Genitofemoral Neuralgia
Genitofemoral neuralgia is a chronic condition that affects the genitofemoral nerve, characterized by sharp, burning, or aching pain in these areas, often triggered by movements, pressure, or prolonged sitting. The genitofemoral nerve can become irritated or compressed due to various factors, including surgery, trauma, or certain medical conditions.
Diagnosis can be challenging due to the overlapping symptoms with other conditions, making it essential for healthcare providers to perform a thorough evaluation. Treatment options range from conservative approaches like physical therapy and medications to more invasive procedures such as nerve blocks or surgery, depending on the severity of the condition.
What is Genitofemoral Nerve? Anatomy and its Function
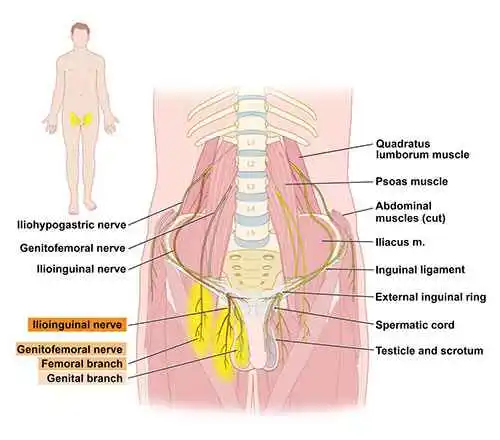
Serving the lower limbs, the genitofemoral nerve is a merged peripheral nerve. It facilitates the male cremaster muscle and adds to the sensation of the genitalia and thigh. The branches arising from the anterior rami of the L1 and L2 nerve roots combine to generate the genitofemoral nerve, which can be found in the middle of the psoas muscle. The nerve emerges distally from the anterior surface, having passed inferiorly via the psoas muscle.
Course
- The genitofemoral nerve develops in the lumbar plexus, which is made up of fibers from the L1 and L2 spinal roots.
- It goes down inferiorly along the posterior abdominal wall after passing across the anterior side of the psoas major muscle.
- When the nerve reaches the inguinal ligament, it splits into two branches.
Genital Branches:
- In males, it crosses the scrotum via the inguinal canal and transmits feeling to both the cremaster muscle and the lateral region of the scrotum.
- It transmits with the region around the thigh, the labia majora, along with the mons pubis in females.
Femoral branch
- Femoral branch, after traveling behind the inguinal ligament and reaching the thigh, cutaneous branches extend to the skin surrounding the femoral triangle.
Sensory Functions
- The skin covering the femoral triangle receives cutaneous innervation from the femoral branch of the genitofemoral nerve.
- The lateral scrotal skin is delivered through the genital branch of the genitofemoral nerve in men and females, it delivers the labia majora, the mons pubis, along with the nearing area of the thigh.
Movement Function
- Regulation of the cremaster muscle is provided via the pelvic branch of the genitofemoral nerve.
- It controls the efferent limb of the cremasteric reflex, which involves the contraction of the cremaster muscle and subsequent elevation of the testis in response to ilioinguinal nerve stimulation.
What is Genitofemoral Neuralgia?
- Genitofemoral neuralgia (nerve discomfort) is the term for compression neuropathy that affects both sexes (men and female). Compressed or “pinched” nerves produce discomfort in the inner thigh, lower abdomen, and groin area.
- The primary indicator of this disease is chronic neurotic discomfort in the groin that spreads across the genitofemoral nerve. Cases of genitofemoral neuropathy have been linked to iatrogenic nerve damage sustained during femoral and inguinal herniorrhaphy, following both open and laparoscopic procedures. Diagnosing this issue can be challenging because the genitofemoral nerve shares a sensory distribution with the ilioinguinal and iliohypogastric nerves.
- Following a diagnosis, genitofemoral neuralgia can be treated with a variety of techniques, including non-invasive injections, surgery, and medical management.
What Is the Cause of Genitofemoral Neuralgia?
The following conditions can lead to genitofemoral neuralgia:
- Stomach tumor
- Tightness in the psoas muscle
- Peripheral neuropathy caused by underlying medical conditions
- The third trimester of pregnancy
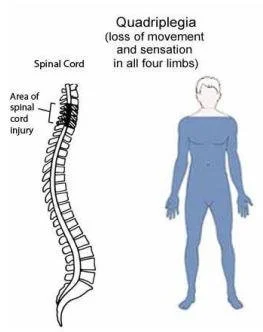
- Problems with the spinal cord
- Trauma to the abdomen or pelvis
- Unwanted outcome of surgery to repair an inguinal hernia
What are the Symptoms of Genitofemoral Neuralgia?
