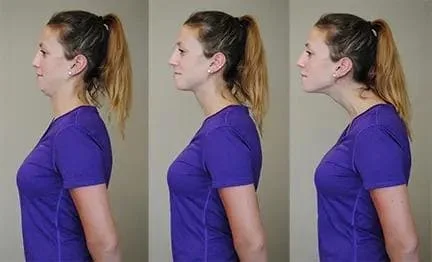
Your therapist will gently apply pressure to areas such as your head, neck, back, and around the spine that are causing discomfort.
Advantages and applications
Craniosacral therapy (CST) is believed to relieve tension in the head, neck, and back muscles, potentially reducing discomfort and stress for both the body and mind. It may also assist in easing restrictions in the head, neck, and nerves, thereby enhancing cranial mobility.
Craniofacial sacral therapy can be beneficial for individuals of all ages and may be incorporated into treatment for various conditions, including:
- headaches and migraines
- irritable bowel syndrome (IBS) with constipation
- insomnia and erratic sleep patterns
- scoliosis
- sinus infections
- neck ache
- fibromyalgia
- babies with persistent ear infections or colic
- recuperation from TMJ trauma, including whiplash damage
- mood disorders such as sadness and anxiety
- challenging pregnancies
Despite a plethora of anecdotal evidence demonstrating the efficacy of CST, further research is necessary to draw this conclusion. While some studies indicate that it may primarily benefit infants, toddlers, and children, there is evidence showing that it can also help reduce tension and stress in others.
Nevertheless, more study indicates that CST could be helpful in treating some diseases, or at the very least, a helpful part of a therapy plan. According to a 2012 research, it helped those with severe migraines feel less uncomfortable. According to different research, CST helped fibromyalgia sufferers feel better about their pain and anxiety.
Risks and side effects
When receiving cranial sacral therapy from a qualified professional, the most typical side effect is some degree of soreness after the procedure. Most of the time this is just temporary and passes within a day or two.
There are certain persons who should not use CST. Among them are those who have: severe bleeding disorders and aneurysms that have been identified as a history of recent traumatic head traumas, such as skull fractures or cranial haemorrhage.
Sessions of craniosacral treatment might run anywhere from thirty to sixty minutes. Keeping up with your goals is necessary for more than one session.
Can you treat yourself with craniosacral therapy?
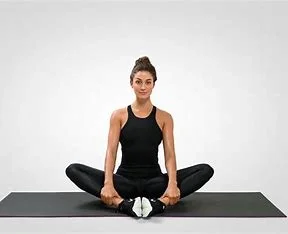
By mastering self-massage techniques for your head and neck, you can encourage relaxation at home between sessions with a licensed professional. This approach should only be applied by trained specialists who have received proper craniosacral therapy education.
Who performs craniosacral therapy?
The following healthcare providers and therapists practice craniosacral therapy:
- A physician assistant.
- A physician with osteopathic training (DO).
- An occupational or physical therapist.
- A certified massage practitioner.
Benefits
What possible advantages can craniosacral treatment offer?
- easing of pain.
- unwinding.
- enhanced emotional health.
- reduction of stress.
Is craniosacral treatment effective?
Research indicates that many people report feeling improvements after receiving craniosacral therapy. However, results can vary as each individual’s situation and motivations for seeking treatment are unique. Ongoing studies aim to further understand the effectiveness of craniosacral therapy for various medical conditions.
How risky is craniosacral therapy?
Craniosacral therapy is a gentle, non-invasive approach to healthcare, with potential side effects that may include feelings of:
- lightheaded.
- Weary.
- dizzy.
- little discomfort.
Recovery and Outlook
How long before the effects of my craniosacral therapy become apparent?
Some people experience immediate relief from their symptoms after craniosacral therapy, while for others, it may take several days for their bodies to adjust to the changes caused by the treatment. Depending on your treatment objectives, it might require multiple sessions over several weeks or months to notice improvements.
When to Make a Doctor’s Appointment
When ought I to give my healthcare provider an awareness?
Reach out to your healthcare provider after a craniosacral therapy session if you experience significant pain, discomfort, or new or worsening symptoms. Consult your healthcare practitioner for guidance if anything doesn’t feel quite right with your body.
