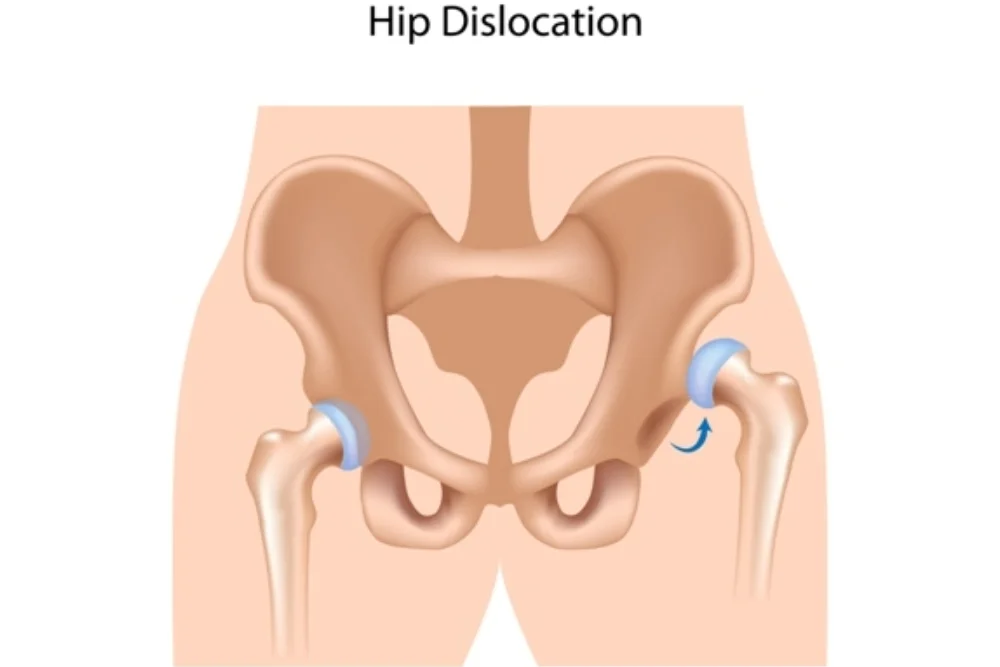
Hip Dislocation
Introduction
Hip dislocation occurs when the ball of the femur (thigh bone) is forced out of its socket in the pelvic bone, typically resulting from high-impact trauma like a car accident or severe fall.
Most frequently, this injury happens in an automobile accident, high-impact fall, at work, or in sports, particularly when it also results in a fractured pelvis or leg. When the femur, or ball joint, positions separated from the acetabulum or socket, it results in a hip dislocation. There is an urgent medical situation.
A displaced hip can be crippling and extremely painful. If a dislocated hip is severe or not properly treated within hours of the incident, it may result in major, lifelong, impairing issues. A person should be evaluated by an orthopedic specialist to rule out a hip dislocation if they sustain any kind of strong impact that causes severe hip discomfort or discomfort in the knee, leg, or even the groin. Short-term problems are less likely when treated right away.
Anatomy of Hip Joint
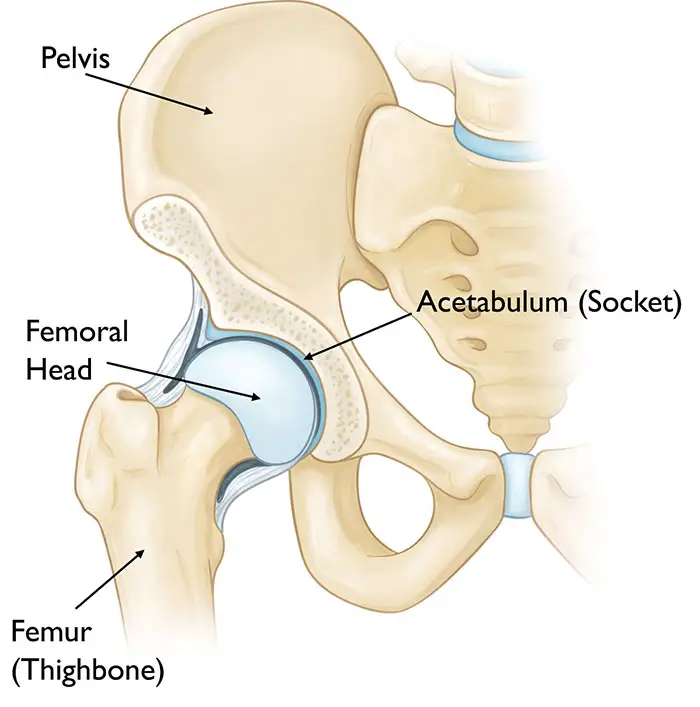
- The anatomy of the hip joint consists of a ball and socket.
