Iontophoresis
What is Iontophoresis?
Iontophoresis is a medical method that uses small electrical currents to transfer drugs across biological membranes, usually while the injured body part is submerged in water.
Iontophoresis is generally used to treat hyperhidrosis, which is characterized by chronic and profuse sweating.
Currents are frequently administered to the hands, feet, or armpits, for a moment blocking the sweat glands. Some people experience a mild tingling sensation during the operation, but the electrical current is not powerful enough to shock them.
Sweating can occur in a variety of circumstances, including warm weather and physical activity, as well as for no apparent cause. It can also be triggered by medical disorders like hyperthyroidism or menopause. In addition to treating hyperhidrosis, iontophoresis can be used to treat sports injuries by administering anti-inflammatory drugs straight to the skin.
How Does It Work?
Iontophoresis uses electricity to transport medicine through the skin and into the affected tissues. It is most typically used to decrease sweat, especially in the hands and feet, but it may also be utilized in physical therapy to decrease inflammation, scar tissue, and pain. This works by applying fundamental electrical polarity principles, which state that opposing polarity (one positive and one negative ion) attracts, but negative polarity (both positive and negative ions repels). The drug used in iontophoresis is in a polarity-specific solution.
A Physical therapist will apply electrodes to your body. When voltage is supplied to medicine via the negative electrode of an electrical stimulation device, the electrical charge opposes the negatively charged medicament. This helps the drug penetrate your skin and underlying tissues.
Principle of Iontophoresis:
- Current required
- Ionic polarity.
- Low-level amplitude
- Electrode size.
Currently required:
A direct (galvanic) current is required to ‘drive’ ions into tissues.
A monophasic pulsed application can also be utilized.
Constant current is desirable over constant voltage. Thus, the applied current will not exceed the specified amount of skin resistance.
Ionic polarity:
Successful ion transfer is based on the physical premise that like poles repel and dissimilar poles attract.
Ions with the same polarity as the stimulating electrode are rejected into the skin.
The active electrode is the one that holds the ionic solution.
The electrode that completes the circuit is known as the Returning, DISPERSIVE, INDIFFERENT, or NOT ACTIVE electrode.
Low-level Amplitude:
Low-level amplitude is more effective.
The therapy typically uses currents of up to 5 mA.
at modest ionic concentrations (up to 5%).
Treatment sessions generally from 10 to 30 minutes.
Electrode size:
The negative electrode should be bigger than the positive electrode.
Increasing the size of the negative electrode reduces the current density on the pad, reducing discomfort.
Iontophoresis is used for what?
Iontophoresis is mostly used to treat specific regions of excessive sweating (hyperhidrosis), most commonly on the palms or soles. Tap-water iontophoresis works less well in the axilla.
There is limited strong evidence available; nevertheless, some studies estimate that up to 80-85% of individuals with palmar hyperhidrosis have subjective relief in their symptoms within 2-4 weeks.
In one tap-water iontophoresis study, after 14 days, there was a 33% and a 37.5% improvement in the soles and axillae, respectively, which improved to 78% and 75% after 20 days.
- Iontophoresis has a wide range of applications:
- Decrease inflammation.
- Decrease pain.
- Decrease muscular spasms.
- Reduces swelling and edema.
- Manage scar tissue
- Reduce calcium deposits
Iontophoresis has also been effectively utilized to transfer medications to the skin.
- An anticholinergic drug such as botulinum toxin A can help to reduce perspiration even further.
- Lignocaine should be used to anesthetize a specific region of the skin.
- Treat fungal infections of the nail plate (onychomycosis).
- Use silver ions to eradicate infections caused by resistant microorganisms.
- Use anti-inflammatory medications to treat bursitis or tendonitis.
Mechanism of iontophoresis:
Iontophoretic transport is typically carried out by two methods.