The most common sign of genitofemoral neuralgia is localized aching in the groin and genitalia. Furthermore, neuralgia can result in:
- Increase in sensation (hyperesthesia)
- Loss of sensation (hypoesthesia)
- More intense pain with leg rotation
- Tingling
- Loss of strength in the abdominal muscles
What are the risk factors for Genitofemoral Neuralgia?
The following variables may make you more likely to risk of getting this condition:
- The most frequent reason is pelvic or abdominal surgery, which includes operations like appendectomy, hysterectomy, hernia repair, and others.
- Abdominal or pelvic trauma: Blunt force injuries may cause nerve injury.
- Pregnancy: The nerve may be compressed by the expanding uterus.
- Underlying medical conditions: Nervous system disorders such as diabetes, multiple sclerosis, and others can make a person more susceptible to disease.
- Psoas muscle compression: This can happen for several causes and irritates nearby nerves.
- Tumors in the pelvis or stomach are frequently a source of nerve compression.
It is noticeable that genitofemoral neuralgia (idiopathic) can have an unknown origin in certain situations.
What is the diagnosis of the Genitofemoral Neuralgia?
A physical examination and a conversation about your symptoms and medical history with your doctor are the initial stages in determining whether you have genitofemoral neuralgia. These extra examinations can be required:
- Blood examinations
- Bone scan
- CT scan
- MRI
- Ultrasound
- The tests are well-tolerated and assist your doctor in determining the best course of action for your problem.
What are the differential Diagnosis for Genitofemoral Neuralgia?
Due to the overlapping in sensory circulation with different inguinal nerves, genitofemoral neuralgia can be difficult to detect. Conditions with Similar Symptoms are included in differential diagnosis.
- Ilioinguinal neuralgia
- Iliohypogastric neuralgia
- Musculoskeletal pain
- Inguinal hernia
What is the Treatment for Genitofemoral Neuralgia?
Conservative Therapy
Your physician could initially advise:
- Injections of corticosteroids
- Analgesic medications
- Patches for topical anesthesia
- Physical therapy
- Cryo-nerve excision
Surgical Therapy
- If the previously described treatment fails to alleviate the symptoms, surgery to decompress the genitofemoral nerve may be required.
- To reach the compressed nerve, your surgeon will create an incision in your belly or thigh. After the compression is released, self-absorbing stitches seal the incision. Depending on how much compression is done, the procedure could take an hour or two.
- The technique is usually carried out under anesthesia as an in-patient procedure, necessitating a one to two-day hospital stay.
- Following the procedure, patients will be taken to a recovery area so that their progress can be regularly monitored.
- The skin around the incision is likely to be numb at first, but the feeling will return as the anesthesia and painkillers leave your body. Although expected, pain and minor swelling in the treated area can be managed.
Complication after surgery
There is danger involved in every surgery, especially if anesthesia is needed. Genitofemoral nerve surgery is a sensitive and demanding procedure, yet it is often considered safe. Rare but likely complications include:
- The scrotum or labia majora lose their feeling
- Cremaster nerve reflex loss
Following Surgery, What Should Do at Home?
Your surgical success will be influenced by the actions you take at home. The following things to aid in your body’s healing process:
- Take a rest
- Utilize the prescribed painkillers to relieve both pain and swelling.
- Quit smoking to encourage circulation and healing.
- When you sleep, place extra pillows behind your tummy and between your knees for added comfort.
- Exercise lightly and gradually as you heal.
Prognosis
Since nerves repair slowly, recovering from pain resulting from both the neuralgia and the surgery itself may take four to five months. Up to a year may pass during the total recuperation process. After genitofemoral nerve decompression surgery, most patients make a full recovery.
Physical Therapy for Genitofemoral Neuralgia
A helpful option in the management of genitofemoral neuralgia is physical therapy. Even though it might not treat the nerve injury directly, it can lessen related pain and improve general function.
- Pain Management: Physical therapists can instruct patients in breathing exercises, relaxation methods, and other pain-reduction techniques.
- Postural changes: Making small adjustments to your posture may assist reduce your stress level.
- Pelvic floor workouts have been shown to help reduce tension and ease the muscles surrounding the pelvis.
- Soft tissue mobilization is a technique that helps lessen nerve discomfort by reducing tension in the surrounding muscles and connective tissues.
- Scar tissue mobilization: This method can assist reduce adhesions and increase mobility if there is a scar from previous surgery close to the nerve.
Exercises for Pelvic Muscles Strengthening
Diaphragmatically Breathing

- Diaphragmatically breathing promotes the pelvic floor and diaphragm’s functioning interaction.
- With a flat yoga or exercise mat, get started by laying down on the base. The exercise can also be done while sitting down.
