Lung Cancer
Introduction
Lung cancer is a type of cancer that starts in the lungs, typically in the cells lining the airways. Lung carcinoma, another name for lung cancer, is a type of malignant tumor that starts in the lung. Genetic damage to the DNA of airway cells, frequently caused by cigarette smoking or harmful chemical inhalation, is the cause of lung cancer.
A tumor can arise as a result of damaged airway cells having the capacity to proliferate unregulated. Tumors spread throughout the lung and impair lung function if left untreated. Lung tumors eventually spread to other areas of the body through metastasis.
In the United States, lung cancer ranks third in terms of incidence. It is caused by dangerous cells in your lungs proliferating out of control. Surgery, immunotherapy, chemotherapy, radiation, and targeted medications are among the available treatments. It is advised to get screened if you are at high risk. Lung cancer deaths have significantly decreased in recent years due to advancements in treatment.
Normal lung structure and function
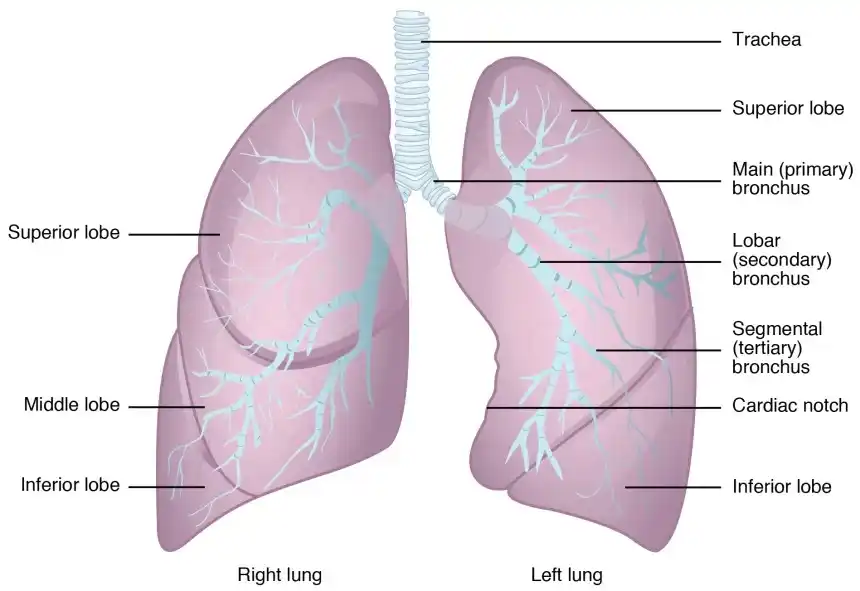
The two sponge-like organs in your chest that make up your lungs are divided into portions known as lobes. You have three lobes in your right lung. There are two lobes in your left lung. The left lung is smaller because the heart takes up more space on the left side of the body.
Air enters your lungs through the trachea (windpipe) after passing through your mouth or nose when you inhale. After splitting into tubes known as bronchi, the trachea enters the lungs and further splits into smaller bronchi. These split into bronchioles, which are smaller branches. Small air sacs called alveoli are located at the end of bronchioles.
When you exhale (breathe out), the alveoli take carbon dioxide out of your blood and absorb oxygen from the air you breathe in. The primary roles of your lungs are to take in oxygen and expel carbon dioxide.
The lungs are surrounded by a thin lining layer known as the pleura. As your lungs expand and collapse while breathing, the pleura shields them and facilitates their movement back and forth against the chest wall.
The diaphragm, a narrow, dome-shaped muscle, divides the chest from the belly under the lungs. The diaphragm rises and falls during breathing, pushing air into and out of the lungs.
Lung Cancer: What Is It?
Lung cancer is caused by cell division in the lungs. The cell’s normal function is to divide and produce additional copies of itself. Your organs’ ability to operate is eventually compromised by tumors, which are lumps of tissue created when damaged cells divide rapidly.
The term lung cancer refers to tumors that originate in the lungs, typically in the small air sacs (alveoli) or airways (bronchi or bronchioles). The term cancer that’s metastatic to your lungs may be used by your healthcare practitioner to describe cancers that originate elsewhere and spread to your lungs.
Pathogenesis
Mutations that enable tumor cells to proliferate indefinitely, promote blood vessel growth, avoid apoptosis (programmed cell death), produce pro-growth signaling molecules, disregard anti-growth signaling molecules, and ultimately spread into surrounding tissue or metastasize throughout the body are the cause of lung cancer, as they are for all cancers.
