Neck Pain at the Base of the Skull
Introduction:
Neck pain at the base of the skull, often referred to as suboccipital pain, is a common issue that can result from poor posture, muscle tension, stress, or underlying conditions like cervical spondylosis or occipital neuralgia. This type of pain may radiate to the upper neck, shoulders, or even cause tension headaches.
Finding the source of pain at the base of your skull, which is where your head and neck meet behind your ears, can be challenging. Realizing what’s causing the pain can help you figure out how to address it.
The dull, throbbing, acute, or stabbing pain near the base of your skull can interfere with your life while you try to determine what’s causing it. Although the majority of the reasons for pain in this area are not serious, they can occasionally be signs of an unexpected or chronic (long-lasting) medical issue that needs to be treated.
Symptoms of Base Skull Neck Pain:
Since it can cause excruciating headaches, many patients wish to treat neck pain near the base of their skull right away. If you suffer from any of the following symptoms or if your neck pain began following a violent incident, you should visit a doctor immediately:
- Migraine.
- Numbness or tingling.
- Fever.
- Pain that gets worse with time.
- Radiating Pain.
A physical therapist can help you identify potential causes of neck pain and provide efficient therapy, regardless of how severe or mild your pain is.
Causes of Neck Pain at the Base of the Skull:
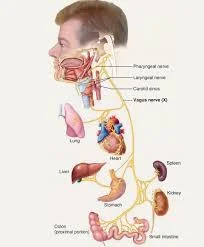
A complex network of vital nerves is involved in this location. It also consists of the muscles, ligaments, tendons, and joints that allow you to easily tilt and rotate your head. Due to its proximity to the brain, the base of the skull is very significant. As a result, pain in this region needs to be treated carefully. You might be experiencing symptoms of the following conditions:
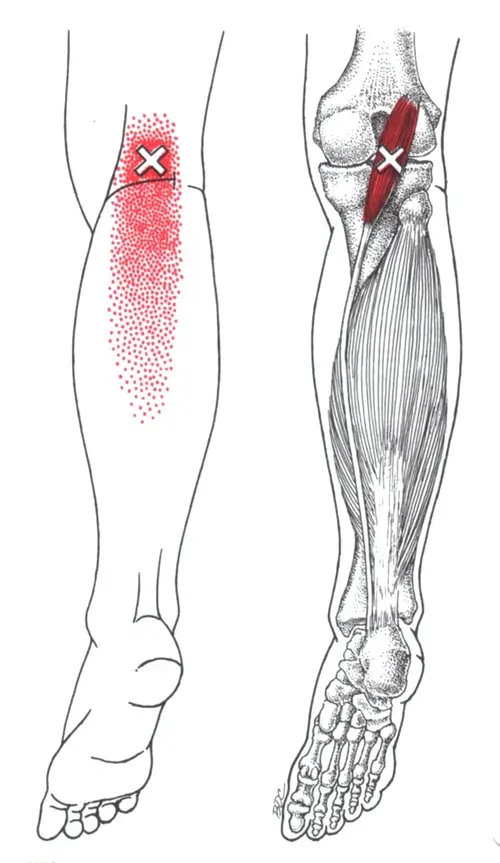
Suboccipital muscle inflammation:
In addition to causing stress and pain in these muscles, poor posture, like hunching over a desk, can irritate the base of the skull. In order to relieve stress and lessen pain, physical therapy can help you with posture correction and massage your tense muscles.
