Finger Pain
Finger pain is a prevalent issue that is commonly caused by hand injuries such as fractures, cuts, or broken nails. It can also be a symptom of underlying medical conditions like osteoarthritis, rheumatoid arthritis, and carpal tunnel syndrome.
The pain in fingers can be described as a throbbing, cramp-like, or achy sensation that can affect any finger, including the thumb, usually stemming from an injury or medical ailment.
While most cases of finger pain are not severe and tend to resolve on their own, persistent or unexplained finger pain might signal a more serious medical problem. It is advisable to seek medical attention if you are experiencing ongoing finger pain.
Anatomy of Fingers
The hand comprises a total of 14 phalanges, which are the bones forming the fingers. Each finger consists of three phalanges known as proximal, middle, and distal, with the thumb having two phalanges. These finger segments are commonly identified as the thumb, index finger, middle finger, ring finger, and pinkie finger. The finger bones are labeled based on their proximity to the palm, with the proximal phalanx being closest to the palm, followed by the middle phalanx, and finally the distal phalanx furthest from the hand.
The fingers have three main joints:
- Metacarpophalangeal joint (MCP): Also known as the knuckle, this joint connects the finger bones to the hand bones. The thumb’s MCP joint connects to the trapezium bone.
- Proximal interphalangeal joint (PIP): The proximal and middle phalanges of the finger are connected by this joint.
- Distal interphalangeal joint (DIP): This joint joins the middle and distal phalanges and is next to the fingertip. Unlike the other fingers, the thumb does not have a DIP joint or distal phalanx bone.
These finger joints are encased with a cartilage layer to facilitate smooth movement between the bones. Each joint has a fibrous capsule lined with synovium, a membrane secreting lubricating fluid for joint movement. The thumb possesses unique capabilities such as touching all fingers of the same hand’s tips and a wide range of motion necessary for grasping and holding objects.
Causes of Finger Pain
There are situations when the cause of your finger pain symptoms is unknown. The list of frequent causes provided below can be useful to you in your search for relief. Not all of these factors, though, are self-diagnostic.
Traumatic Finger Pain Causes
Finger pain caused by trauma can stem from various sources. Examples include:
- Bruises and Strains: Accidents like slamming a finger in a door or playing sports can lead to finger injuries.
- Fractures: Despite their strength, finger bones can easily break or fracture. Stress fractures, especially in fingers, may not be immediately noticeable. Symptoms can include swelling, limited hand and finger movement, and difficulty grasping objects.
Infectious Finger Pain Causes
Infections can also be a source of finger pain. Some possibilities are:
- Bacterial Infections: The most common bacterial infection affecting hands is paronychia, typically seen around the fingernails. Any cut on the finger can potentially lead to a painful infection if left untreated.
- Viral Infections: Conditions like herpetic whitlow can cause finger pain, particularly in the fingertip area.
Medical Conditions Contributing to Finger Pain
Several medical conditions can result in finger pain, such as:
- Joint Issues: Arthritis can manifest with finger pain, alongside weakness in the hands.
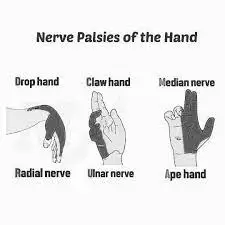
- Nerve Damage: Conditions like carpal tunnel syndrome can cause tingling and discomfort in the fingers due to nerve damage.
- Blood Vessel Trauma: Thoracic outlet syndrome, characterized by compression impeding blood flow to the extremities, can lead to symptoms like finger tingling and numbness.
Rheumatoid Arthritis
Rheumatoid arthritis is a persistent inflammatory condition affecting joint linings, leading to thickening and pain. It can also impact various body parts such as the heart, lungs, eyes, and circulatory system. This disease is autoimmune, where the body’s immune system mistakenly attacks itself for unknown reasons.
The main demographic at risk is women between 30-60 years old, along with factors like family history, smoking, and obesity playing a role. Initial symptoms consist of warm, swollen, stiff, and painful joints, particularly in the fingers and toes, accompanied by fatigue and fever. Usually, the body’s joints on both sides are impacted.
Without treatment, irreversible joint damage and deformities may occur, alongside other complications. Early detection allows for preventive measures to commence promptly. Diagnosis involves physical examinations, blood tests, and imaging scans like X-rays, CT scans, or MRIs.