Electro-migration
Electro-osmosis
Electromigration: it is also known as electrorepulsion. Ions migrate across a membrane (the skin) in response to an electric field. There are two electrodes: cathode and anode. When an electric field is applied, negatively charged medications resist into the skin beneath the cathode, and positively charged pharmaceuticals transfer under the anode.
Electro-osmosis: The second mechanism, electro-osmosis is defined as the volume flow caused by current flow. It is determined by the molecules’ physiochemical characteristics as well as the polarity of the applied current. For example, when negative charges are deposited on the cathode (-), they move transdermally to the anode (+).
Points to Remember:
- Drug delivery is local, but only penetrates a few millimetres.
- Drugs must be ionized and have a net charge (+ or -).
- Negative charges are deposited on the cathode (-) and move transdermally to the anode (+).
- Positive medicines are applied to the anode (+), and they move transdermally to the cathode.
- The electrode via which the medication is given is designated an active electrode. The dispersive electrode is normally the opposite electrode.
Physiological changes in iontophoresis:
- ion penetration
- acid/alkaline responses
- Hyperemia
- dissociation
Ion penetration:
Penetration is limited to 1mm, followed by deeper absorption by capillary circulation. The active electrode stores the majority of deposited ions, which are thereafter reduced by the blood’s flow.
Acid/alkaline reactions:
ACID will accumulate beneath the POSITIVE electrode (weak HCL).
This is because negatively charged chloride ions (CL- from NACL) are attracted to the anode.
This is considered sclerotic, which hardens tissues and acts as an analgesic by releasing oxygen locally.
Alkaline buildup occurs under the negative electrode (cathode) as positively charged sodium ions (NA + from NACL) flow towards it.
Na+ ions react with water to produce sodium hydroxide (NaOH).
Sclerolytic is a softening agent that releases hydrogen and helps control scars and burns.
Hyperemia:
Both positive and negative electrodes cause vasodilation, resulting in hyperemia and heat.
Cathodal hyperemia typically persists longer than anodic hyperemia.
Hyperemia beneath both electrodes often lasts no longer than an hour.
Dissociation:
Ionizable compounds break down in solution, producing ions that migrate to the opposite pole when exposed to direct current.
Absorption occurs through capillary circulation.
This is an example of ion transfer.
Types of electrodes in iontophoresis:
- Traditional
- Commercial
- Traditional electrodes:
- Older electrodes were constructed of tin, copper, lead, aluminum, or platinum and supported with rubber.
- Cover the skin fully with a sponge, cloth, or gauze.
- The absorbent material is soaked with an ionized solution. For medicinal ointments, apply them to the skin and cover with absorbent material.
- Commercial electrodes:
- Sold with most iontophoresis systems.
- Electrodes consist of a tiny chamber with a semipermeable membrane that allows for the injection of ionized solutions.
- The electrodes naturally connect to the skin.
Parameters of iontophoresis:
Maximum Safe Current Density (MSCD).
Cathode: 0.5 mA/cm².
Anode: 1.0 mA/cm².
The maximum safe current intensity (MSCI) is obtained by multiplying the MSCD by the electrode’s surface area.
MSCD equals MSCI/SAE.
The calculation of dosage involves multiplying intensity by duration (D = Ma × min).
Typical dose ranges from 40 to 80 mA×min.