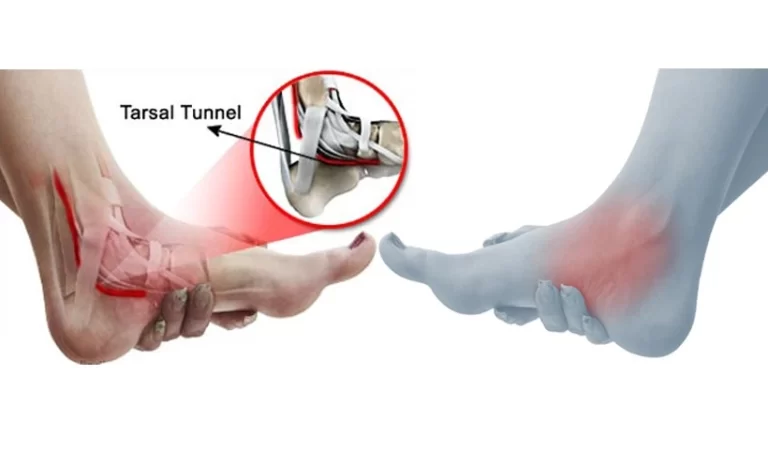
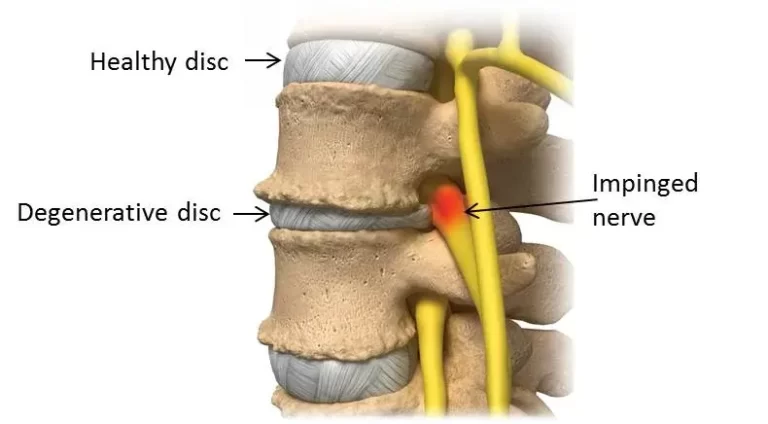
Herniated cervical disc:
Your neck’s discs are called cervical discs. Their inner layer is softer, and their outer layer is more resilient. A herniated disc can occur when a portion of the inner layer slides out of the outer layer.
You are more likely to experience pain near the base of your skull if the disc is higher. Cervicogenic headaches are frequently caused by herniated cervical discs. Additionally, you can have a reduction in the range of motion in your upper arms, shoulders, or neck. You may feel numbness in your fingers and the rest of your arm.
Occipital neuralgia:
When one of your occipital nerves is pinched, inflamed, or injured, you may experience occipital neuralgia. Where your neck meets your skull, occipital neuralgia typically causes throbbing, acute, or electric-like pain. Physical therapy might provide comfort by releasing the tissue that is compressing your nerve.
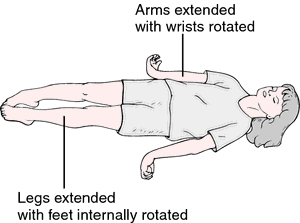
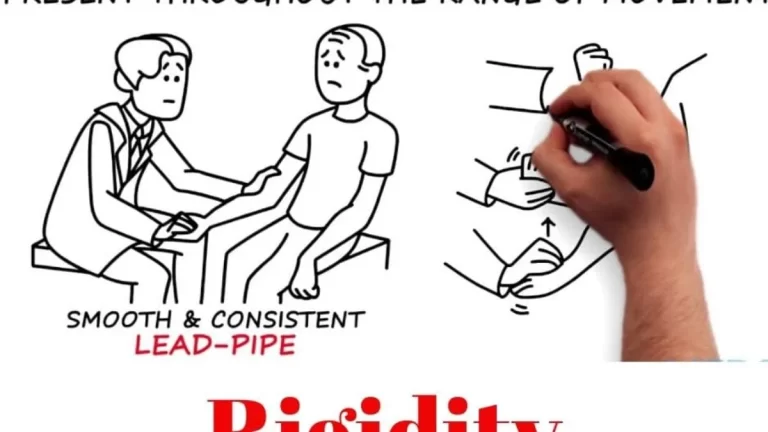
Rheumatoid or Osteoarthritis:
Rheumatoid or Osteoarthritis, often known as rheumatoid arthritis, is a very prevalent condition in adults that can arise from the gradual degradation of cartilage between joints. This deterioration may result in both dull and severe pain as the joint’s bones scrape against one another when moving. Curiously, the C1 and C2 vertebrae are frequently affected by arthritis.
Tension Headache:
Often called a tension headache, tension-type headaches are the most prevalent type of headache condition. The pain may be slight or moderate, and headaches may occur infrequently or frequently.
These headaches could resemble:
- A sharp ache on your forehead, scalp, or behind your ears
- A dull pain throughout your head
- More intense pain across your shoulders, in your temples, or at the back of your neck
Stress, disease, exhaustion, sleep deprivation, dental issues, and muscular tension are just a few of the numerous factors that can cause headaches. This kind of headache is more common in women, although it will happen to most people at some point in their lives.
Migraine:
Some migraineurs may experience headache pain at the back of their skull. Neck pain is also directly related to migraine. Some claim that neck pain can cause a migraine attack, while others report that it is one of the symptoms they encounter before or after a migraine attack.