- The acetabulum, a component of the big pelvic bone, forms the socket.
- The femoral head, or top end of the femur, is the ball.
- The surface of the ball and the socket are covered in a smooth substance known as articular cartilage. It produces a surface that is low-friction, facilitating easy bone-to-bone movement.
- The surface of the ball and the socket are covered in a smooth substance known as articular cartilage. It produces a surface that is low-friction, facilitating easy bone-to-bone movement.
- The labrum, a strong fibrocartilage, encircles the acetabulum. The labrum serves as a barrier that securely seals the socket and enhances joint stability. The strong bands of tissue known as ligaments give the hip joint extra stability.
- The head of the femur rests comfortably inside the acetabulum in a healthy hip.
What is Hip Dislocation?
- A painful condition known as hip dislocation occurs when the hip’s ball joint pops out of its socket. The cause generally includes a significant traumatic injury. (It is a little bit easier to dislocate an artificial hip replacement.)
- An injured hip requires immediate medical attention. Until it is fixed, it incapacitates your leg and produces severe pain. It may also cause secondary harm to nearby blood vessels, ligaments, nerves, and tissues. Long-term harm may result from hip dislocation, particularly if it is not immediately treated.
- A developmental condition known as hip dysplasia causes your hip joint to not fit properly in its socket. It can occasionally lead to hip dislocation. Hip dysplasia frequently gets referred to as developmental dislocation. Hip dysplasia patients have shallow hip sockets, which make it harder for their joints to stay in position than it would be for healthy hips. It’s also possible that they have loose hip ligaments and muscles, which means it takes less effort to dislocate their joint than it would for the majority of us.
What is a Subluxation, or Partial Hip Dislocation?
- In medical terms, an incomplete dislocation is categorized as a subluxation. It indicates that your ball joint has slipped partially away from its socket, but not completely. A subluxation may be moderate or severe. It is common in patients who have hip dysplasia or have had their hip replaced.
- Injuries are commonly the cause of severe subluxations. More severe occurrences may be as painful and debilitating as a total dislocation, necessitating a healthcare professional’s intervention. Listen to your body and seek professional assistance if you are in extreme pain or unable to walk.
- A lesser case may result from general wear and strain on your hip, such as damaged cartilage that helps seal your joint in its socket. It could be chronic or recurrent. If you have a mild subluxation, you may be able to walk and gently stretch it back into position.
What are the different types of Hip Dislocation?
- Posterior dislocation
- Anterior dislocation.
- Central dislocation
Posterior dislocation
- Among the three kinds of hip dislocations, it occurs most frequently.
- It happens when there is a forceful thrust to the knee that pushes the adducted and flexed femur backward, like when a passenger’s knee strikes the dashboard of an automobile.
- The posterior hip of the acetabulum may fracture as a result of the femoral head being forced backward.
Clinical Symptoms:
- Significant localized discomfort and tenderness.
- The lower limb posture with a posterior dislocation consists of internal hip rotation, flexion, and adduction. There is identified limb shortening.
- The attempted movement was stiff and unpleasant.
- Localized hematoma
- The femoral head is palpable posteriorly at the gluteal area.
- The decreased femoral pulsation
Anterior dislocation
- It is uncommon and happens because of violent abduction force, with the thigh flexed.
