Modified Ashworth Scale
Introduction
The Modified Ashworth Scale (MAS) is a clinical tool used to assess spasticity in individuals, particularly those with neurological conditions such as stroke, multiple sclerosis, and cerebral palsy.
Severe spasticity has a profound effect on a patient’s life, influencing everything from everyday activities to mental health and even financial security. However, spasticity can help individuals with weak limbs particularly those in the lower extremities by making it easier for them to move around and walk. For these reasons, the examination of spasticity is necessary so that specialists can identify if their treatment procedures are effective.
A five-point numerical rating system, ranging from 0 (no resistance) to 4 (limb rigidity in either flexion or extension), was used in the original Ashworth scale. The modified Ashworth scale (MAS), which has been modified, has been used to quantify spasticity in clinical settings and scientific studies. The goal of the modified Ashworth scale is to assign a muscle spasticity rating. The following is the scale:
Modified Ashworth Scale:
- 0: The tone of the muscles has not increased.
- 1: a slight increase in muscle tone during flexion or extension of the affected part or parts, followed by a slight resistance or catch and release when the affected part or parts achieve their range of motion.
- 1+: The remaining range of motion has very little resistance (less than half) after a minor increase in muscle tone that gives the sensation of a catch.
- 2: There is a noticeable increase in muscular tone over a significant percentage of the range of motion, even though the affected part or parts can still be moved with ease.
- 3: much higher muscular tone and difficult passive motion
- 4: The affected part(s) are rigid while extending or flexing
Intended Population
The Modified Ashworth Scale (MAS) has been applied to the following populations: individuals with cerebral palsy, multiple sclerosis, stroke, spinal cord injury, traumatic brain injury, hypertonia in children, and abnormalities of the central nervous system.
Method of Use
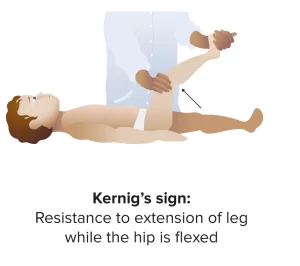
The patient’s limb is initially extended from a position of maximal flexion to maximal extension (the point at which the first gentle resistance is met) in order to conduct the test.
Reliability
To guarantee the Modified Ashworth Scale’s accuracy and consistency when used by several assessors and on many testing occasions, a thorough investigation of its reliability has been conducted. The major research that looked into the MAS’s intra- and inter-rater reliability are listed below.
Interrater/Interrater Reliability
- While interrater reliability measures the consistency of assessments made by the same assessor in time, interrater reliability describes the level of agreement between many assessors. The Modified Ashworth Scale must be validated in clinical and research contexts using these dependability indicators.
- In everyday practice, the Modified Ashworth Scale technique is a typical instrument for measuring spasticity and may be completed quickly and easily.
Validity
A number of techniques, including content, construct, and criteria validity, can be used to evaluate validity.
Criterion Validity
- The relationship between the MAS scores and other recognized markers of spasticity, including EMG values, is examined for criterion validity.
- However, because of a significant methodological flaw, it is not possible to conclude with certainty that the modified Ashworth score is a reliable and accurate measure of spasticity. Although it was said that grading spasticity (by passively moving the limb) took between 0.25 and 0.33 s, several of the EMG characteristics that were produced had weak reference points to this time frame.
Construct Validity
- To increase the scale’s sensitivity, some research added a 1+ category, which falls between 1 and 2, to the original scale. Since then, both scales have been applied to clinical and scientific settings as spasticity measurements. After assessing the resistance to passive movement about a joint, an assessor assigns a clinical rating on the Ashworth Scales for spasticity. With the exception of grade “4”, both grades indicate the resistance experienced when a joint is moved through its entire range of motion.
Content Validity
- The MAS’s content validity assesses if it has all the elements required to measure spasticity.
Clinical Significance
Many patients experience spasticity after an initiating event. According to recent scientific studies, 20 to 30 percent of stroke survivors experience spasticity. Seven years following a stroke, physicians looked at the prevalence of increased muscle tone, including contracture and normal spasticity. The MAS can be used in clinical practice to measure the effectiveness of both pharmacological and rehabilitation therapy for these individuals because of its simplicity in terms of clinical use.
These days, the Modified Ashworth Scale (MAS) is the gold standard for clinical assessment of spasticity in the extremities. It is the most extensively used tool to gauge how well pharmaceutical and rehabilitative therapy work in treating and managing spasticity in individuals with spinal cord injury.
FAQs
What is the spasticity tone scale?
The Ashworth scale (AS) is the most widely used and well-known scale (Table 3). This scale ranges from 0 (normal) to 4 (severe spasticity) for muscular tone. This scale is simple to use, but the results vary depending on who is doing the evaluation.
In stroke patients, is the Modified Ashworth Scale a reliable tool?
For the hip flexors, the interrater reliability of the MAS was moderate, whereas the other four muscle groups that were first examined following a stroke showed comparable results in terms of reliability. Our study’s findings support the notion that, when applied by a single rater, the MAS is a trustworthy metric.
How is the Ashworth scale performed?
Until the first gentle resistance is detected, the rater should stretch the client’s limb from a maximal flexion to a maximal extension position.
References
- Harb, A., & Kishner, S. (2023, May 1). Modified Ashworth Scale. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK554572/
- Modified Ashworth Scale – Strokengine. (n.d.). https://strokengine.ca/en/assessments/modified-ashworth-scale/