While there isn’t a cure for rheumatoid arthritis, management strategies can enhance a person’s quality of life. Treatment options include nonsteroidal anti-inflammatory drugs, steroids, anti-rheumatic medications, physical therapy, and sometimes corrective joint surgery.
Raynaud Phenomenon
Raynaud phenomenon, also known as Secondary Raynaud syndrome, causes abnormal constriction of small skin arteries when exposed to cold air or water. This restricts blood flow to the hands, fingers, feet, toes, nose, and ears. Secondary Raynaud syndrome, typically triggered by an underlying medical condition like rheumatoid arthritis, scleroderma, or lupus, is rare.
More prevalent among women living in cold regions, the Raynaud phenomenon presents symptoms like numb and cold hands and feet, with skin color changing from pale to bluish and then red once warmed. Untreated cases may lead to ulcers, finger/toe deformities, and potentially gangrene due to reduced circulation.
Diagnosis involves a patient’s history, physical exams, and blood tests. Treatment consists of medications to improve circulation, addressing underlying conditions, and lifestyle adjustments for enhanced extremity protection in cold conditions.
Psoriatic Arthritis
Psoriatic arthritis, a complication of psoriasis, results in thickened, red, scaly skin. Arthritis might emerge before or after psoriasis develops. Both conditions, stemming from genetic and environmental factors, are autoimmune diseases where the body attacks itself.
Primarily affecting individuals aged 30-50 with a family history of psoriasis, psoriatic arthritis manifests with painful, swollen, and warm joints on one or both sides of the body, finger/toe swelling and deformities, flaking fingernails, and foot discomfort. Seeking treatment is crucial to prevent permanent joint, eye, and heart damage.
Diagnosis involves physical exams, x-rays, and MRIs with blood and joint fluid tests confirming psoriatic arthritis. Treatment includes over-the-counter anti-inflammatory drugs, anti-rheumatic meds, immunosuppressants, and joint steroid injections. Joint replacement surgery may be considered in extreme situations.
Non-Serious Finger Injury
Injuries to the fingers are a common occurrence and usually do not require medical intervention. You can manage these injuries at home by applying ice and allowing the affected finger to rest. If there is swelling and difficulty moving the finger, an X-ray may be necessary to rule out a fracture.
Symptoms and Characteristics:
- Common symptoms include recent finger injury, finger pain from an injury, swollen finger, and severe finger pain.
- Consistently present symptoms of a non-serious finger injury are: new damage to the finger
- Symptoms that are never present in non-serious finger injuries include: a twisted or bent finger
- Urgency level: Self-treatment
Nail Infection (Paronychia)
Paronychia is an infection that affects the skin around the fingers or toes, specifically where the skin meets the nail. Acute paronychia, characterized by sudden onset, is typically caused by the staphylococcus bacteria. On the other hand, chronic paronychia is often a result of a fungal infection, particularly common in individuals who frequently have wet hands due to their line of work.
Those with diabetes or compromised immune systems are at a higher risk of developing nail infections. Symptoms may include sore, reddened, and swollen skin around the nail, sometimes accompanied by pus. Diagnosis involves a physical examination and occasionally a skin culture to identify the infecting organism.
Treatment:
- Acute paronychia: Treatment involves having a healthcare professional clean any wounds, drain infections if needed, and prescribe antibiotics if necessary.
- Chronic paronychia: Management includes ensuring the affected skin stays dry and using antifungal medications on the affected nail.
Symptoms and Characteristics:
- Top symptoms include swollen, painful, and spontaneously occurring fingers and nails.
- Urgency level: Phone call or in-person visit
Mallet Finger
Mallet finger is an injury to the tendon at the furthest knuckle of the finger, resulting in the inability to straighten the tip of the finger. Seeking medical attention from a primary care physician or visiting an urgent care clinic within 24 hours is essential.
Diagnosis typically involves X-rays to assess the severity of the injury, and treatment consists of splinting. In cases where the bone is protruding through the skin, immediate emergency room care is necessary.
Jammed Finger
Jammed fingers, often associated with sports activities but also possible during everyday tasks, require evaluation by a physician or at an urgent care facility within the next day. In most instances, surgery is not needed, and splinting the finger is sufficient.
Symptoms and Characteristics:
- Top symptoms: finger bruise, finger joint stiffness, swollen finger, finger discomfort following an injury, and recent finger injury
- Symptoms that always occur with a jammed finger: recent finger injury, finger pain from an injury
- Urgency level: Primary care doctor
Dislocated Finger
Dislocations at the finger’s base are uncommon but can damage the finger’s blood supply and nerves. Immediate care is necessary, and seeking treatment at an urgent care facility or emergency room is advised. A physician can safely “reduce” – realign the finger back into place.
