Lumbar Spine Normal Range Of Motion
Introduction
Maintaining normal spinal movement patterns during the developmental stage requires an adequate range of motion (ROM). The individual vertebra’s shape changes during growth and maturation, leading to changes in posture and mobility in the mature spine.
Understanding patterns of change across the adult lifespan and the proposed reasons for these changes is essential for exploring spinal mobility in children. Limited spinal mobility as a result of spinal disorders or injury requires quantifying spinal mobility, which is a crucial component of the physical therapy examination process for both adults and children.
The lumbar vertebrae achieve two significant developmental milestones between seven and 11 years of age. First, primary ossification is completed between approximately seven and nine years, making the bone less malleable in response to internal and external forces as the percentage of bone increases relative to the percentage of cartilage.
Second, the lumbar facet joints change from a relatively frontal to a sagittal plane, changing the shape from flat at birth to curved by approximately 11 years of age. This change in lumbar facet orientation plays a role in the quantity and direction of lumbar movement.
Spinal mobility involves not only the range of motion (ROM) of a joint or series of joints but also internal influences such as joint type, elasticity of muscle tissues, tendons, ligaments, and musculature length, as well as external factors such as age, gender, height, and weight.
The lumbar range is essential in children because spinal mobility during the developmental stage may be affected by diseases, disorders, and/or injuries of the neuromuscular or musculoskeletal systems.
Several techniques have been developed to assess spinal flexibility, such as visual estimation, finger-to-floor distance, sit-and-reach measurements, standard or modified Schober’s methods, subjective reports through questionnaires, and the use of devices such as flexicurves, protractors, goniometers, and inclinometers. The preference for the technique of spinal ROM evaluation in routine clinical practice is often based on its reliability, validity, simplicity, cost, level of invasiveness, and technicality.
Establishing reference norms for spinal flexibility requires assessment techniques with a high level of validity and reliability. The inclinometric technique, which is valid and reliable, has been recommended as a valuable tool in routine clinical assessment of spinal ROM. It is believed that the inclinometric technique can measure and differentiate movements of the hip from those of the lumbar spine, and it can be learned quickly within a short period.
Normative values of the spine’s range of motion (ROM) are crucial for the proper diagnosis of spinal impairments, monitoring the effect of treatment, and the patient’s recovery. Physical therapists can utilize normative values to estimate the active end-range spinal position attained in each cardinal plane motion. This estimation is essential as physical therapists do not have access to radiographs, unlike physicians, who use radiographs to measure spinal mobility. The use of normative values helps in quantifying spinal mobility and provides a feasible alternative to radiographs for physical therapists.
Early identification and management of abnormal lumbar spinal mobility are essential to prevent further deformity. Normative data and confounding factors that affect the lumbar range are valuable components in the prevention of deformities. Although normative values for adult spinal mobility have been established using various measurement devices, little information is available on normal lumbar spine mobility for children aged five to 11 years. The study’s purposes aim to establish normative values for active lumbar flexion, extension, and side bending in children aged five, seven, nine, and 11 years and identify the confounding factors that affect the lumbar range.
Overview of the three different kinds of range-of-motion exercises
- Passive range of motion is when someone else moves the lumbar spine through its available range of motion while the person receiving the exercise stays completely relaxed.
- Active-assisted range of motion is when the lumbar spine receives some help from an external force, such as a physical therapist or a person helping the patient.
- Active range of motion is when the patient performs the exercise entirely on their own, without any external force contributing to the motion.
What is a goniometer?
- A device known as a goniometer is used to measure the range of motion of the lumbar spine. It is typically made of either metal or plastic and consists of two arms. To determine the angular distance, the goniometer is placed on the head and the numbers are observed. The physical therapist usually employs a goniometer to measure the lumbar spine’s range of motion.
- If a patient is experiencing a decrease in lumbar spine range of motion, the physical therapist can use a goniometer to assess the initial range of motion at the beginning of an assessment. In subsequent sessions, the therapist employs a goniometer to ensure that the intervention is working.
- The universal goniometer is the most widely used of all the goniometer types available.
Universal Goniometer
There are two types of universal goniometers available: short-arm and long-arm goniometers. Short-arm goniometers are suitable for measuring smaller joints like the wrist, elbow, or ankle, whereas long-arm goniometers are more precise for joints with long levers such as the knee and hip joints.