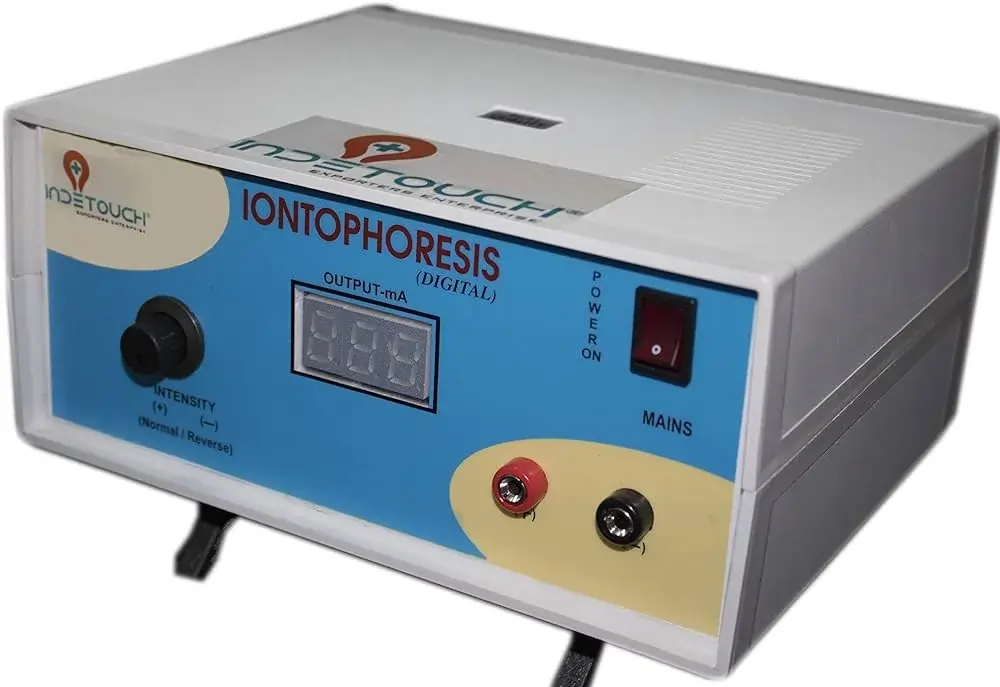
Requirement of the apparatus:
- The equipment requires a low-voltage, direct current source with low amperage.
- A shallow plastic tray for the anode.
- A sole or arm bath for the cathode.
- Two big electrodes and leads.
- Two big lint cushions protect the electrodes.
- Solution of anticholinergic compounds
- Distilled water
Various Medications Used With Iontophoresis:
Iontophoresis can be used with a variety of drugs to get varying outcomes. This may include:
- Dexamethasone controls inflammation.
- Acetic acid is often used to treat myositis ossificans, which occurs when bone tissue forms within a muscle, and adhesion capsulitis, which limits shoulder movement, as well as to eliminate accumulations of calcium.
- Sodium chloride is used to break down and cure scar tissue.
- Calcium chloride: Used to reduce muscular spasms.
- Tap water helps reduce hyperhidrosis, a disorder that causes sweating palms and feet.
- Magnesium sulfate is used to alleviate muscular discomfort and spasms.
- Iodine is used to treat sclerotic disorders like frozen shoulder, and it may aid in improving circulation to tissues.
- Hyaluronidase is commonly used to treat soft tissue swelling and edema (swelling caused by excessive fluid).
What it feels like:
When your physical therapist decides to provide medicine using iontophoresis, the therapist should discuss the risks and advantages of the practice. A therapist will next apply two electrodes to your skin. One electrode will be saline, while the other will be the treatment electrode with the drug. The electrodes will be linked to an iontophoresis equipment by a wire.
Your physical therapist will then activate the iontophoresis equipment and gradually raise the strength of the electricity that passes through the electrodes. This energy helps to propel the drug through your skin and into your tissues. When the electricity is turned on, you may experience a little tingling or stinging feeling beneath the electrodes. Tell your physical therapist if you experience any discomfort or pain throughout the process. The therapist can alter the voltage to make it more pleasant for you.
Treatment methods for iontophoresis:
Hands

The shallow plastic tray is put on an arm bath table, with the patient sitting next to it.
The active electrode (anode) is put in a plastic tray and covered with one of the lint pads.
The pads should be at least eight layers thick to provide proper contact with the tissue and the electrode while also effectively absorbing any chemicals that may develop throughout the therapy.
The tray includes a 0.05% solution of glycopyrronium bromide in distilled water, which acts as an anticholinergic and effectively covers the palm.