Simple dislocations typically require buddy taping to an adjacent finger, while more complex fractures necessitate immobilization with a splint. After the reduction, monitoring the blood flow to the fingertip is crucial. If the finger cannot be reduced, consultation with a hand surgeon is recommended.
Boxer’s fracture
- Boxer’s fracture is the term used to describe a fracture in one of the fingers, often resulting from a closed fist striking a hard object.
- To alleviate pain and swelling, apply ice. If there is an open wound, clean it gently with soap and water before seeking care at your nearest urgent care clinic.
- Symptoms of a boxer’s fracture include finger pain, swelling, and a history of a forceful impact on the finger.
- If you notice your finger is misshapen, it is important to have it examined through an x-ray. Trying to realign it on your own is not recommended.
- In cases where a finger appears bent or crooked, seeking attention at a hospital emergency room is necessary to address the issue promptly.
Identifying Different Types of Finger Pain
Finger discomfort can manifest as a dull, achy sensation or as a sharp, cramp-like pain, sometimes starting suddenly and then subsiding.
Accompanied by swelling, a broken finger typically appears swollen, purple, or bruised, and causes intense pain. Occasionally, the bone might even be visibly dislocated underneath the skin.
Throbbing or movement-induced pain can be indicative of conditions like carpal tunnel syndrome, affecting nerves and muscles in the hand and arm. Symptoms might include throbbing pain in the fingers, discomfort when moving the affected areas, difficulty with typing or writing, and hand tremors.
Sharp shooting pain may occur from a finger dislocation, where the bones become dislocated from their joints, sometimes visibly. This type of injury can also lead to throbbing or sharp pain.
In cases of a finger cut, pain localized to the site of injury might extend to surrounding areas based on the severity of the cut.
Discomfort accompanied by lumps in the hand could indicate the presence of growths like boils or nodules. This may be experienced alongside typical finger pain, presenting as a fluid-filled lump, a firm patch of skin, a movable lump under the skin’s surface, or a tender lump upon touch.
Symptoms of Finger Pain
Finger pain may be associated with various other symptoms. For instance, infections in the finger could extend to the bloodstream, triggering fevers, inflammation, and shivering.
Additional symptoms that might coincide with finger pain can encompass:
- Discomfort in the arm or wrist
- Areas with bruising
- Changes in skin color
- Weakened grip
- Presence of discharge or pus
- Issues with fingernails, such as bruising beneath the nail or nail detachment
- Flu-like manifestations
- Cuts, ulcers, lesions, or scrapes
- Bumps on the finger
- Limitation in joint movement range
- Rigidity
- Swollen regions
- A sensation of numbness”
When to Seek Medical Attention
If your finger pain persists for more than a week without a known injury, it is advisable to contact a healthcare provider. Finger pain and swelling can be indicative of underlying conditions that require attention.
Certain signs and symptoms should prompt a visit to a healthcare provider, including:
- Pain that significantly hinders fine motor movements
- Inability to move fingers without pain
- Red, hot, or swollen fingers
- Loss of sensation in the finger
- Presence of symptoms like fever, fatigue, or unexplained weight loss alongside the pain.
Diagnosis
Your healthcare provider will conduct a physical examination and inquire about your medical background, specifically how and when your finger pain symptoms emerged, to identify the source of your discomfort.
Imaging or blood tests may be recommended by your healthcare provider to aid in the diagnostic process.
Medical Background
In the initial assessment, your healthcare provider will review your medical history, focusing on any existing medical conditions and the onset of your finger pain.
Furthermore, your healthcare provider will pose queries regarding your symptoms, such as:
- Are you experiencing tingling, numbness, swelling, burning sensation, or muscle weakness?
- Has the pain intensified over time?
- Does the pain occur at rest or specifically when you perform certain actions or move your fingers?
- Have you suffered any prior injuries to your hand or fingers?
Inform your healthcare provider if you have recently dealt with an infection or are experiencing symptoms like fever, fatigue, or unexplained weight loss, as these could indicate an underlying systemic condition contributing to your finger pain.
Physical Examination
A physical examination will be conducted by your healthcare provider to assess the condition of your hands and fingers, as well as to check for any limitations in the movement or signs of pain in your finger joints.