How well does craniosacral treatment work?
There have been very few studies investigating the use of CST in disease treatment. This indicates that further study is required to confirm the complementary or alternative therapy’s efficacy.
Studies bolstering CST
Most of the CST research is rather old. A 2010 research looked into how CST affected fibromyalgia sufferers. Ninety-two individuals with the disease received CST or a placebo for a duration of twenty weeks. The outcomes demonstrated that medium-term pain improved for individuals who had CST.
A further 2011 study on CST and fibromyalgia indicates that the treatment may lessen anxiety and enhance the quality of life for persons who have the illness.
A Brief 2016 Investigation According to a reliable source, CST may assist patients with neck discomfort to operate better, live better, and experience less severe pain. More research is yet required because these studies are smaller and older.
Studies that cast doubt on CST
Overall, studies that reviewed and discussed earlier research have concluded that the claims made for CST are not sufficiently supported by the available data. They argue that there are flaws in the research’s effectiveness. Again, though, most of these assessments are more recent. An analysis from 2011 examined eight CST-related research.
A 2012 study concluded with six randomized controlled trials. The analysis demonstrated that there was probably bias in five of the six trials and that there was insufficient evidence from the sixth experiment to validate the effectiveness of CST.
Conceptual basis
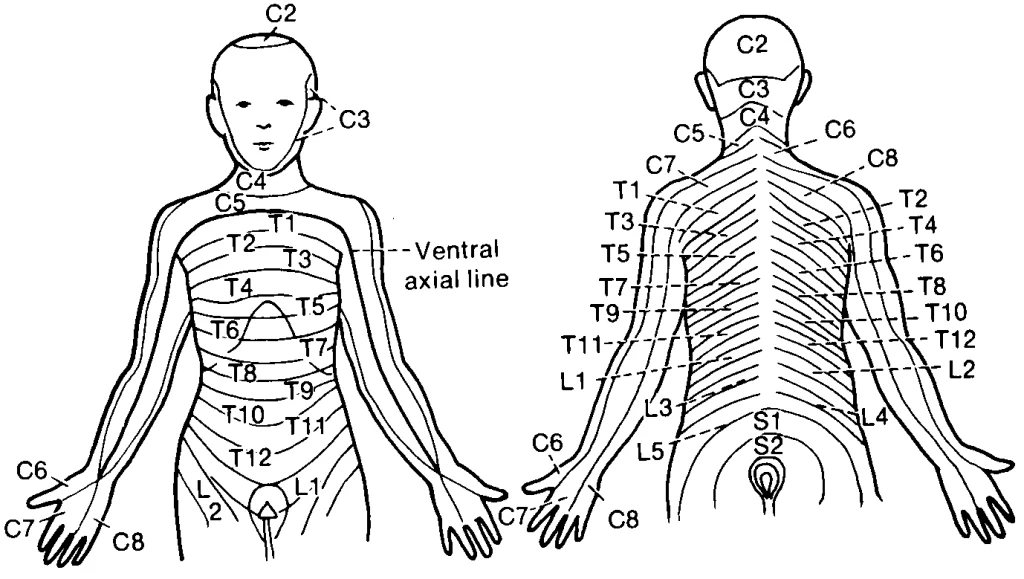
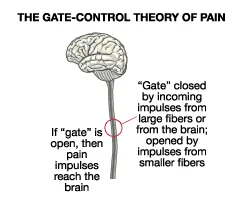
Practitioners of cranial osteopathy and CST assert that the small, regular movements of the cranial bones are affected by either cerebrospinal fluid pressure or arterial pressure. Fundamental to CST is the notion that the cranial bones move in a rhythmic fashion that is perceptible to the hand and that these motions may be modulated by certain pressures to yield therapeutic outcomes. However, there is no evidence to support the claim that these procedures can really realign the bones in a person’s skull.
The main concept of cranial osteopathy is attached to our procession of the structure and function of the human spine, brain, and skull.