- Practice increasing relaxation for a few seconds. It would help if you tried to make every effort to have your body calm.
- Utilizing one hand on the belly and one on the chest, complete a sequence of little movements.
- Inhale through your nostrils while maintaining a mostly stable chest to make your stomach develop. Take a slow inhalation and exhale after two to three seconds.
- Hold one hand on the upper chest and the other on the abdomen, and keep doing it multiple times.
- Individuals can sense your pelvic floor muscles, whether you clench the muscles that restrain you from discharging gas or stop mid-urination. These exercises will need you to activate your pelvic floor muscles.
- Initially, you may find that lying down is the most comfortable posture, but once you’ve identified which muscles in your pelvic floor are engaged, you may complete the exercises in any position.
- You should contract your pelvic floor muscles, hold them for three seconds, and then release them for the same duration of time. Repeat a couple of times after that. If you want to strengthen your muscles, you can conduct Kegel exercises while sitting, standing, or walking.
- Concentrate simply on constricting your pelvic floor muscles to earn the greatest advantages. Take caution not to flex your buttocks, thighs, or abdomen muscles.
- Breathe normally without holding it in. Instead, let your respiration be free as you perform the exercises.
- Three times a day, repeat. Make an effort to finish three sets of ten reps or more throughout the day.
Happy Child Pose

- Happy Baby Pose is a good pose to perform when you want to relax and stretch your pelvic floor.
- To begin, contract your knees while lying on the ground.
- Your knees should be 90 degrees bent toward your belly with the soles of your feet pointing up.
- Take grip of your feet’s the inside or the outside.
- Your knees should be somewhat wider than your torso when you open them. After that, lift your feet till they are under your arms. Confirm that your ankles are higher than your knees.
- Angle your heels and firmly put your paws in your hands. You can gently move back and forth or hold this posture for a few breaths.
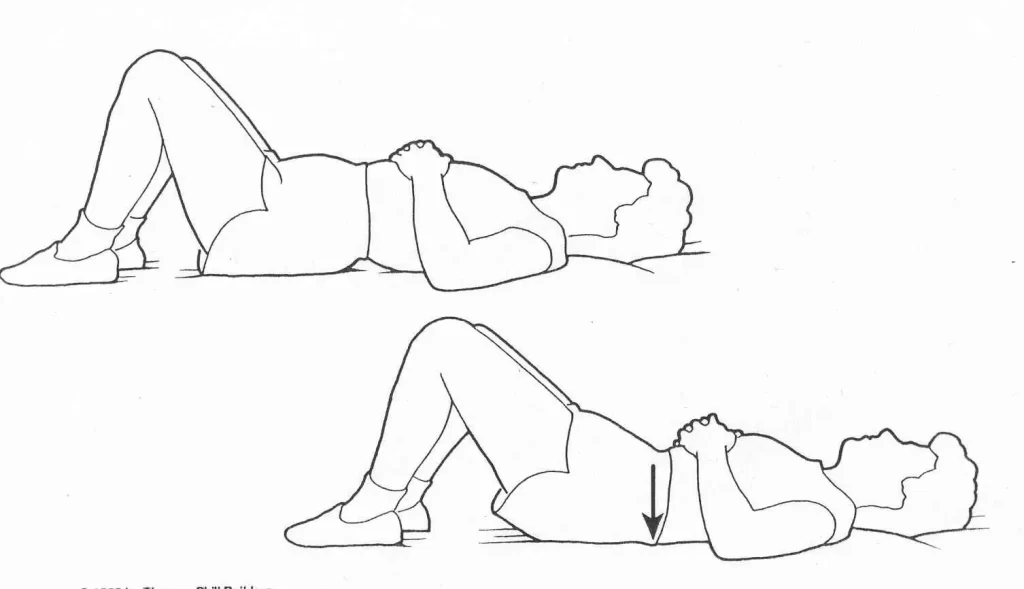
Bridging
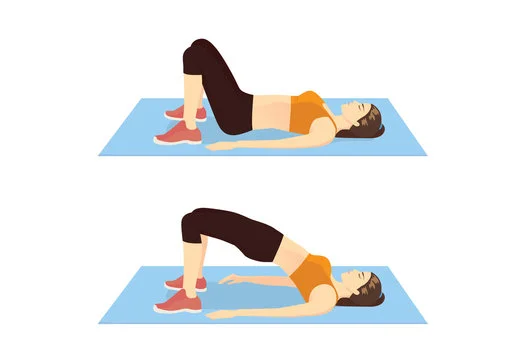
- To carry out this task:
- Angle your knees and lie down in a supine position with both feet flat on the ground. Keep the arms by your sides, while palms facing down.