During the examination, signs of the following will be observed:
- Redness
- Warmth
- Swelling
- Tenderness
- Bruising
- Numbness
- Abnormal skin texture
Blood Tests
Suppose conditions such as gout, autoimmune disorders like rheumatoid arthritis, psoriatic arthritis, lupus, scleroderma, or an infection are suspected. In that case, blood tests will likely be recommended by your healthcare provider to aid in the diagnosis.
Blood tests can help determine the diagnosis by measuring levels of uric acid, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), rheumatoid factor, and antinuclear antibodies, among others.
Imaging
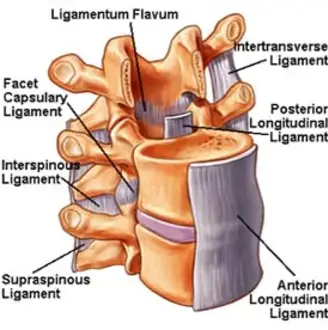
Various imaging techniques are commonly used to examine your finger joints, evaluate joint alignment, and identify indications of damage or inflammation. X-rays are usually the first choice to detect arthritis or fractures, while a magnetic resonance imaging (MRI) test may be conducted to assess a sprain or tear in cases of suspected tendon or ligament injuries.
Joint Aspiration
When a joint infection or conditions like gout are suspected, joint aspiration may be performed by your healthcare provider. This procedure involves extracting fluid from your finger joints for testing for any irregularities.
Nerve Conduction Study
In cases where nerve compression or damage is believed to be the cause of your finger pain, a nerve conduction test may be conducted to assess the nerve functionality. This test involves the application of electrodes on your skin and administering small electrical shocks to measure the speed of signal transmission in your nerves, thereby evaluating nerve function.
Home Remedies for Finger Pain
If you believe a visit to the doctor is unnecessary for treating your finger pain, there are various home remedies you can attempt.
Remedies to Try at Home:
- R.I.C.E. Method: If your finger pain is not severe, follow the R.I.C.E. method – rest, ice, compression, and elevation. Rest your finger as much as possible, apply ice several times a day, compress it gently, and elevate it when at rest.
- Buddy Taping: Secure your injured finger to a healthy adjacent finger using stiff tape that prevents movement. This technique acts as a makeshift splint, keeping your injured finger stable during the healing process, particularly beneficial for minor fractures and sprains.
- Pain Relief Medication: Over-the-counter pain relievers like ibuprofen, naproxen, or aspirin can help alleviate swelling and discomfort if taken as directed.
- Epsom Salt Soak: To relieve general pain, consider soaking your finger in a bowl of Epsom salt. This method can help relax stiff joints and soothe muscle discomfort effectively.
Treatment Options for Finger Pain
The treatment options for finger pain will differ based on the root cause and severity of your symptoms. While many cases of finger pain can be effectively managed with medication and self-care techniques, more severe or chronic injuries may necessitate surgical intervention.
Lifestyle Treatments
Certain home remedies can aid in alleviating finger pain, including:
- Applying topical pain relief creams or gels
- Using ice or heat for pain relief
- Engaging in gentle finger and wrist stretching exercises
- Taking a break from activities that involve grasping or gripping
- Using splints or immobilizers for added support during the healing process
- Implementing adaptive equipment and modifications to reduce stress on finger joints
- Making dietary adjustments, such as avoiding shellfish and alcohol in cases of gout
- Avoiding exposure to cold temperatures if you have Raynaud’s syndrome
Medications
Depending on the level of pain experienced, medication may be necessary to manage symptoms. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) or stronger prescription opioids can be taken orally. Steroids may also be injected directly into the finger joints to reduce inflammation.
For individuals with systemic or autoimmune conditions, healthcare providers may prescribe medications like colchicine or allopurinol for gout, antibiotics for infections, or disease-modifying antirheumatic drugs (DMARDs) for autoimmune conditions. Iontophoresis, a method that delivers dexamethasone through the skin via electrical stimulation, can also be used to alleviate pain.
Surgery
In cases of significant finger injuries or deformities causing persistent pain and impaired hand and finger function, surgery may be necessary to improve joint alignment. Surgery is usually considered a last resort after attempting other treatment options. However, for severe finger fractures, immediate surgery may be required to stabilize and realign joints.