Although different alterations can give distinct malignancies these capabilities, oncogenes and tumor suppressors are typically activated and inactivated by cancer-contributing mutations. Certain mutations, known as driver mutations, are disproportionately involved in the development of tumors and are especially prevalent in adenocarcinomas.
The receptor tyrosine kinases EGFR, BRAF, MET, KRAS, and PIK3CA are usually where these arise.
Tyrosine kinases ALK, ROS1, NTRK, and RET are overexpressed in some adenocarcinomas due to chromosomal rearrangements.
Usually, a single driver mutation is present in a particular tumor. On the other hand, SCLCs frequently feature mutations that have made the tumor suppressors p53 and RB inactive rather than these driving alterations.
Early in the course of all lung malignancies, a group of tumor suppressor genes on chromosome 3’s short arm are frequently lost.
Types of lung Cancer:
Although there are many types of lung cancer, the two primary types that are commonly referred to as lung cancer are small cell lung cancer and non-small cell lung cancer.
- Non-small cell lung cancer
- Small cell lung cancer
Non-small cell lung cancer (NSCLC)
The most common kind of lung cancer is non-small cell lung cancer (NSCLC). More than 80% of cases of lung cancer are caused by it. Squamous cell cancer and adenocarcinoma are common varieties. Two less prevalent forms of NSCLC are sarcomatoid carcinoma and adenosquamous carcinoma.
Small cell lung cancer (SCLC)
Compared to NSCLC, small cell lung cancer (SCLC) grows more quickly and is more difficult to cure. It frequently manifests as a tiny lung tumor that has already metastasized to other body areas. Small cell carcinoma (also known as oat cell carcinoma) and mixed small cell carcinoma are two distinct forms of SCLC.
Other lung cancer type
Sarcomas (cancer of the soft tissues or bones), lymphomas (cancer of the lymph nodes), and pleural mesothelioma (cancer of the lining of the lungs) are among the other cancers that can begin in or near the lungs. These are treated differently and are usually not called lung cancer.
What are the stages of lung cancer?
The size of the original tumor, its depth and extent in the surrounding tissue, and whether it has migrated to lymph nodes or other organs are the main factors used to stage cancer. Guidelines for staging vary depending on the type of cancer.
Lung cancer staging
Multiple size and spread options for each stage can fit into that group. For example, a Stage III cancer may have a smaller primary tumor than a Stage II cancer, but it may be at a more advanced stage due to other causes. Lung cancer is generally staged as follows:
- Stage 0 (in-situ): The lung or bronchus’s upper lining is cancerous. It hasn’t extended outside of the lung or to other lung regions.
- Stage I: The lung has not been affected by the cancer.
- Stage II: The cancer is larger than Stage I, contains many tumors in the same lung lobe, or has progressed to the lymph nodes of the lung.
- Stage III: The cancer is bigger than Stage II, has spread to neighboring structures or lymph nodes, or has many tumors in various lung lobes.
- Stage IV: The cancer has progressed to the heart, other lung, the fluid surrounding the lung, or distant organs.
Although stages I through IV are currently used by clinicians for small cell lung cancer, the terms limited or extensive stage may also be used. Whether the region can be treated with a single radiation field is the basis for this.
One lung is all that is affected by limited stage SCLC, which can also occasionally be found in the lymph nodes in the middle of the chest or above the collar bone on the same side.
One lung is completely covered in extensive stage SCLC, or it has progressed to the other lung, the lymph nodes on the opposite side of the lung, or other body areas.
Metastatic lung cancer
Metastatic lung cancer is a type of cancer that starts in one lung and spreads to the other lung or other organs. Compared to lung cancer that has not moved beyond its original site, metastatic lung cancer is more difficult to treat.
Prevalence
Over 200,000 new cases of lung cancer are reported by health systems annually, making it the third most frequent disease in the United States.
Signs and symptoms of lung cancer
Most lung cancer symptoms resemble those of other, less dangerous conditions. Many people do not feel symptoms until the disease has advanced, although some do in its early stages. Only one or a few of these symptoms may be present in persons who do:
- A persistent cough or one that worsens with time.
- Breathing difficulties or dyspnea.
- Discomfort or chest pain.
- Wheezing.
- Blood in the cough (hemoptysis).
- A hoarse voice.
- Loss of appetite.
- Sudden loss of weight.
- Unexplained tiredness or fatigue.
- Shoulder pain.
- Facial, neck, arm, or upper chest swelling (superior vena cava syndrome).