- It happens in road traffic accidents.
- The displaced head of the femur might rest on the obturator foramen or the symphysis pubis.
Clinical Symptoms:
- Tenderness, stiffness, and localized discomfort.
- Inability to weight-bearing
- The limb seems to lengthen as it is externally rotated.
Central dislocation
- This kind of dislocation happens when someone falls onto their greater trochanter or when they are in an automobile accident.
- The acetabulum base fractures as a result of the femoral head being forced deeply into the pelvis.
Clinical Symptoms:
- Severe stiffness and localized discomfort
- When attempting to move the hip joint, there is considerable pain and restrictions on hip abduction and rotation.
- The lower limb stays in a short, neutral rotational position.
What are the causes of the Hip Dislocation?
- The most frequent cause of traumatic hip dislocations is motor vehicle crashes. When a knee collides with the dashboard, it frequently dislocates.
- This strain forces The thigh backward, forcing the femur’s ball head out of the hip socket.
- Using a seatbelt can significantly lower your chance of hip dislocation in an accident.
- A hip dislocation can also result from an industrial accident or a fall from a considerable height, such as a ladder.
- Hip dislocations can occur from collisions during sports, such as hockey or football, however, they are significantly less common.
- Hip dislocations frequently result in other injuries, such as head, back, abdomen, and leg fractures as well as pelvic and leg fractures. The most widespread fracture occurs when the posterior portion of the hip socket is damaged due to a collision with the femur head after a concussion. This phenomenon is referred to as a posterior wall acetabular fracture and dislocation.
- In children: It may require significantly less effort to dislocate the joint if the child has developmental hip dysplasia or hip dislocation.
- Occasionally due to underlying medical issues, such as neuromuscular diseases or cerebral palsy.
What is the appearance of a Dislocated Hip?
- Your leg is trapped in a fixed posture, rotated inward or outward if you view the injury from the outside.
- Your hip joint is driven backward out of its socket (posterior dislocation) about 90% of the time, causing your foot and knee to point inward. Your knee and foot will point outward if your hip is forced forward from its socket (anterior dislocation).
- Twisted legs may look longer or shorter than the other. You might see hip discoloration or swelling, or you might be able to detect that your hip isn’t aligned.
What are the risk factors for the Hip Dislocation?
- Compared to women, men are more likely to have suffered from hip dislocations.
- You have an increased chance of experiencing another hip dislocation if you have already had one.
- Common causes include falls from heights, motorbike accidents, and car crashes.
- Sports involving contact, such as rugby, football, and hockey, can raise risks.
- A disorder when there is an incorrect formation of the hip joint, increasing the risk of dislocation.
- Rheumatoid arthritis and osteoarthritis can weaken the joint, increasing the risk of dislocation.
- Osteoporosis and osteonecrosis are two conditions that can weaken bones and raise the risk.
- Fall risk is increased by conditions that affect balance and coordination, such as cerebral palsy and Parkinson’s disease.
How are Hip Dislocations Diagnosed?
Medical History:
- The doctor will ask about the circumstances that led to the injury, previous hip problems, and any associated symptoms.
Physical examination:
- The doctor will check the hip joint’s range of motion, stability, and discomfort. They may additionally look for nearby areas for additional injuries.
Imaging tests:
- A pelvic x-ray taken from the front and back would confirm the diagnosis.
- An excess of the femur’s head or neck and the acetabular edge may be shown on the X-ray.
- Labrum and cartilage can be found with an MRI.
- Accurate visualization of the bone and soft tissues surrounding the hip joint, including bursae and ligaments, is possible with CT scans.
- To identify malignancies, necrosis, and stress fractures in the hip, scintigraphy, or bone scans, are utilized.
- One method for identifying hip irregularities and soft tissue issues like edema is ultrasonography.
What is the treatment for Hip Dislocations?
Hip dislocations can be treated both surgically and non-operatively. Time for reduction is important because the longer the hip is dislocated, the higher the risk of avascular necrosis in the native hip, according to several studies.