Surgical procedures can also address chronic conditions like carpal tunnel syndrome or de Quervain’s tenosynovitis. Releasing the wrist or thumb retinaculum during surgery can reduce compression on inflamed tendons, alleviating pain and associated symptoms.
Physical Therapy for Finger Pain
Benefits of Physical Therapy
Physical therapy provides numerous valuable benefits for individuals with finger pain. Here are some key advantages of integrating physical therapy into the treatment plan for this condition:
- Non-Surgical Approach: Physical therapy offers a non-invasive and conservative option for treating finger pain, making it ideal for those seeking to avoid surgery or invasive procedures.
- Pain Management: Physical therapists utilize various techniques and exercises to reduce pain and discomfort related to finger pain. These methods may include manual therapy, stretching, and modalities like ultrasound or heat therapy.
- Enhanced Range of Motion: The goal of physical therapy is to improve joint function and flexibility in the affected finger or thumb. By working on increasing the range of motion, patients can move their digits more easily and without pain.
- Muscle Strengthening: Specific exercises target the hand and forearm muscles to enhance strength and stability. Stronger muscles offer better support to the affected finger, reducing the risk of further complications.
- Personalized Treatment Plans: Physical therapists create tailored treatment plans based on the individual’s condition and requirements. This personalized approach ensures that therapy addresses the specific challenges presented by the finger pain.
- Prevention of Future Problems: In addition to treating current symptoms, physical therapy focuses on preventing future issues. Therapists emphasize techniques to maintain hand health and lower the chance of trigger finger recurring.
- Improved Quality of Life: As symptoms improve and function is restored, individuals benefit from an overall enhancement in their quality of life. This allows for easier performance of daily activities and work-related tasks.
- Patient-Centered Approach: Close collaboration between physical therapists and patients ensures progress is monitored and treatment plans are adjusted accordingly. This patient-centered approach guarantees that therapy remains effective throughout the recovery journey.
Physical Therapy Exercises for Fingers
Passive Range of Motion (PROM) Exercises
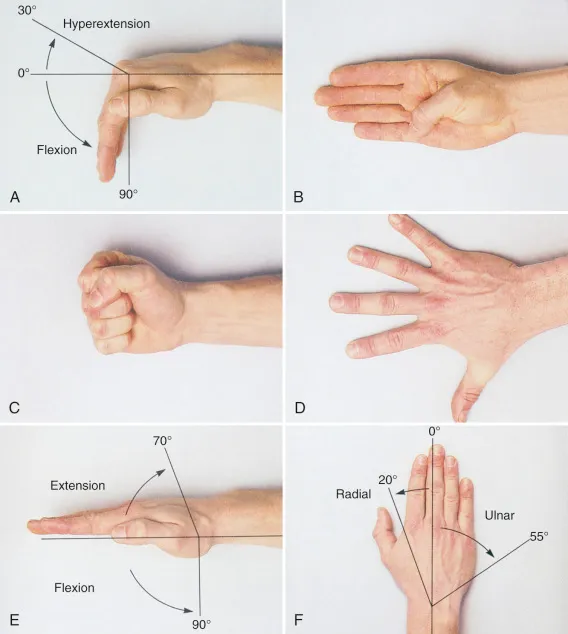
These exercises involve the physical therapist gently moving the finger through its full range of motion to improve mobility and flexibility.
- Finger Flexion: The therapist will hold the patient’s hand and gently bend the affected finger towards the palm, moving it through the full range of flexion.
- Finger Extension: The therapist will hold the finger and gently straighten it, moving it through the full range of extension.
- Abduction/Adduction: The therapist will spread the fingers apart (abduction) and bring them back together (adduction), working on the full range of motion for each finger.
- Circumduction: The therapist will move the finger in a circular motion, rotating it through its full range of motion in all directions.
Active Range of Motion (AROM) Exercises:
These exercises involve the patient actively moving the affected finger(s) through their full range of motion without assistance.
- Finger Flexion/Extension: The patient will bend and straighten each finger, one at a time, moving through the full range of motion.
- Finger Abduction/Adduction: The patient will spread the fingers apart and bring them back together, focusing on moving each finger individually.
- Finger Circles: The patient will make circular motions with each finger, rotating them in both clockwise and counterclockwise directions.
- Finger Oppositions: The patient will touch the tip of each finger to the tip of the thumb, working on the full range of motion for each digit.
