Neurotmesis:
Neurotmesis is a type of severe peripheral nerve injury that results from nerve transection. Neurotmesis involves cutting off the entire nerve, affecting the endoneurium, perineurium, and epineurium. The myelin sheath, connective tissues, and axon are ruptured as a result of neurotmesis.
When a peripheral nerve injury is severe enough to cause neurotmesis, the affected person as well as the medical community will be greatly impacted. A total severance of the nerve characterizes this illness, causing damage to the nerve fibers as well as the connective tissue structures that support and shield them.
In this article, we include neurotmesis’s definition, causes, symptoms, diagnostic techniques, available treatments, and overall effects on patients’ lives to gain an understanding of the condition.
What is Neurotmesis?
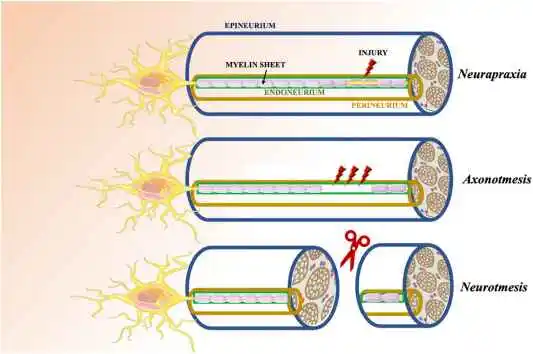
The most severe type of peripheral nerve injury is called neurotmesis, according to the Seddon classification system, which divides nerve injuries into three categories: axonotmesis, neurapraxia, and neurotmesis.
- Neurapraxia: The mildest type, in which there is no structural damage but a brief loss of function.
- Axonotmesis: When one axon is damaged but the surrounding connective tissues are unharmed.
- Neurotmesis: This is characterized by total disruption of the surrounding connective tissues, such as the endoneurium, perineurium, and epineurium, as well as the nerve fibers themselves.
Because the supporting structures are destroyed in addition to the nerve being cut in neurotmesis, spontaneous regeneration, and healing are extremely difficult. Even with surgical intervention, recovery from this type of injury can be slow and incomplete. Surgical intervention is frequently necessary to restore function.
Anatomy
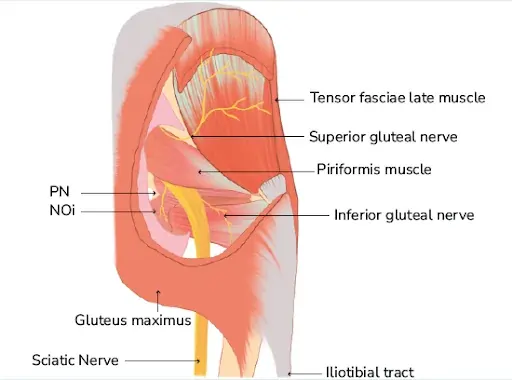
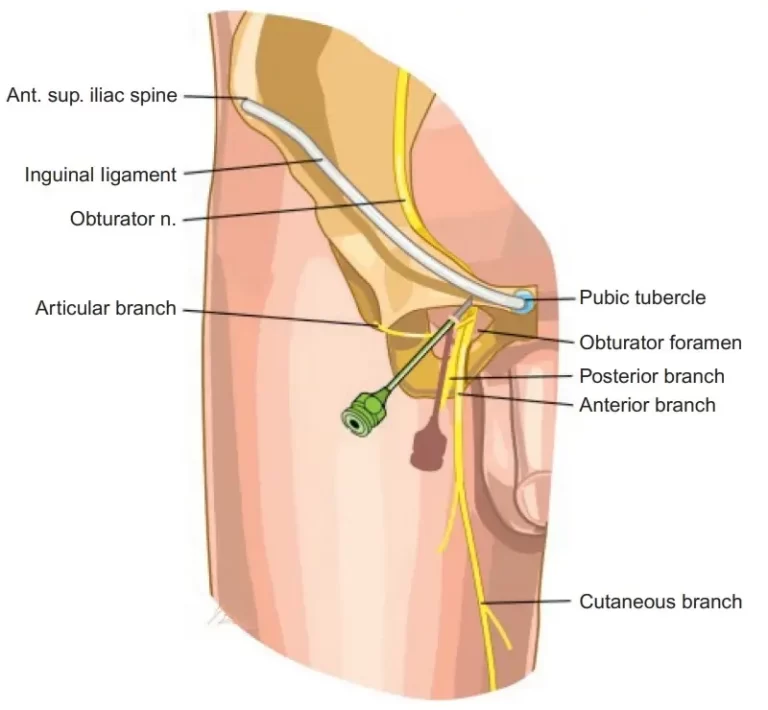
- The disorder known as neurotmesis, which affects the peripheral nervous system and usually affects the upper limbs (arms), represents 73.5% of all cases of peripheral nerve injury. The most typically damaged nerve in these situations was the ulnar nerve.