- To lift your buttocks and pelvic floor muscles a few inches off the ground, flex them together.
- For 3-5 seconds, maintain this posture.
- You should begin to relax your pelvic floor muscles, and your thighs should sink to the ground.
- In a single set, you can do this as many as ten times.
- After taking a break, continue with up to two more sets.
- As their pelvic floor gets stronger, a lot of people find they can do additional repetitions.
Squat

- To do a squat, one must:
- Holding your feet flat on the ground, place them hip-width apart.
- Flex at the knees while bringing your buttocks as close to a surface as possible.
- Hold your back straight and incline slightly forward. The knees and toes have to be in the correct position.
- When you stand back up, concentrate on clenching your pelvic floor and buttocks.
- This exercise can be carried out in up to ten sets of repetitions.
- Before attempting any more sets, have a rest.
What are the precautions for Genitofemoral Neuralgia?
Genitofemoral neuralgia cannot be prevented specifically, however, the risk can be decreased by avoiding situations that could irritate or harm the nerve. The following general safety measures:
- Taking care of underlying diseases: Follow your doctor’s instructions to successfully manage any conditions that impact the nervous system, such as diabetes, multiple sclerosis, or other conditions that affect the nerves.
- Preventing excessive strain: Lifting large amounts of weight or using excessive strain can make the issue worse.
- Pay attention to post-operative care: To reduce nerve discomfort after pelvic or abdominal surgery, make sure you follow your doctor’s recovery instructions.
- Mild exercise: Walking and swimming are two regular, low-impact exercises that can assist preserve flexibility and general health.
Summary
A painful condition known as genitofemoral neuralgia is typically experienced by those who have had lower abdominal surgeries, such as herniorrhaphy. Along the nerve’s distribution, genitofemoral neuralgia’s painful symptoms appear.
The cutaneous distribution of the Genitofemoral nerve(GFN) and other inguinal nerves, particularly the ilioinguinal nerve, overlaps, making accurate diagnosis difficult. Identifying differential diagnoses is a necessary skill for physicians to carry out a successful pain relief strategy.
Both diagnostic and therapy purposes are served by selective nerve blocks. Long-term pain relief can be achieved by nerve excision treatments if targeted nerve blocks prove to be effective.
FAQs
In men, what is the genitofemoral nerve?
The genital branch of the genitofemoral nerve enters the inguinal canal from the deep inguinal ring. The scrotal skin and cremaster in men are supplied by the genital branch.
What causes males to experience pain in the genitofemoral nerve?
Anywhere along the genitofemoral nerve’s route, compression might result in genitofemoral neuralgia. The most typical causes of compression of this nerve are trauma, particularly blunt trauma, and nerve injury from pelvic surgery. Rarely does genitofemoral neuralgia develop on its own.
What signs and symptoms are associated with genitofemoral neuralgia?
Among the symptoms are numbness and searing, sharp, stabbing, or throbbing pain in the belly and between the legs.
How is genitofemoral nerve pain alleviated?
Nonsteroidal anti-inflammatory medications and avoiding physical activity that exacerbates the condition’s symptoms, such as prolonged sitting or squatting, may be the first lines of a cure for genitofemoral neuralgia.
What occurs in the event of injury to the genitofemoral nerve?
Since the nerve controls both sensation and movement, the muscles in front of the abdominal wall weaken if the femoral branch of the genitofemoral branch is impacted.
References
- Genitofemoral nerve. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/genitofemoral-nerve
- Genitofemoral Neuralgia – Pain Spa. (2023, June 27). Pain Spa. https://www.painspa.co.uk/condition/genitofemoral-neuralgia/
- Pain. (2020, July 13). Ilioinguinal or Genitofemoral Neuralgia. Atlanta, GA – Spine Surgery. https://atlantaspineinstitute.com/understanding-pain/ilioinguinal-or-genitofemoral-neuralgia/
- Lpcadmin. (2017c, June 12). Nerve Pain Genitofemoral Neuralgia – Pain Clinic London. London Pain Clinic. https://www.londonpainclinic.com/neuropathic-pain/nerve-pain-genitofemoral-neuralgia/
- Genitofemoral Neuralgia | Dr Vanessa Sammons. (2021, July 8). Dr Vanessa Sammons. https://drvanessasammons.com.au/nerves/pelvis-and-leg-nerves/genitofemoral-neuralgia/
- Cesmebasi, A., Yadav, A., Gielecki, J., Tubbs, R. S., & Loukas, M. (2014). Genitofemoral neuralgia: A review. Clinical Anatomy, 28(1), 128–135. https://doi.org/10.1002/ca.22481