- Horner’s syndrome is characterized by a small pupil and drooping eyelid in one eye, along with little or no perspiration on that side of the face.
First signs of lung cancer?
Although it can also be an indication of less serious illnesses, a cough or pneumonia that persists after treatment may occasionally be an early indicator of lung cancer. The most typical symptoms of lung cancer are hoarseness, chest pain, shortness of breath, coughing that doesn’t go away, or unexplained weight loss.
Some of these symptoms may appear early (in stages I or II), depending on where the cancer begins in the lungs, but they frequently do not appear until the cancer has spread to later stages. If you’re at a higher risk, it’s crucial to get examined for lung cancer.
How long is it possible to have lung cancer without being aware of it?
It might take years for cancer to develop in your body before you become aware of it. In its early stages, lung cancer frequently shows no symptoms.
Causes
Cells that continue to divide when they shouldn’t are the source of lung cancer. Even though cell division is a natural process, every cell has an internal switch that stops it from dividing into new cells (senescence) or, if necessary, causes it to die off (apoptosis). When a cell undergoes too many divisions or modifications (mutations), the off switch is activated.
Normal cells in your body that have undergone mutations that cause them to lose their off switch are called cancer cells. Unchecked, cells continue to proliferate and disrupt your normal cells. Cancer cells have the ability to spread damage throughout your body by entering your lymph nodes or bloodstream.
Although the exact origin of these alterations that cause cancer in some people but not in others is unknown, smoking tobacco products is one of the factors that can increase your chance of lung cancer-causing cell damage.
Risk factors
Although there are numerous variables that can raise your risk of developing lung cancer, the largest risk factor is smoking tobacco products of any type, such as cigarettes, cigars, or pipes. According to experts, smoking is responsible for 80% of lung cancer deaths.
Additional risk factors consist of:
- Being in close proximity to tobacco smoke.
- Being exposed to dangerous substances such as coal products, silica, diesel exhaust, uranium, asbestos, radon, air pollution, and others.
- Having received radiation therapy to the chest in the past (for example, for lymphoma or breast cancer).
- Lung cancer running in the family.
Is lung cancer a result of vaping?
Certain compounds, including some known carcinogens, may be inhaled when vaping, which is the practice of using a device to inhale a mist of nicotine and flavoring. Although the whole range of long-term repercussions of vaping is unknown, it may harm the lungs.
Is it possible to develop lung cancer without smoking?
Up to 20% of individuals with lung cancer have never smoked, despite the fact that smoking is the main risk factor for the disease. For this reason, it’s critical to discuss any troubling symptoms with your healthcare physician.
Testing and Diagnosis
How is a diagnosis of lung cancer made?
Lung cancer diagnosis may involve several steps. A medical professional will often listen to your symptoms, ask about your medical history, and perform a physical examination (such as listening to your heart and lungs) during your initial visit.
A chest X-ray and blood tests may be the first things your doctor does because the symptoms of lung cancer might be confused with those of many other, more prevalent conditions.
A biopsy and other imaging tests, such as a CT scan, are typically the next stages in the diagnosis process if your doctor believes you may have lung cancer.
Additional tests include examinations of malignant tissue from a biopsy to assist in establishing the best course of treatment and a PET/CT scan to check for the spread of cancer.
Does lung cancer appear on a chest X-ray?
When it comes to detecting lung tumors, especially in their early stages, CT scans are more accurate than X-rays. On an X-ray, tumors may be too small to see or may be obscured by other body parts, such as your ribs. Lung cancer cannot be diagnosed by X-rays; they can only alert your healthcare professional to any unusual activity that warrants further investigation.
What tests will be performed?
Blood tests, imaging, and fluid or tissue biopsies are among the procedures your healthcare professional may order or carry out.
Blood examinations: Although blood tests cannot identify cancer on their own, they can assist your doctor in assessing the health of your organs and other body parts.
Imaging CT scans and chest X-rays provide your doctor with pictures that may reveal lung abnormalities. PET/CT scans are typically performed to assess a troubling CT scan result or determine whether cancer has spread following a cancer diagnosis.
A biopsy: Your healthcare professional may employ several techniques to examine the contents of your chest in greater detail. Your doctor may do a biopsy, which involves taking samples of tissue or fluid.
These samples can then be examined under a microscope to check for cancer cells and identify the kind of cancer. Additionally, samples can be examined for genetic alterations (mutations) that could impact your course of treatment.