Gravity Goniometer/Inclinometer
One arm of a particular goniometer is equipped with a weighted pointer that remains upright due to the effect of gravity.
Goniometers that function through software or smartphone technology have numerous advantages. These include easy accessibility, effortless measurement, and the ability to track measurements via applications. Additionally, they can be used with one hand. The accelerometers in smartphones are utilized in these goniometers to calculate the angles of knee joints.
Arthrodial Goniometer
Measuring cervical rotation, anteroposterior flexion, and lateral flexion of the cervical spine is made easy with the twin-axis electro-goniometer. Although it is more reliable than the universal goniometer, it is still challenging to apply in the clinical evaluation of a patient. It is therefore more commonly used for research purposes.
Tape Measure
The tape measure is likely the most commonly used and simplest instrument for measuring spinal motion. It has also been used for longer than any other measurement in the clinic to determine the range of motion of the lumbar spine. Overall, it is the least expensive option available for this purpose.
Methods
Testing Lx Flexion
- Radiography is the most precise technique to evaluate the motion of vertebrae. However, the utilization of extended radiography is not advisable due to the potential hazards of radiation and the expenses involved.
Other methods of measurement include:
- Fingertip to floor test (uses tape measure)
- The Schober test and a modified version of the Schober test, which involves using a tape measure, are both important tests to consider.
- Goniometer
- Tape measure
- Radiography is the most precise way to determine the movement of the vertebrae, but it is not practical to use long-term radiography because of the potential hazards of radiation exposure and the associated expenses.
An expensive handheld, circular, fluid-filled disc with a weighted gravity pendulum attached to it that is kept in the vertical direction is called an Inclinometer. It is graduated over 360 degrees by 0.5-degree intervals.
A non-invasive electro-goniometer and torsiometer were utilized to measure the range of motion (ROM) of the lumbar spine. The accuracy and reliability of the devices were verified by comparing the ROM values obtained from dynamic flexion/extension and lateral bending radiographs with those produced by the device that was activated while the radiographs were obtained.
Intraobserver reliability was established by determining the intraclass correlation coefficient for repeated measurements on the same subjects by one investigator on consecutive days. These tools were used in a clinical laboratory setting to assess the complete active ROM of the lumbar spines (flexion/extension, lateral bending, and axial rotation) of 60 asymptomatic subjects (30 women and 30 men; aged 20 to 75 years) and evaluate the functional ROM required to complete 15 simulated activities of daily living (ADLs).
Visual observation
There are significant variations in the lumbar range of motion caused by certain variables. The normal population’s motion characteristics, as shown in the table above, differ significantly from those of the LBP population. However, since these populations are diverse, there is a lot of variability within each group, which limits the clinical utility of these measurements.
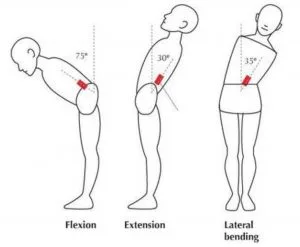
With age, there is a decline in flexion, which goes from 73 to 40 degrees. Lateral flexion (L&R), which goes from 28-14 degrees, also declines with age. Extension, which goes from 29-6 degrees, has the most significant decline at 79% with age. However, there is no decline in axial rotational, which remains constant at 7% throughout the age spectrum.
In 2005, researchers created comprehensive, gender-specific, broadly based, and age-related indices for normative lumbar ranges of motion in all planes of movement. These indices apply to individuals throughout their adult lives, from adolescence through to old age.