Muscle Strain or Injury:
The suboccipital muscles, which stretch to support the back of your head and are situated at the top of your neck, are particularly susceptible to tension. Cervicogenic headaches, which frequently begin as neck pain before spreading to the head, might be caused by overly tight suboccipital muscles. The base of the skull may also hurt due to strain and inflammation caused by frequent muscle spasms or trauma to the suboccipital muscles, such as whiplash following an automobile accident.
Diagnosis of Base Skull Neck Pain:
They will probably perform a quick physical examination of the injured area. A neurological examination, which includes assessing your reflexes, balance, stability, and reaction to heat and cold stimuli, may also be performed by your healthcare professional.
That might be all your doctor needs to diagnose some conditions, such as tension-type headaches or muscular strains.
If there are other reasons, a healthcare professional will either run additional tests or send you to a specialist for further assessment.
Diagnosing Arthritis:
Magnetic resonance imaging (MRI) and X-rays are two imaging procedures that can be used to diagnose arthritis. Both are capable of taking pictures of the interior of the body.
By revealing to your doctor any indications of joint degeneration or inflammation, both tests can aid in the diagnosis of arthritis. You might be referred to a rheumatologist, a specialist who treats arthritis, depending on the findings.
Diagnosing Occipital Neuralgia:
Your physician can suggest an MRI or computed tomography (CT) scan if a physical examination is insufficient to diagnose occipital neuralgia. CT scans are comparable to X-rays, but because they capture images from several perspectives, they are more detailed.
Occipital neuralgia is frequently treated by neurologists or medical professionals who specialize in the nervous system.
Diagnosing a Herniated Cervical Disc:
Basic blood tests may be performed by a healthcare professional to check for indications of inflammatory diseases. They can then select from a number of imaging tests to check for any physical changes to the discs or vertebrae if these test results are negative. An MRI to determine whether soft tissue or nerves within the discs are damaged, a CT scan to check for bone loss or herniation, and an X-ray to assess spinal alignment and health are some examples of these tests.
Unless your symptoms have persisted for more than six weeks or have not improved with simple treatment, these imaging tests are typically not performed. A herniated cervical disc can be treated with the assistance of an orthopedist or orthopedic surgeon.
Diagnosing Vertebral Artery Dissection:
The preferred method for diagnosing VAD is an MRI. However, computed tomography angiography (CTA) is the next best thing because most people cannot easily obtain MRIs for a rapid diagnosis.
Dye is injected into the blood vessels by the test administrator. Any indication of blood vessel disease, including a tear, is shown on the imaging by the dye. Blood vessels in the head and neck are treated using CTA. Your provider will probably order a CT scan if CTA is not accessible.
Treatment of Neck Pain at the Base of the Skull:
The origin of this kind of pain determines how it should be treated, however, most problems near the base of the skull can be resolved with a mix of home remedies and prescription medications.
Possible treatment possibilities include:
- Over-the-counter medication: Nonsteroidal anti-inflammatory medicines (NSAIDs) like Advil (ibuprofen) or OTC pain relievers like Tylenol (acetaminophen) might help lessen pain from headaches, strained muscles, arthritis, and a ruptured cervical disc.
- Lifestyle changes: Getting enough sleep, maintaining proper posture, stretching gently, getting frequent moderate exercise, and reducing stress and worry may all help.
- Prescription drugs: Prescription drugs can help ease the pain of occipital neuralgia, arthritis, or a herniated disc.
- Physical therapy: For occipital neuralgia, arthritis, and a herniated cervical disc, a physical therapist can help you strengthen your muscles and expand your range of motion.
- Surgery: To treat pain from occipital neuralgia, arthritis, and a herniated cervical disc, numerous surgical procedures are carried out. However, in the majority of cases, your doctor might wait to consider surgery until you’ve tried less intrusive methods.
Physical Therapy Treatment:
Pain medication and cold packs can help manage your neck pain during the day, but they may not address the underlying reason. Upper neck pain and other musculoskeletal conditions are well-treated by physical therapists. To help you recover from neck pain at the base of your skull as soon as possible, they have access to a variety of methods, tools, and instructional materials.
- Spinal manipulation.
- Active Release Techniques.
- Therapeutic exercises.
- Graston Technique.
- Functional rehabilitation.
Prevention:
Maintaining good posture while doing daily tasks and embracing healthy lifestyle choices are key to preventing base of skull neck pain. Frequent neck, shoulder, and upper back strengthening and stretching exercises can enhance muscular balance and lessen suboccipital strain. Ergonomic workstation modifications are essential for reducing neck strain, particularly for people who use computers or phones for extended periods.