The following procedures are used to either learn more about the spread of lung cancer or to make an initial diagnosis:
- Biopsy using a needle: Your healthcare practitioner will use a needle to take tissue or fluid samples for analysis during this procedure.
- Video-assisted thoracic surgery (VATS), thoracoscopy, or bronchoscopy: Using these techniques, a healthcare professional examines several lung regions and obtains tissue samples.
- Thoracentesis: This process is used by a healthcare professional to collect a sample of the fluid surrounding your lungs for analysis.
- Endoscopic esophageal ultrasonography or endobronchial ultrasound: These techniques are used by a provider to examine and biopsy lymph nodes.
- Either mediastinotomy or mediastinoscopy: Using these techniques, a healthcare professional examines and collects samples from the mediastinum, the space between your lungs.
Molecular analyses: During a biopsy, your doctor may screen a sample of tissue for gene alterations (mutations) that can be targeted by certain medications as part of your treatment regimen. The following genes may have alterations that can be targeted in NSCLC:
- KRAS,
- EGFR,
- ALK,
- ROS1,
- BRAF,
- RET,
- ME, and
- HER2
- NTRK.
Prevention
How can lung cancer be avoided?
- The only way to avoid cancer is to lower your risk because we don’t know for sure what causes the majority of them. Here are a few strategies to lower your risk:
- Avoid smoking, or if you already smoke, stop. Within five years of stopping, your risk of lung cancer begins to decline.
- Avoid substances that can damage your lungs, such as secondhand smoke.
- Eat well and keep your weight within a healthy range. Consuming two to six and a half cups of fruits and vegetables daily may help lower your chance of developing cancer.
- If your risk of lung cancer is high, get screened.
Screening
With screening tests, you can improve your chances of detecting cancer early on. If you fulfill each of the following criteria, you are qualified for a lung cancer screening:
- You are in the 50–80 age range.
- You either smoke now or have given it up in the previous 15 years.
- The number of packs of cigarettes you smoke each day multiplied by the number of years you have smoked is 20 pack-years.
Treatment
What is the treatment for lung cancer?
The goal of lung cancer treatments is to either kill the cancer or stop its spread. Your immune system can eliminate, destroy, stop the growth of cancerous cells, or teach them to fight. Additionally, several therapies are utilized to reduce pain and lessen symptoms. How you are treated will depend on several factors, including the kind, location, and severity of your lung cancer.
Which drugs or therapies are utilized to treat lung cancer?
Surgery, radiofrequency ablation, radiation therapy, chemotherapy, targeted medication therapy, and immunotherapy are among the treatments for lung cancer.
- Surgery may be an option for SCLC with only one tumor and non-small cell lung cancer (NSCLC) that hasn’t spread. To ensure that no cancer cells are left behind, your surgeon may remove the tumor along with a tiny portion of the surrounding healthy tissue. In certain cases, resection the removal of all or part of your lung is necessary to increase the likelihood that the cancer won’t return.
Radiofrequency ablation
Sometimes, radiofrequency ablation (RFA) is used to treat NSCLC tumors close to the outer borders of your lungs. RFA heats and kills cancer cells using high-energy radio waves.
Radiation treatment
High-energy beams are used in radiation therapy to destroy cancer cells. It can be taken on its own or to increase the efficacy of surgery. Additionally, radiation therapy can be used to reduce discomfort, decrease tumors, and provide palliative care. Both SCLC and NSCLC use it.
Chemotherapy
Chemotherapy is frequently a mix of several drugs intended to prevent the growth of cancer cells. It can be used before, following, or in conjunction with immunotherapy or other forms of medication. Chemotherapy for lung cancer is usually given intravenously.
Targeted drug therapy
Lung cancer cells in certain NSCLC patients contain certain alterations (mutations) that promote the growth of the malignancy. In an effort to slow down or eliminate cancer cells, certain medications target these alterations.
Additional medications known as angiogenesis inhibitors can prevent the tumor from generating new blood vessels, which are necessary for the growth of cancer cells.
Immunotherapy
Normally, our bodies identify and eliminate damaged or dangerous cells. Cancer may cover itself from the immune system in order to avoid being eliminated. Immunotherapy helps your body fight cancer by exposing cancer cells to your immune system.
Symptom-relieving therapies (palliative care)
Breathing difficulties and other symptoms decrease by certain lung cancer treatments. These include procedures to remove fluid from the area surrounding your lungs and prevent it from returning, as well as treatments to shrink or remove tumors that are obstructing your airways.
Physical therapy
Physical therapy interventions differ according to the timing of treatment and the stage of the illness path.