- The anatomy of peripheral nerves is such that an endoneurium surrounds the axons, followed most frequently by a myelinated sheath. That is surrounded by a perineurium, of which the outermost layer is known as the epineurium.
- “Local vascular trauma causes hemorrhage and edema (swelling), which results in a strong inflammatory response that causes scarring of the injured segment,” states the statement following an accident. Because of the severity of the injury, total loss of function occurs most of the time.
What are the causes of the Neurotmesis?
There are numerous traumatic events and medical problems that might cause neurotmesis:
- Trauma: This category includes injuries from accidents, surgery, or violence such as serious cuts, crushing injuries, or strain injuries. A severe impact trauma or a deep knife wound, for instance, could harm the nerve.
- Surgical Complications: Nerves may unintentionally be severed or cut during specific surgeries, such as those affecting the extremities.
- Tumors: If a tumor invades or compresses a nerve, causing its destruction, neurotmesis may also result.
- Infections and Inflammatory Conditions: Severe infections or autoimmune disorders causing damage to nerves may in rare instances cause neurotmesis.
What are the symptoms of the Neurotmesis?
Depending on which nerve is impacted, neurotmesis symptoms might vary, but they typically consist of:
- Loss of Sensation: Total or partial loss of sensation in the nerve’s supplied area. This could appear as a total loss of sensory input or as numbness.
- Motor Dysfunction: If the damaged nerve regulates the action of muscles, the affected muscles may become paralyzed or fragile. For example, damage to an arm motor neuron may result in paralysis of the hand or fingers.
- Pain: In the region where the injured nerve serves, patients may feel excruciating pain, which is frequently described as scorching or shooting.
- Autonomic Symptoms: Perspiration, blood flow, or other involuntary processes may be problematic in the affected location if the damaged nerve regulates autonomic activities.
What is the diagnosis for Neurotmesis?
Clinical assessment of symptoms, physical examination, and other diagnostic testing are used to identify neurotmesis. Several muscle strength tests as well as sensory examinations, which involve sensing vibration, light touch, pinprick, and other sensations, are frequently administered to patients.
- Clinical Examination: Sensory and motor impairments can be evaluated with a comprehensive physical examination. The doctor will look for indications of sensory loss, muscle weakness, and nerve damage.
- Electromyography (EMG): This examination monitors electrical activity in the muscles and can be used to determine the extent of nerve damage.
- Nerve Conduction Studies: This test is used to verify the existence of neurotmesis by measuring the strength and speed of electrical signals that pass through the nerve.
- Imaging studies: To help with surgical intervention planning, an MRI or ultrasound can be utilized to visualize the injured nerve and the surrounding tissues.
What are the treatments for the Neurotmesis?
Neurotmesis treatment usually involves a mixed approach that combines non-surgical and surgical techniques:
Pain Management:
- Medications, nerve blocks, and other pain reduction techniques are frequently used in the management of chronic pain. Neuropathic medications, such as anticonvulsants, tricyclic antidepressants, and serotonin reuptake inhibitors, are frequently used as the first line of treatment for pain in patients. Opioids, tramadol, and non-steroidal anti-inflammatory medicines (NSAIDs) make up the second class of medications used to manage pain.
Splinting:
- Static or dynamic splinting is another method used to assist in nerve repair and reduce discomfort. It can protect the wounded area and enhance function.