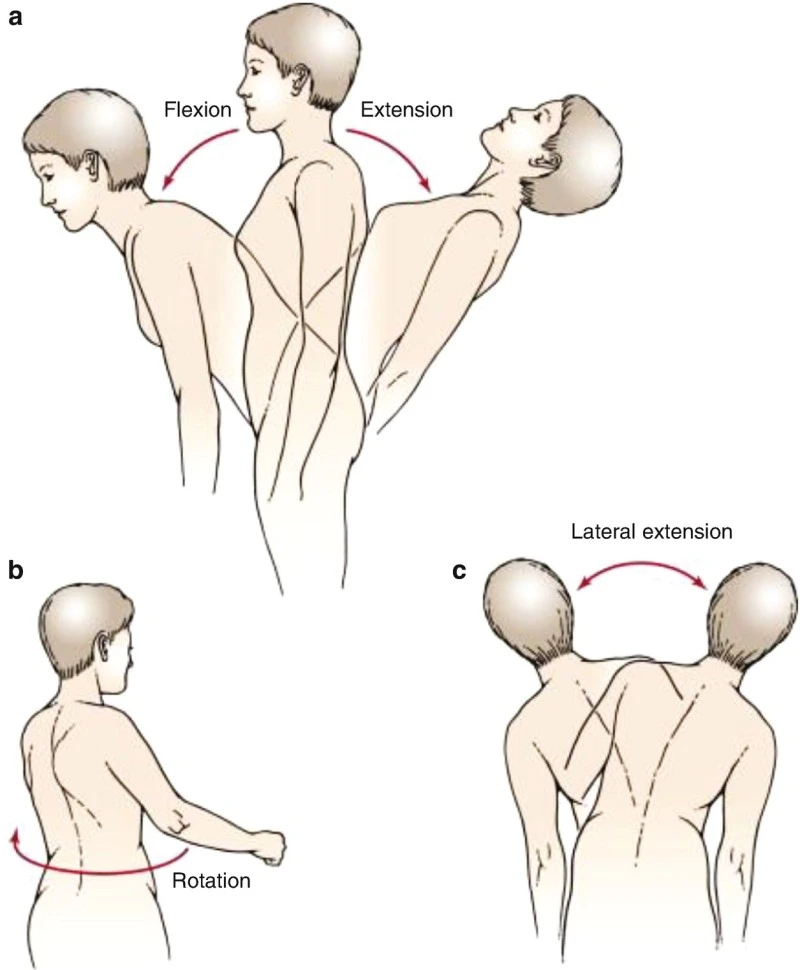
Movements of the lumbar spine
- Flexion: Bending the spine forward implies moving it towards the floor from the front side.
- Extension: Bending the spine backward refers to moving toward the floor from the back.
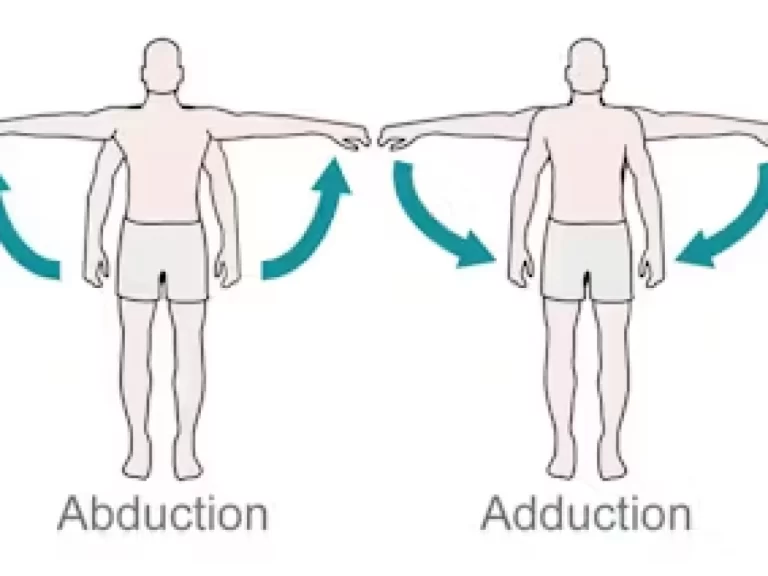
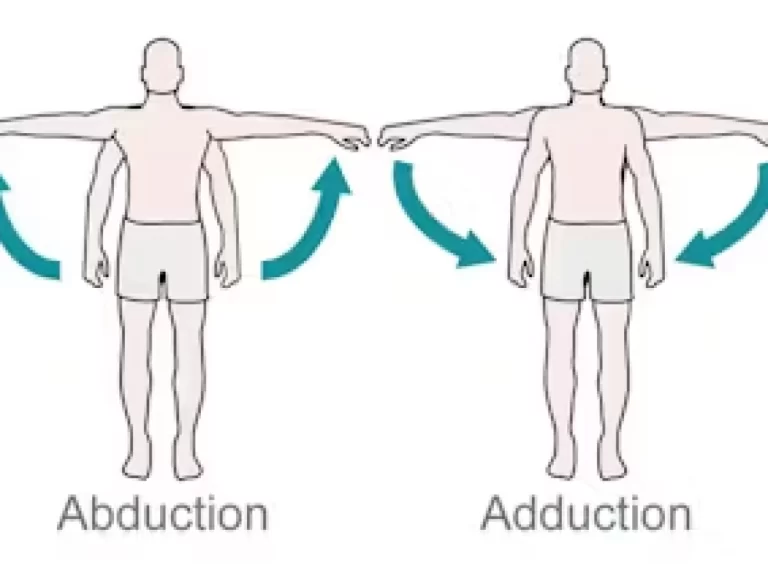
- Lateral flexion: The lateral movement of the spine occurs on both the left and right sides.