Strengthening Exercises
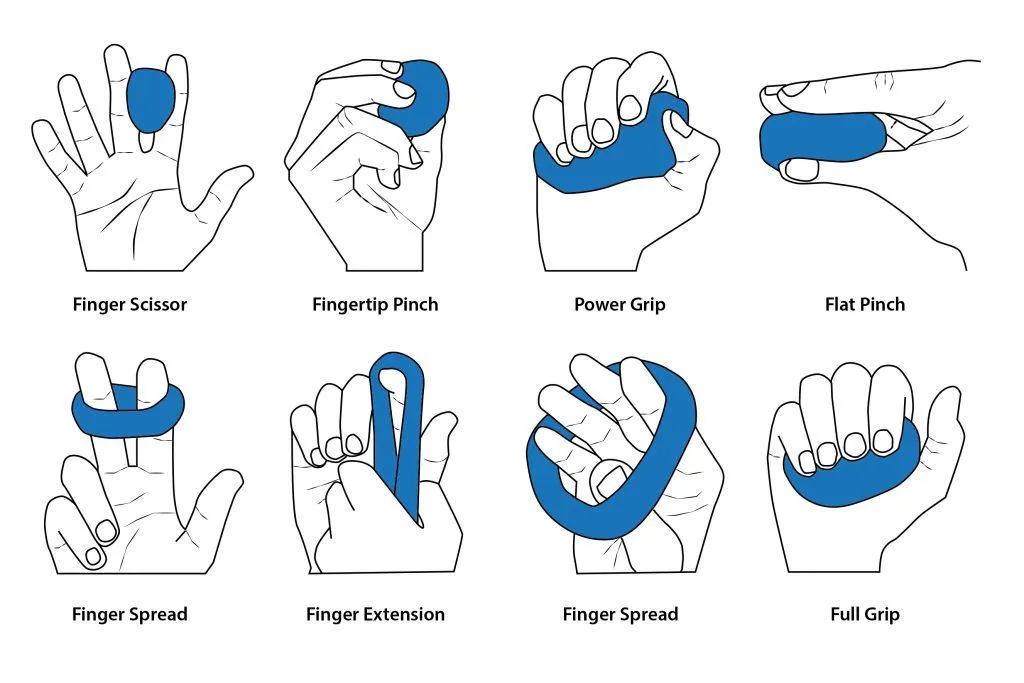
Finger Grip Strengthening:
- Squeeze a soft rubber ball or stress ball with the affected hand/fingers
- Perform repetitions of squeezing and releasing
- Gradually increase resistance by using a firmer ball or adding putty/therapy clay
Finger Abduction/Adduction:
- Place a rubber band around the fingers, creating resistance
- Spread the fingers apart (abduction) against the resistance of the band
- Bring the fingers back together (adduction)
- Repeat for the desired number of repetitions
Finger Extension:
- Place a rubber band around the fingertips
- Straighten the fingers against the resistance of the band
- Hold for a few seconds, then release
- Repeat for the desired number of repetitions
Wrist Curls:
- Hold a lightweight dumbbell or a soup can in the affected hand
- Rest the forearm on a table, with the wrist hanging off the edge
- Curl the wrist upward, then downward, bending at the wrist joint
- Repeat for the desired number of repetitions
Finger Ladder:
- Use a finger ladder or a similar device with rungs or loops
- Insert the fingers into the rungs or loops
- Perform finger flexion and extension by straightening and curling the fingers
- Progress to using smaller rungs or loops for increased resistance
Putty/Therapy Clay Exercises:
- Squeeze and release a ball of putty or therapy clay with the affected hand/fingers
- Knead and roll the putty, working the muscles of the hand and fingers
- Gradually increase the resistance by using a firmer putty or clay
Resistance Band Exercises:
- Fasten a resistance band to a steady surface.
- Loop the band around the fingers or hand
- Perform exercises such as finger flexion, extension, abduction, and adduction against the resistance of the band
The physical therapist may also incorporate the use of specialized hand exercisers or other resistance devices to target specific muscle groups and movements. They will guide the appropriate resistance level, number of repetitions, and sets based on the individual’s condition and goals.
Prevention
Swollen and achy joints in the fingers may indicate various systemic and autoimmune conditions. Maintaining optimal overall health and embracing an anti-inflammatory lifestyle can help prevent or reduce the severity of symptoms.