- Exercise intervention prescription and delivery should be an essential component of physical therapy management for lung cancer.
- Exercise and physical activity are essential for addressing the three primary aspects of the cancer continuity: morbidity, death, and prevention.
- Similar to the recommendations for the general adult population, the American Cancer Society advises persons with cancer to perform two sessions of resistance training and at least 150 minutes of moderate-intensity aerobic exercise each week.
Exercise
- Resistance training and aerobic exercise improve lung functionality by clearing airways and reducing airflow obstruction; as a result, the enhanced functional skills boost energy levels and sputum production.
- Programs for pulmonary rehabilitation are specifically designed for people who have recently undergone lung surgery, for example, to maximize their respiratory function and, consequently, their quality of life (QOL) and engagement in daily activities.
- In addition to maximizing function, physical activity, psychological state, and health-related quality of life over the long term, exercise after surgery or therapy attempts to restore physical status (addressing potential treatment-related loss of muscle strength and functional ability).
- Increasing one’s ability to exercise (fitness)
- Enhancing muscular strength and lowering cancer symptoms, such as fatigue and dyspnea
- Lowering the rate of depression
- Lowering tension
- Lowering cancer-related distress and enhancing life quality
How much should I exercise?
The guidelines for cancer patients include 30 minutes of aerobic exercise at least five days a week, such as jogging, swimming, brisk walking, or riding a stationary bike.
Strengthening exercises are also advised two to three days a week to maintain muscle strength, and if you have experienced falls or have poor balance, you should also do balance exercises.
There are limitations on the kind of exercise and quantity of heavy lifting and strengthening exercises you can perform in the early post-lung surgery period.
Treatment side effects
The type of treatment for lung cancer determines the side effects. For your particular treatment, your physician can advise you about potential side effects and potential consequences.
- Nausea and vomiting,
- Diarrhea,
- Loss of hair,
- Exhaustion,
- Mouth sores,
- Weakness, tingling, or loss of sensation (neuropathy),
- Itchy rash,
- Discomfort in the joints,
- Pneumonitis, colitis, hepatitis, and other complications may cause further adverse consequences.
- Breathlessness,
- Cough,
- Pain,
- Having trouble swallowing,
- Skin that is red, dry, or irritated,
- Ache in the chest wall.
FAQs
How long can a lung cancer patient live?
Almost 65 out of 100 people (almost 65%) with stage 1 lung cancer will survive their cancer for 5 years or more after they’re diagnosed.
How can we stop the spread of lung cancer?
The goal of chemotherapy is to prevent cancer cells from proliferating in order to reduce their mass and prevent them from spreading. Patients with stage 3 or stage 4 lung cancer that has progressed to adjacent organs can use it. Depending on the results of the medical evaluation, surgery can also be necessary.
Can lung cancer be cured?
After receiving a diagnosis, roughly one in ten patients survive for at least ten years, and two out of five survive for at least a year. However, depending on how far the disease has gone at the time of diagnosis, survival rates might vary significantly.
Is it possible to survive with one lung?
If necessary, most people can survive with just one lung rather than two. Unless the other lung is injured and unable to perform these functions, one lung can frequently supply enough oxygen and expel enough carbon dioxide.
What cancer is 100% curable?
Melanoma, Hodgkin lymphoma, and cancers of the breast, prostate, testicles, cervical region, and thyroid have some of the greatest 5-year relative survival rates, despite the fact that there are no tumors that can be cured. Cancer is a condition when cells in specific body regions develop and multiply out of control.
Is it possible to treat stage 4 lung cancer?
Lung cancer frequently goes undetected until it’s at an advanced stage because symptoms don’t appear before then. If there are symptoms, they’re often similar to other health problems. Stage 4 lung cancer can’t be cured.
What is the fastest-killing cancer?
Pancreatic cancer is the most deadly kind of cancer, taking the lives of more than 80% of those who are diagnosed and having the lowest survival rate. This is partly because this kind of cancer is misdiagnosed and delayed.
Does lung cancer have a hereditary component?
Although the two main causes of lung cancer are smoking and air pollution, a number of studies have shown that hereditary factors also play a role in the development of lung cancer. Both smokers and non-smokers are more susceptible to lung cancer if there is a family history of the disease.
Reference
- What is lung cancer? | Types of lung cancer. (n.d.). American Cancer Society. https://www.cancer.org/cancer/types/lung-cancer/about/what-is.html
- Lung cancer. (2024, December 6). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/4375-lung-cancer