- Rotation: Rotating the spine to the right and left sides.
ADLs
- Housework
- During daily activities, people tend to use only a small portion of their full active range of motion (ROM). A study conducted in 2010 found that the ROM and percentage of full active lumbar spinal ROM used during 15 ADLs ranged from 3 to 49 degrees.
- When lifting an object from the ground, squatting requires 42 degrees of sagittal motion, while bending at the waist necessitates 48 degrees of sagittal motion. Ascending and descending stairs require a comparable amount of total motion in all three motion planes, but all of them are less than the above figures.
- Personal hygiene ADLs, such as hand washing, washing hair, shaving, and make-up application, require a similar amount of motion as walking and going up and down stairs when grouped.
Statistical Analysis
The statistical analysis of the data obtained in the study was performed using IBM SPSS Statistics vn. 23 software (Statistical Package for Social Sciences). The mean and standard deviation values were used to express numerical data, while frequency and percentages were used to express categorical data.
The Kolmogorov-Smirnov test was utilized to assess the data’s normal distribution. The mean range of motion (ROM) measurements were compared between genders using the Mann-Whitney U test. The study required a minimum of 273 participants to maintain a 5% margin of error with a 90% confidence level.
Active Range of Motion
The patient should perform these standing movements under the therapist’s observation. The therapist should consider the patient’s willingness to perform the movement, assess any differences in the range of motion (ROM), and look for any compensation mechanisms. It is recommended that painful movements should be performed last. During the movements, the therapist should watch out for any limitations in movement and possible causes such as pain, spasms, stiffness, or blocking (Magee, 2006).
Flexion
Flexion: Monitor the patient’s movement range, which should be around 40-60 degrees. Be observant of any compensatory movements in the thoracic spine. The typical lumbar lordosis should level out during the procedure. Keep an eye out for sudden or discomforting movements, and take note of how far the patient can lean forward during flexion.
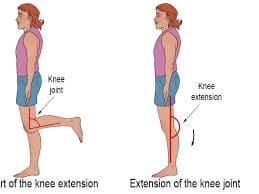
Extension
Extension: When moving within a range of 20-35 degrees, the patient should put their hands on their hips to stabilize the movement and avoid compensating with their pelvis…….
Lateral Flexion
Lateral Flexion: 15-20 degrees, the patient runs their hand down the side of the leg while attempting not to make any forward or backward movements. Make a comparison with the opposite side and record the degree of rotation that is done in addition to the flexion.
Rotation
Rotation: Performing active range of motion exercises within a temperature range of 3-18 degrees can be done either in a standing or sitting position, which helps in eliminating hip movement. There are alternative methods of performing active range of motion, such as sitting and quadruped positions. However, according to the authors, the use of the quadruped position highlights the deviation from the norm.
Quadruped Flexion-Extension
Quadruped Flexion-Extension: The individual is requested to assume the posture of a cat by positioning themselves on their hands and knees. The shoulders, wrists, hips, and knees should be at a 90-degree angle while keeping the back straight. Starting from this initial position, the individual should arch their whole spine as much as possible, without making any compensatory movements in their elbows or any other joints. After a few seconds, they should return to the starting position and then fully extend their whole spine. Once again, the initial position should be resumed after a few seconds.
Quadruped Flexion
Quadruped Flexion: Placing the patient on their elbows during the test is a variation that can be used to lower the upper body. This position results in the greatest lumbar flexion and thoracic extension.