Habits that support an anti-inflammatory lifestyle include:
- Following a nutritious and balanced diet
- Making sure you consistently receive seven to eight hours of good sleep
- Effectively managing stress levels
- Seeking strong social support from loved ones
- Minimizing exposure to harmful toxins and chemicals
Additionally, taking care of your fingers and hands can aid in preventing injuries. This involves minimizing repetitive hand and wrist movements whenever possible and giving your fingers a break from activities that cause discomfort.
Summary
- Various factors can lead to finger discomfort, such as osteoarthritis, rheumatoid arthritis, gout, fractures, and sprains, among others.
- While certain finger pain causes can be managed with home remedies like ice packs, heat packs, or over-the-counter medications, more severe or persistent pain may necessitate broader treatment methods to reduce inflammation across the body.
- Minimizing repetitive strain on hands and fingers, and taking breaks from activities that exacerbate discomfort, particularly if fingers are already painful, can aid in preventing symptoms from emerging or worsening.
FAQs
What are the most common causes of finger pain?
The most common causes of finger pain include injuries (such as sprains, fractures, or dislocations), arthritis (osteoarthritis, rheumatoid arthritis, or psoriatic arthritis), tendinitis (like trigger finger or de Quervain’s tenosynovitis), nerve compression (carpal tunnel syndrome or cubital tunnel syndrome), infections (paronychia or felon), autoimmune diseases (lupus or scleroderma), repetitive strain injuries, Raynaud’s phenomenon, and gout.
How can I tell if my finger pain is serious or not?
Seek medical attention if you experience severe or persistent pain, significant swelling or deformity, inability to move the finger, signs of infection (redness, warmth, fever), numbness or tingling, or if the pain interferes with your daily activities. These signs could point to a more serious underlying illness that needs to be evaluated and treated right away.
What are the best ways to manage finger pain at home?
Home care strategies for finger pain include resting and immobilizing the affected finger(s), applying cold or heat therapy, keeping the hand elevated, taking over-the-counter pain relievers or anti-inflammatory medications, performing gentle exercises and stretches, using ergonomic modifications, practicing self-massage, managing stress, making lifestyle adjustments, and using supportive aids like splints or grip aids.
When is physical therapy recommended for finger pain?
Physical therapy is often recommended for finger pain caused by conditions like arthritis, tendinitis, nerve compression syndromes, or injuries. Physical therapists can provide pain management techniques, range-of-motion exercises, strengthening exercises, joint mobilization, splinting, ergonomic education, and customized home exercise programs to promote healing and restore function.
What types of medications are used to treat finger pain?
Medications commonly used to treat finger pain include over-the-counter pain relievers (acetaminophen, ibuprofen, naproxen), prescription-strength non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, disease-modifying antirheumatic drugs (DMARDs) for autoimmune conditions, and topical analgesics or anti-inflammatory creams or ointments.
When is surgery necessary for finger pain?
Surgery may be recommended for severe cases of finger pain or when conservative treatments have been ineffective. Surgical procedures include arthrodesis (joint fusion), arthroplasty (joint replacement), tendon repair or reconstruction, nerve decompression, or drainage or debridement of infections.
Can finger pain be prevented?
While some causes of finger pain may be unavoidable, there are preventive measures you can take, such as proper warm-up and cool-down exercises, maintaining good posture and ergonomics, taking breaks and stretching during repetitive tasks, using appropriate protective equipment, and managing underlying conditions like diabetes or arthritis.
How can I cope with chronic finger pain?
Coping with chronic finger pain involves developing healthy coping mechanisms (deep breathing, meditation, mindfulness), modifying activities and tasks to reduce strain, using assistive devices and adaptive equipment, engaging in regular exercise and physical therapy, managing medications properly, and seeking support through counseling or support groups.
References
Maday, R. (2018, March 26). Finger Pain | Possible Causes, Arthritis, & Treatment | Buoy. https://www.buoyhealth.com/learn/finger-pain
Dpt, K. G. P. (2022, December 12). Causes of Finger Pain and Treatment Options. Verywell Health. https://www.verywellhealth.com/finger-pain-6373927
Kahn, A. (2023, March 1). Understanding Finger Pain. Healthline. https://www.healthline.com/health/finger-pain#treatment
The Role of Physical Therapy in Managing Trigger Finger. (2023, September 14). Online Physiotherapy | Best Physiotherapists | PhysioMantra. https://physiomantra.co/physical-therapy/physical-therapy-for-trigger-finger/
Parmar, D. (2023, December 20). Finger Pain Cure: Causes, Symptoms, Treatments. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/finger-pain/