Further lowering the risk can be achieved by utilizing supportive pillows when sleeping, avoiding extended static positions, and taking frequent rests. Deep breathing, yoga, meditation, and other stress-reduction methods may also assist in avoiding the muscle tension that causes base of the skull pain.
Prognosis:
With the right care and therapy, the prognosis for base skull (suboccipital) neck pain is usually good. Conservative therapies, including physical therapy, posture correction, ergonomic improvements, and focused exercises to strengthen the muscles in the neck and upper back, provide significant relief for the majority of people.
The underlying reason, such as a cervicogenic headache, bad posture, or muscle strain, might affect recovery duration, but symptoms usually go away in a few weeks to a few months. To avoid recurrence and preserve long-term neck health in chronic instances, a multidisciplinary approach incorporating pain management and lifestyle changes may be required.
Complications:
If base skull (suboccipital) neck pain is not addressed or is not adequately managed, complications may develop. Chronic pain can impair everyday activities and quality of life by causing muscle stiffness, headaches, and decreased neck mobility.
Persistent tension in the suboccipital area may occasionally be a factor in referred shoulder and arm pain, vision abnormalities, or cervicogenic dizziness.
Rarely, neurological abnormalities necessitating more extensive medical intervention may arise if the pain is caused by underlying structural problems or nerve compression.
Conclusion:
In conclusion, base skull neck pain is a common yet frequently treatable condition that is usually caused by tense muscles, bad posture, or underlying cervical problems. Most people can have substantial relief and avoid recurrence with early diagnosis and adequate treatment, including physical therapy, posture correction, and lifestyle changes.
To prevent any consequences and guarantee a higher quality of life through greater neck function and less pain, prompt intervention is necessary.
FAQs
Why does it hurt to touch the base of the skull?
Occipital neuralgia can develop on its own, as a result of a pinched nerve root in the neck (from arthritis, for instance), or as a result of previous scalp or skull injuries or surgeries. Nerves can occasionally become trapped by “tight” muscles at the back of the skull.
Is base of the skull soreness typical?
The dull, throbbing, acute, or stabbing pain near the base of your skull can interfere with your life while you try to determine what’s causing it. Although the majority of the reasons of pain in this area are not serious, they can occasionally be signs of an unexpected or chronic (long-lasting) medical issue that needs to be treated.
How can someone with neck pain sleep?
Aim for neutral spine posture while sleeping on your side or back with adequate pillow support if you have neck pain. To fill the space between your neck and the pillow, think about using a cervical pillow or a rolled-up towel. Sleeping on your stomach can worse neck strain, so avoid doing so.
Does nighttime make neck pain worse?
“You should try to optimize every aspect that is within your control, including sleep, if you already have neck pain.” People frequently forget that their actions throughout the day can cause them to toss and turn at night, which can result in pain and poor alignment.
When under stress, may the base of the skull hurt?
When the muscles in the neck and scalp tense or contract, tension headaches result. The contractions of the muscles may be a reaction to anxiety, stress, despair, or a brain injury. Although they can happen at any age, adults and older teens are the most likely to experience them.
How can I sleep without getting neck pain?
Prioritize side sleeping with appropriate neck alignment or back sleeping with pillow support to get a good night’s sleep and prevent neck pain. A rolled-up towel or a cushion that takes into account the natural curvature of your neck can be used to fill the gap between it and the mattress.
Which side of the neck pains the most?
On the other hand, severe and ongoing left-sided neck pain, or pain that has no known explanation and does not subside with rest or at-home remedies, suggests a significant issue that requires medical attention.
Which vitamin is the source of neck pain?
Neck pain is linked to deficits in vitamin D and B12. A lack of vitamin D can make muscles weak and painful, which can make neck pain worse. A lack of vitamin B12 can have an impact on the nervous system, which may result in neurological symptoms like neck pain and paresthesia, or tingling feelings.
Does the base of the skull hurt while under stress?
When the muscles in the neck and scalp tense or contract, tension headaches result. The contractions of the muscles may be a reaction to anxiety, stress, despair, or a brain injury. Although they can happen at any age, adults and older teens are the most likely to experience them.
References
- Back of neck Pain Base of skull area: All you need to know. (2025, March 27). Centeno-Schultz Clinic. https://centenoschultz.com/symptom/neck-pain-at-the-base-of-skull/
- Grogan, J. (2025, March 14). Neck pain at the base of the skull: 4 Causes | SOL. Alliance Physical Therapy Partners. https://solpt.com/why-am-i-feeling-neck-pain-at-the-base-of-my-skull/
- Bradley, S. (2025, January 17). What to know and do about pain at the base of your skull. Health. https://www.health.com/pain-at-base-of-skull-8747542