Quadruped Extension
Quadruped Extension: When the hands of the patient are lifted, it results in the greatest lumbar extension and thoracic flexion in the upper body.
Techniques of measurement in detail
Tape Measure
A tape measure is likely the most economical device for quantifying spinal movement, and it may also be the simplest to operate. Moreover, the use of a tape measure for evaluating the range of motion (ROM) of the spine in clinical settings predates any other measurement method.
Flexion and Extension
Schober method
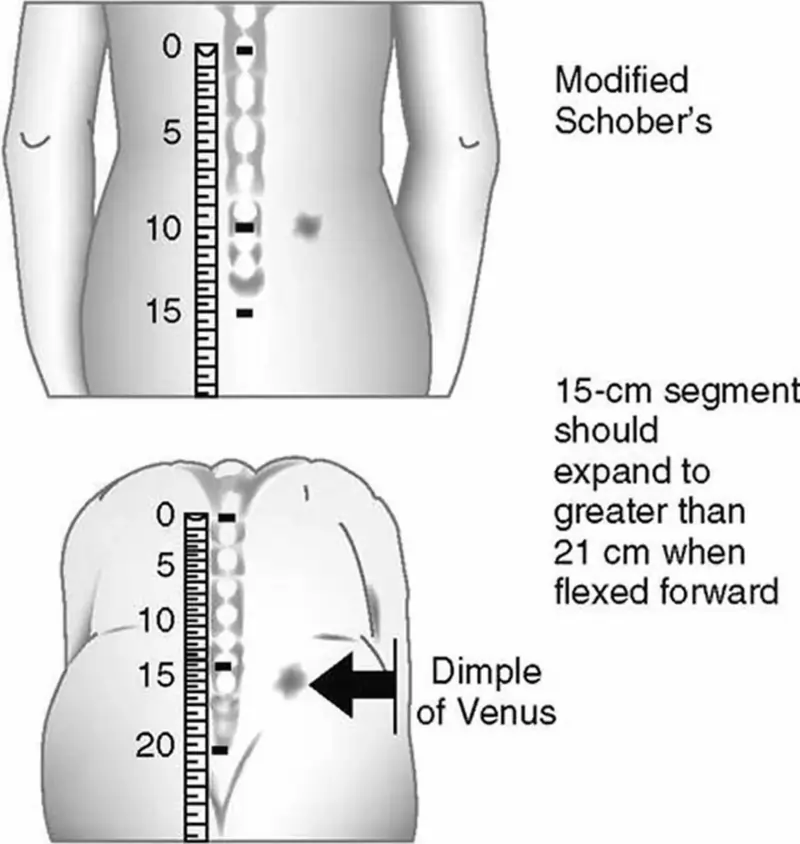
The measurement of lumbar flexion commonly involves a technique developed by Schober and later modified by Macrae and Wright. Schober first described the two-mark method in 1937, which involves marking the lumbosacral junction and a spot 10 cm higher, then measuring the increase in distance between the two marks after the subject bends forward as far as possible. This technique, known as the skin distraction method, relies on stretching or distracting the skin over the spine. Macrae and Wright modified the Schober technique by adding a third mark five centimeters below the lumbosacral junction, as they had observed that the skin above and below the lumbosacral spine was distracted during flexion, leading to measurement inaccuracies.
Van Adrichem and van der Korst later suggested that using the lumbosacral junction for measurement added difficulty, and Williams et al recommended the use of the modified-modified Schober method instead, which uses two skin landmarks instead of three, with one bisecting a line connecting the two posterior superior iliac spines and the other 15 cm higher. The baseline for measuring lumbar and thoracolumbar flexion in this chapter is the bisection of the line connecting the two PSIS, as described by Williams et al.
Moll and Wright suggested modifications of the Schober technique for the examination of lumbar extension, involving measuring the change in skin marks as the marks move closer together during the extension movement. As previously described, the baseline measurement for lumbar extension used in this chapter is the bisection of the line connecting the two PSIS, according to Williams et al.
The tape measure method for measuring lumbar flexion, lumbar extension, and thoracolumbar flexion involves aligning the tape measure with specific bony landmarks, such as the midline of the spine in line with the PSIS, spinous process of the C7 vertebra, or a baseline mark that is 15 cm higher. These landmarks are indicated by red lines and dots in the images provided.