The hand is put in the tray, with the electrode linked to the treatment unit’s positive terminal.
One foot is immersed in warm water in the foot bath, and the negative terminal is linked via an electrode covered by a lint pad.
The current is turned on and gradually raised to the required level for the specified period.
Feet
To treat feet, reverse the setup by placing the shallow tray with an anode on the floor and the arm bath with a cathode, allowing the arm to complete the circuit.
Iontophoresis for hyperhidrosis:
- Iontophoresis treatments for hyperhidrosis typically last 25-45 minutes. However, you will most likely require more than one session to see an improvement in your symptoms.
- Some persons with hyperhidrosis require frequent treatments. Your doctor will set up a series of sessions based on your symptoms. They may propose that you purchase a portable unit for use at home.
Iontophoresis for Sports Injuries:
- When utilized to treat a sports injury, iontophoresis is always done in a doctor’s office. Your healthcare professional will add anti-inflammatory medicine to a basin of water, and you will immerse the affected region in the water.
- Your doctor will next apply a modest electrical current to the medicinal water. The electrical current will provide tingling sensations, but they should not be uncomfortable.
- Most iontophoresis treatments for sports injuries last between 10 and 15 minutes. Your doctor may suggest many treatments each week until your injury heals.
- Iontophoresis is a non-invasive, painless treatment. Iontophoresis may cause some people to develop side effects, although these are often minor.
- The most prevalent adverse effect is dry skin. Blistering, peeling, and inflammation may also develop on the skin.
- However, these adverse effects are frequently alleviated by applying moisturizer to the skin following each session. Over-the-counter hydrocortisone cream may also help you feel more comfortable.
- Iontophoresis for cancer:
- Iontophoretic devices can administer various anti-cancer medicines.
- These devices have demonstrated potential in pre-clinical and clinical trials for retinoblastoma (an eye cancer), skin, bladder, and pancreatic cancer.
- Iontophoresis can also be used to administer chemotherapy drugs for the treatment of head and neck cancer.
- Local iontophoretic chemotherapy treatment reduces medication adverse effects and is recommended for medicines that are harmful when administered systemically.
- Cisplatin and 5-fluorouracil, two anti-cancer medications that may be delivered by iontophoretic devices, are used to treat skin cancer.
- Iontophoresis can also be used to give other anticancer medicines, such as imatinib mesylate and the STAT3 siRNA complex.
Dosage of the Iontophoresis:-
- Dosage for Iontophoresis depends on patient size and skin tolerance.
- For an average adult, 12 milliamps for 13 minutes is recommended, but a youngster needs half that amount.
- The necessity to repeat the therapy varies per patient.
- Some conditions need months of recovery after a single treatment, while others require a repeat treatment within four to six weeks.
Complications of iontophoresis:-
- Chemical burns
- Heat burns
- Ion-related sensitivities and allergies.
Chemical Burns:
This is due to excessive production of sodium hydroxide at the cathode.
Initially pink, the skin becomes grey and leaks wound after a few hours.
This burn takes a long time to heal.
Treatment should include antibiotics and clean dressings.
Burns under the anode are uncommon and manifest as a hardened red patch, akin to a scab.
Heat Burns:
Excessive heat in high-resistance zones causes burns.
The electrodes are not wet enough. – They do not fit well or make excellent skin contact.
Treatment should include antibiotics and clean dressings.
Allergic responses to ions:
If a patient is allergic to shellfish, avoid using “iodine”.
Patients with active peptic ulcers or gastritis have a poor response to ‘hydrocortisone’.
Patients with aspirin sensitivity may respond negatively to salicylates.
Patients who are sensitive to metals may respond to copper, zinc, or magnesium.
How many times taken this treatment?
- The treatment time ranges from 10-20 minutes.
- The patient should be comfortable, with no reported or apparent discomfort or burning.
- Check skin every 3-5 minutes for symptoms of irritation.