CST practitioners, similar to those in many other forms of alternative medicine, believe that physical manipulation can help alleviate energy or fluid blockages, which they consider to be the root cause of all illnesses. They believe they are able to recognize and modify the regular movement of the bones in the skull.
The patient’s body is gently palpated by the therapist, who also pays close attention to the motions that are expressed. The feeling a practitioner gets when they are attuned to a patient is called entrainment.
The two disciplines are essentially the same, according to contemporary cranial osteopaths, however, cranial osteopathy has “been taught to non-osteopaths under the name CranialSacral therapy.”
How may it enhance well-being and health?
Some conditions, such as migraine headaches, chronic pain, chronic fatigue syndrome, PTSD, trauma of any type, post-surgical recovery, TMJ, and others, are treated using craniosacral therapy in addition to other therapies.
When administered by a qualified professional in a caring and courteous manner, craniosacral treatment has no negative effects. It might encourage clients to adopt a more direct and personal perspective on their well-being or a sense of “being more at peace with oneself.”
Additionally, it could encourage an organic transition to self-acceptance, a stronger inclination towards loving relationships, and a feeling of aliveness.
The cerebrospinal wave: what is it?
There is considerable discussion and speculation in the literature on craniosacral therapy regarding the characteristics of the cranial-rhythmic impulse, often referred to as the cerebrospinal wave.
Where the pulse comes from (the literature does not address this). Should the skull’s bones shift (cranial sutures move; craniosacral therapists disagree; classical anatomists frequently think that the cranial sutures fuse in maturity), etc. Whether or not there is a regular, detectable pulse (there have been several unsuccessful efforts to measure the craniosacral pulse’s cycle rate per minute).
Whether or whether the practitioner’s presence influences the pulse (this issue is crucial to the debate between integrative and allopathic philosophies; we think it is foolish to think we have no power over what we perceive, touch, or observe).
Where can I locate a professional?
Craniosacral treatment
Obtaining references is crucial when selecting a practitioner, but in the end, you have to figure out who “feels right to you.”
Online directories for craniosacral therapists in the United States and overseas include the Directory of Registered Craniosacral Therapy Practitioners from The Craniosacral Therapy Association of North America and Upledger’s International Association of Healthcare Practitioners.
In order to get insurance overage, providers usually need to hold a license in a certain specialty (such as physical therapy, chiropractic care, or massage treatment).
Summary
Several systematic evaluations have shown that there is a dearth of high-quality research on CST. Though there is little chance of damage, some people may benefit from CST, especially in terms of stress and anxiety reduction. If CST encourages people to see their health and well-being more optimistically, then they could benefit from it.
CST should never be used in place of medical care or other tried-and-true patient therapies by practitioners.
FAQs
What is the purpose of craniosacral therapy?
CST facilitates headache and neck pain alleviation. This therapy may help get rid of discomfort and side effects that come with cancer treatment.
Is craniosacral treatment authentic or fraudulent?
It also proceeded to CST as pseudoscience and quack medicine because of the practices. It is predicated on essential false beliefs regarding the structure and function of the human skull, and it’s marketed as a panacea for many various medical ailments.
What is the CranioSacral treatment success rate?
As for the CST group, over 78% reported minimally significant improvements in pain intensity at week 20, and 48% even reported significant therapeutic benefits.
Which three forms of craniosacral treatment exist?
William Sutherland’s “Aha” moment in 1948 broadened his understanding of cranial osteopathy, a discipline he founded that ultimately gave rise to the Upledger, Biodynamic, and Visionary bodies of CranioSacral Therapy.
For whom is craniosacral treatment inappropriate?
Individuals who suffer from any of the following medical conditions shouldn’t receive craniosacral therapy: thrombi. other traumatic brain injuries, such as concussions. Brain enlargement.
References
- Craniosacral Therapy. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/17677-craniosacral-therapy
- Craniosacral therapy: Does it work? https://www.medicalnewstoday.com/articles/318490
- Cranial Sacral Therapy. Healthline. https://www.healthline.com/health/cranial-sacral-therapy
- Wikipedia contributors. Craniosacral therapy. Wikipedia. https://en.wikipedia.org/wiki/Craniosacral_therapy