Fingertip to floor method
Some researchers have suggested the use of the fingertip-to-floor method to quickly and consistently assess the flexion of the spine. This technique differs from the Schober method and its variations in that it does not involve measuring directly over the lumbar spine. Instead, the patient simply bends forward and the distance between the floor and the tip of the middle finger is measured using a tape measure. The fingertip-to-floor test is a combined test that measures multiple muscle movements.
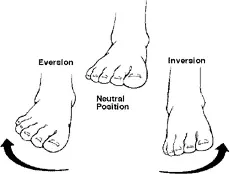
Lateral Flexion
In the literature, two methods have been proposed to use a tape measure for examining lateral flexion of the spine, but neither has gained clinical prominence. One of these methods involves marking the lateral thigh and the other involves measuring the distance from the third fingertip to the floor.
Mellin first introduced the method of marking the location on the lateral thigh that the third fingertip can touch during erect standing and after lateral flexion to measure lateral flexion. The range of lateral flexion to that side is represented by the distance between the two marks.
To measure lateral flexion using the fingertip-to-floor method, the distance from the third fingertip to the floor is measured while the patient is standing erect and then again after they laterally flex the spine. The difference in distance between erect standing and lateral flexion is considered the range of lateral flexion.
An alternative technique involves aligning the tape measure at the end range of motion of lateral flexion using the distance-to-floor method. The red dot at the level of the middle fingertip indicates the landmark for both the starting position and end range of motion of thoracolumbar lateral flexion. The difference between the skin marks on the thigh, indicated by the red dots, is measured using a tape measure.
Rotation
Frost et al2 devised a technique for gauging rotation in the thoracolumbar spine utilizing a tape measure, with the lateral tip of the ipsilateral acromion and the greater trochanter of the contralateral femur as reference points.
The starting position for measuring thoracolumbar rotation using the tape measure method can be determined by the patient holding the tape measure against the superior landmark, which is the lateral tip of the ipsilateral acromion.
The tape measure’s initial alignment is set up to measure thoracolumbar rotation while the patient is sitting.
The tape measure’s alignment at the end range of motion (ROM) of thoracolumbar rotation can also be determined using this method.
Goniometer method to measure lumbar ROM
The measurement of the range of motion (ROM) of the spine is often done using a standard goniometer, which comprises two rulers rotating on a protractor. In this chapter, techniques for measuring flexion, extension, and lateral flexion of the spine are explained. However, the rotation of the thoracolumbar spine is not generally measured using a goniometer.
The starting position for measuring lumbar flexion using the goniometer technique is indicated by a red line and dot, which represent the mid-axillary line at the level of the lowest rib and mid-axillary line, respectively. Similarly, the end range of motion (ROM) of lumbar flexion can be measured using the goniometer technique, with the same landmarks for goniometric alignment indicated by the red line and dot.
During the beginning range of lumbar flexion, the goniometer alignment is adjusted to ensure accuracy. Similarly, during the end range of lumbar flexion, the goniometer alignment is adjusted to ensure accuracy.
The starting position for measuring lumbar extension using the goniometer technique is also indicated by a red line and dot, representing the mid-axillary line at the level of the lowest rib and mid-axillary line, respectively. Similarly, the end range of motion (ROM) of lumbar extension can be measured using the goniometer technique, with the same landmarks for goniometric alignment indicated by the red line and dot.
During the beginning range of lumbar extension, the goniometer alignment is adjusted to ensure accuracy. Similarly, during the end range of lumbar extension, the goniometer alignment is adjusted to ensure accuracy.
The starting position for measuring lumbar lateral flexion using the goniometer technique is indicated by red dots, representing the spinous process of the S1 vertebra and the spinous process of the C7 vertebra. Similarly, the end range of motion (ROM) of lumbar lateral flexion can be measured using the goniometer technique, with the same landmarks for goniometric alignment indicated by the red dots.
During the beginning range of lumbar lateral flexion, the goniometer alignment is adjusted to ensure accuracy. Similarly, during the end range of lumbar lateral flexion, the goniometer alignment is adjusted to ensure accuracy.