Surgery:
- Surgery is sometimes a possibility, but there is still extremely little chance that the damaged nerve will ever function normally again. Joining healthy nerves with diseased nerves is the aim of surgery. External neurolysis, end-to-end repair, nerve grafting, and nerve transfer from another part of the body are the most often used surgical methods.
Physical Therapy:
- To optimize healing following surgery, physical therapy is necessary. The goal of therapy is to keep the damaged limb’s muscles strong, joints mobile, and functional use of the affected limb.
Occupational therapy
- Occupational therapy teaches people how to carry out daily tasks with the function that remains after a permanent change in function.
Psychological Support:
- It can be difficult to deal with the aftereffects of a severe nerve injury, so counseling or psychological support may be helpful.
Physical Therapy for the Neurotmesis
As soon as surgery is completed, physical therapy should be started to maximize healing and avoid problems.
- Modalities: Methods for controlling pain and inflammation, such as ultrasound, heat, and cold.
- Electrical Stimulation: Electrical currents are used to activate muscles and enhance performance.
- Splinting: Using braces or splints to support the injured limb and prevent abnormalities.
- Range of motion exercises: Mild motions to avoid contractures and stiffness in the joints.
- Strengthening Exercises: Specific exercises to restore muscle mass in the injured area.
Which complications are present in Neurotmesis?
Many complications can arise from neurotmesis, a severe form of peripheral nerve injury requiring total nerve severance. A patient’s quality of life and ability to function may be severely affected by these problems.
- Neuropathic Pain: Individuals who have neurotmesis may have persistent, paralyzing neuropathic forms of nerve pain.
- Failed Regeneration: The nerve may not effectively regenerate after surgery, leading to a permanent loss of function.
- Muscle Atrophy: In the absence of nerve innervation, the injured nerve’s governed muscles may atrophy from lack of use.
- Contractures: Atrophied muscles can shorten and stiffen, resulting in joint movement limitations known as contractures.
- Ulcers: Sensation can be compromised by nerve injury, making it challenging to identify and stop skin injuries, which can result in ulcers.
- Psychological Problems: Neurotmesis-related pain and function loss can cause psychological problems, such as anxiety and sadness.
Prognosis
The degree and location of the lesion, the success of the surgical repair, and the timing of intervention are only a few of the many factors that influence the prognosis for neurotmesis. In general, healing can be sluggish and can take several months or even years.
Complete recovery may not always be achievable, and some degree of lasting damage may persist even with the best care. The current focus of research is on improving surgical methods and developing new strategies for nerve regeneration.
Summary
Neurotmesis is a severe and challenging form of peripheral nerve injury that has complex aftereffects for the affected person. Improving patient outcomes requires an understanding of the type of injury, suitable diagnostic methods, and comprehensive treatment plans. For people suffering from the severe effects of neurotmesis, there is hope for improved recovery prospects and more potent treatments as research progresses.
FAQs
What does neurotmesis mean?
A peripheral nerve that has been completely severed is called neurotmesis. Peripheral nerve injury severity can be divided into three categories: neurapraxia, axonotmesis, and neurotmesis. Complete sensory and motor impairments to the skin and muscles innervated by the damaged nerve result from neurotmesis.
Is there a cure for neurotmesis?
The complete recovery is restricted by degenerative changes that impact the target muscles and end organs, as well as by disordered axonal regeneration at the anastomosis site. When healing does happen, it usually starts close by and moves farther away.
How is neurotmesis treated surgically?
External neurolysis, end-to-end repair, nerve grafting, and nerve transfer from another part of the body are among the most often used surgical methods.
References
- Quintá, H. R., & Barrantes, F. J. (2019b). Axolemmal membrane damage and repair: from neuronal development to axonal trauma and restoration. Current Topics in Membranes, 169–185. https://doi.org/10.1016/bs.ctm.2019.07.007
- Neurotmesis. (2022, July 4). Wikipedia. https://en.wikipedia.org/wiki/Neurotmesis
- Neurotmesis. (2024, January 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/32644534/
- Knowledge and Sources on Neurotmesis – Taylor & Francis, n.d. https://taylorandfrancis.com/knowledge/medicine-and-healthcare/neurology/neurotmesis/