Side effects of iontophoresis:
Iontophoresis is a safe technique with few side effects. It is critical to prevent direct contact with the electrodes during therapy, which may result in a small electrical shock.
Most people suffer from pins and needles or a burning sensation. Adverse consequences might include:
Redness on the treated skin
Small blisters (vesicles), called pompholyx
Dermatitis, or dry, cracked skin.
Although these iontophoresis side effects are likely to subside within a few days, emollients/moisturizers should be used multiple times per day to alleviate discomfort. Topical corticosteroids can be used.
Anticholinergic medications, such as glycopyrrolate can be absorbed into the body and cause systemic adverse effects such as dizziness, dry eyes, and dry mouth.
Contraindications to Iontophoresis:-
Iontophoresis should not be used on patients with epilepsy or a history of seizures.
- A patient with a cardiac ailment or pacemaker
- A patient has a metal implant.
- A pregnant lady.
- Patients should postpone therapy if they have a recent wound, skin graft, or scar in the treatment location, as iontophoresis can be uncomfortable and ineffective.
Precautions for iontophoresis:
Skin Sensitivity: Certain people may have sensitive skin that reacts to the electrical current utilized in iontophoresis. It is critical to check the skin throughout treatment and alter the intensity if discomfort or irritation arises.
Electrolyte Imbalance: Because iontophoresis uses electrical current to force ions into the skin, there is a danger of affecting electrolyte levels in the body. This is particularly critical when electrolyte-containing drugs are administered during iontophoresis. Monitoring electrolyte levels may be required in such cases.
Allergic Reactions: Patients should be tested for allergies to any drugs or chemicals used during iontophoresis. Allergic responses can range from moderate skin irritation to more serious reactions that need medical treatment.
Skin Integrity: Iontophoresis should not be used on damaged or fractured skin since it might cause further irritation or infection. Before beginning therapy, ensure that the skin is undamaged and healthy.
A Specialist Supervision: Iontophoresis should be performed under the supervision of a skilled healthcare expert who can monitor the therapy, alter settings as needed, and handle any issues or concerns that occur.
- Do not use two chemicals on the same electrode, even if they have the same polarity.
- Avoid administering ions with opposing polarity during the same therapy session.
FAQs
Iontophoresis is used for what?
Iontophoresis is mostly used to treat hyperhidrosis, which causes excessive sweating.
What ion is utilized for iontophoresis?
Iontophoresis uses chlorine, a negatively charged ion, to repair keloid scars and scar tissue.
What are the downsides of Iontophoresis?
Minor responses, such as itching, erythema, and general iontophoretic skin surface irritation, are common.
Is iontophoresis safe?
Iontophoresis has few side effects and is well tolerated by the majority of patients. There is a brief tingling feeling during and after treatment.
Who should avoid iontophoresis?
Patients who have a history of hypersensitivity or bad responses to the medicine being given should avoid iontophoresis.
What is the definition of iontophoresis in simple terms?
Iontophoresis is the method of conducting a small electrical current via the skin. Iontophoresis has several applications in medicine.
References
- Roth, E. (2021, February 8). Iontophoresis. Healthline. https://www.healthline.com/health/iontophoresis
- Iontophoresis | DermNet. (n.d.). https://dermnetnz.org/topics/iontophoresis
- Iontophoresis. (n.d.). Physiopedia. https://www.physio-pedia.com/Iontophoresis
- Pt, B. S. (2022, November 21). Iontophoresis in Physical Therapy. Verywell Health. https://www.verywellhealth.com/iontophoresis-in-physical-therapy-2696534
- Ladva, V. (2023, November 11). Iontophoresis – A Non-Invasive Treatment for Hyperhidrosis. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/iontophoresis/
- V. (2022, January 2). Iontophorosis : Indication, Contraindication, Precaution. Mobility Physiotherapy Clinic. https://mobilephysiotherapyclinic.net/iontophorosis/