Inclinometer
The use of inclinometers for measuring spinal mobility has been approved by the American Medical Association (AMA) in its Guides to the Evaluation of Permanent Impairment. Thus, it can be inferred that the inclinometer has gained acceptance as a feasible and potentially accurate method for measuring spine mobility.
There are different techniques for using the inclinometer to measure spinal movement. One method uses two inclinometers simultaneously to measure spinal movement (double-inclinometer method), while another uses one inclinometer to measure the same spinal movement (single-inclinometer method). Additionally, the inclinometer can be held against the subject during the examination of ROM, or it can be strapped onto and attached to the individual (Back range of motion [BROM] device). All these methods have been approved by the AMA as appropriate for measuring spinal mobility.
This chapter describes the use of the dual-inclinometer technique for measuring the movement of the lumbar and thoracic spine for flexion, extension, lateral flexion, and rotation.
The starting position for measuring lumbar flexion using the dual-inclinometer (AMA) technique is indicated by red lines and dots, which represent the bony landmarks for inclinometer alignment (midline of the spine is aligned with the PSIS and that it is 15 cm above the baseline mark make sure of that.
The end range of motion (ROM) of lumbar flexion is also indicated by red lines and dots, which represent the bony landmarks for inclinometer alignment (The mark 15 cm above the baseline should be aligned with the midline of the spine and the PSIS).
Conclusions
Most people only use a small portion of their full range of motion when performing daily activities, as per this study’s quantification of lumbar motion required for simulated ADLs. This study’s findings can serve as a baseline for clinicians to accurately evaluate preoperative impairment and post-surgical outcomes.
The natural decrease in flexion, side bending, and rotation in this population aligns with typical development changes in the neuromuscular and musculoskeletal systems. Between ages 5 and 11, individuals continue to build strength and motor control. Ossification of the lumbar spine is complete by ages 7 to 9, and lumbar facet orientation matures around age 11. Changes in spinal mobility observed between ages 5 and 11 could represent a developmental pattern.
FAQs
What is the range of motion of L4 L5?
The range of motion for L4-L5 is measured in degrees and corresponds to a moment of 8 Nm during flexion and 6 Nm in extension. The range of motion has a tolerance of ±6 Nm during lateral bending and ±5 Nm during axial rotation.
What is lumbar motion?
The lumbar region of the spine allows for bending forward and backward, side-to-side movements, and turning. These movements are the result of the individual segments in the spine. Each of these segments has six degrees of freedom, which allow for both rotational and translational movements in all three spatial planes.
Is the L4-L5 disc bulge serious?
A bulging disc at the L4-L5 level can result in serious health problems, including impotence and reproductive difficulties. Additionally, it may cause infertility, a loss of bowel or bladder control, paralysis in one or both legs and even death.
What is the lumbar used for?
A spinal tap, also known as a lumbar puncture, can be performed to achieve the following objectives: Obtain cerebrospinal fluid for testing purposes to identify infections, inflammation, or other illnesses. Evaluate the pressure of cerebrospinal fluid. Administer spinal anesthetics, chemotherapy drugs, or other medications.
Can lumbar nerves heal?
After a nerve is cut or damaged, it will undergo a process of self-repair. The axons, or nerve fibers, will initially shrink back and take approximately one month to ‘rest’ before they begin to grow again. Axons will regenerate at a rate of around 1mm per day. However, the extent to which the nerve will recover is variable, and the recovery will never be complete.
References
- MEASUREMENT regarding the LUMBAR and THORACIC SPINE’S MOTION RANGE. Musculoskeletal Key. https://musculoskeletalkey.com/measurement-of-range-of-motion-of-the-thoracic-and-lumbar-spine/
- Pediatric physical and occupational therapists’ consensus opinion about the characteristics of hypotonia in children. Pediatric Physical Therapy. https://doi.org/10.1097/01.pep.0000155630.54603.b6
- Lumbar Spine Range Of Motion.Physiopedia. https://www.physio-pedia.com/Lumbar_Spine_Range_Of_Motion


I am a 78 yo female in Washington, D.C. area, searching for the ideal treatment, recovery/healing from compression fractured L3, and the relevant physical therapy after 8 weeks post injury. Would appreciate relevant response offered.!
Please Find Best Physical Therapy Clinic near in your area!