Non-surgical Treatment
Hip dislocation is prevented by applying traction force in the opposite direction when the hip is at a 90° flexion. This is known as closed relocation of the hip. To avoid further damaging cartilage and soft tissue, this should ideally be performed under general or regional anesthetic with muscular relaxation.
In a theater, it could potentially be performed under anesthesia. The hip’s stability should be closely examined following the relocation. Depending on the hip’s stability and the severity of the soft tissue damage, a period of bed rest may be advised.
Surgical Treatment
Surgical Guidelines:
- Ineffective conservative approach
- Instability after a conservative move
- Associated acetabular or femur head fractures
- Pieces of loose bone in the joint area following the reduction.
Hip arthroscopy: This procedure can be performed to look for chondral damage and intra-articular fractures as well as to remove fragments from within the joint.
Hip replacement: If relocation and stabilization of the related injuries do not result in satisfactory stability, hip replacement surgery may also be considered. Dislocation after hip replacement surgery may need revision surgery to guarantee the hip’s long-term stability.
Open reduction indicators: When challenged with difficult relocations or when any obstacles (such as loose pieces or soft tissue) hamper closed reduction.
Decreasing neurological symptoms after closure reduction, particularly after posterior dislocation for sciatic nerve function.
Cases where leg manipulation is not advised in individuals with proximal femur fractures.
What is the physical therapy for Hip Dislocations?
People who have dislocated their hips will need a lot of physical therapy. The amount of time needed for soft tissue healing (and bone healing in cases where there are accompanying fractures) must be carefully taken into account during hip dislocation rehabilitation. The orthopedic surgeon will guide any potential weight-bearing limits that may arise after hip medical therapy. Following a hip dislocation, recovery can be completed in three to six months.
- Gait training: Starting with crutches or a walking frame to restrict weight bearing, and progressing from there.
- Boost hip mobility, using hip mobilizations.
- Strengthening of hip-supporting muscles, with a focus on hip stabilizers such as hip flexors, hip extenders, hip abductors, and hip adductors.
- Stretching
- Graded return to sport or activity
To lessen discomfort and inflammation during a hip dislocation physical therapy treatment plan, therapists may employ modalities like
- Ice.
- Ultrasound.
- Electric stimulation.
- Cold laser.
Prognosis
After a dislocation, the hip requires some time to heal up to two-three months. Further fractures could result in a prolonged recuperation period. To prevent the hip from dislocating once more, the doctor could advise restricting hip motion for a few weeks. Physical treatment is frequently advised when recovering. In a short amount of time, patients frequently start to walk with crutches. Walking aids assist patients in regaining their movement. Devices ranging from crutches, walkers, and, finally, canes.
What are the complications of Hip Dislocation?
Long-term effects may result from a hip dislocation, especially if there are accompanying fractures.
- Nerve damage: Nerves in the hip can be crushed and stretched when the femur is forced out of its socket, especially in posterior dislocations. The most frequently affected nerve is the sciatic nerve, which runs from the lower back down to the back of the legs. A sciatic nerve damage might result in lower limb paralysis as well as typical mobility impairment in the knee, ankle, and foot. Approximately ten percent of sciatic injury cases originate from hip dislocation. Most of these patients will recover some nerve function.
- Osteonecrosis: The femur can rip blood vessels when it is forced out of its socket. Osteonecrosis, also known as avascular necrosis, is the outcome of a bone dying due to a lack of blood flow. This is a painful ailment that may eventually result in arthritis and hip joint degeneration.
- Arthritis: Damage to the protective cartilage that covers the bone may also occur, raising the possibility of joint arthritis. Arthritis may eventually necessitate other surgeries, such as a total hip replacement.
How to prevent Hip Dislocation?
- Safety: Standard safety precautions are the best defense against hip dislocation, which typically occurs as a consequence of an accident. When driving, buckle up, and when playing contact sports, put on protective gear. Furthermore, proceed with caution when utilizing a ladder or other work equipment.
- Posture awareness: Sit with your back in a neutral position and your feet flat on the floor. Do not cross your legs. Avoid bending forward when seated on a chair. Your knees ought to stay apart. Position a wedge or pillow between your knees when you sit or lie down. Do not bend your knees. Do not elevate your knees higher than your hips.
- Steer clear of low chairs. Using the armrests and your upper body strength, push yourself up to stand from a seated posture. When you are picking anything up off the ground, try not to bend at the waist. You can bend your knees or use a tool to pick up the object.
- Conditioning: Your hip may be more prone to dislocating again if you have already experienced one. By maintaining your hip tendons and muscles conditioned through regular exercise and strengthening them through physical therapy, you can assist in strengthening your joints.
- Treatment for hip dysplasia: To avoid further harm, children with this condition should receive treatment while their skeletons are still forming.
Summary
Don’t mess around with a dislocated hip. It’s a medical emergency, and both short-term relief and long-term healing rely on prompt treatment. Most likely, a stressful incident led to your dislocated hip. If this is the case, there are likely to be additional injuries such as fractures and rips. However, if you have a replacement hip, it may have dislocated more easily, even while sitting in a low chair or crossing your legs.
You may not have secondary injuries, but treating the dislocated hip is still important for relieving pain and restoring functionality. Quality medical care will assist you in preserving as much hip functionality as possible for an extended period. If you think you may have a dislocated hip, don’t wait to get emergency attention.
FAQs
What causes hip dislocation mostly?
The most frequent cause of traumatic hip dislocations is motor vehicle crashes. When a knee collides with the dashboard, it frequently dislocates. This strain forces the thigh backward, forcing the femur’s ball head out of the hip socket.
Even with a dislocated hip, are you still able to walk?
A hip dislocation arises when the hip’s ball joint dislodges from its socket. Until it is realigned, this painful medical emergency usually keeps you from walking. Most hip dislocations happen because of trauma, which takes months to heal and sometimes requires surgery.
Can I sit when my hip gets dislocated?
During the healing process following a dislocated hip, you must refrain from bending your hip past 90 degrees. When you sleep on your side, keep the top leg from crossing over the bottom leg by placing a pillow between your legs and knees. Don’t cross your legs when seated.
What is the hip dislocation’s immediate course of treatment?
A hip dislocation requires immediate medical attention. Seeking early medical attention is a crucial aspect of the treatment plan. A “closed reduction” is the standard approach used by paramedics or other medical personnel to realign the hip joint. This is frequently done while under sedation.
How long does it generally take to heal from a hip dislocation?
Following a hip dislocation, recovery is contingent upon the extent of the damage and any coexisting issues. To allow the hip to heal, it typically entails a period of immobility with a wheelchair, crutches, or brace. It is common to offer physical therapy and rehabilitation activities to regain range of motion, flexibility, and strength.
Does a hip dislocation have any long-term complications?
Even though most hip dislocations respond well to treatment, problems are possible. Hip instability, repeated dislocations, fractures, injury to nerves or blood vessels, avascular necrosis (inadequate blood supply to the femur head), and the onset of post-traumatic arthritis are a few examples of these.
References:
- Hip Dislocation – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/hip-dislocation
- Hip Dislocation. (2024b, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22222-hip-dislocation
- Weatherford, B. (n.d.). Hip Dislocation – Trauma – Orthobullets. https://www.orthobullets.com/trauma/1035/hip-dislocation
- Dislocated Hip Symptoms, Diagnosis, and Treatments | HSS. (n.d.). Hospital for Special Surgery. https://www.hss.edu/condition-list_hip-dislocation.asp
- Williams-Johnson, J., Williams, E., & Watson, H. (2010). Management and Treatment of Pelvic and Hip Injuries. Emergency Medicine Clinics of North America, 28(4), 841–859. https://doi.org/10.1016/j.emc.2010.07.002
- Sutariya, H. (2023, June 9). Hip Dislocation – Type, Cause, Symptoms, Diagnosis, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/hip-dislocation/