Femoral Nerve
Introduction
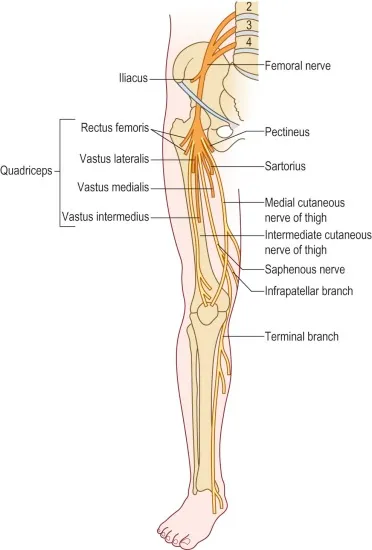
The femoral nerve is a major peripheral nerve of the lower limb, originating from the lumbar plexus (L2-L4). It supplies motor innervation to the anterior thigh muscles (e.g., quadriceps) responsible for knee extension and hip flexion, and provides sensory innervation to the anterior thigh and medial leg via the saphenous nerve. It plays a crucial role in walking, standing, and maintaining balance.
The lateral circumflex femoral artery separates the anterior and posterior segments of the femoral nerve.
Structure
In the Abdomen
The psoas major muscle is where the femoral nerve starts its journey through the abdomen. After there, it travels laterally to the psoas major muscle distal portion before being “sandwiched” between the iliacus and psoas major muscles. The psoas major muscle is situated above the femoral nerve, whereas the iliacus muscle is situated under it.
The femoral nerve supplies the iliacus muscle. Because the psoas major muscle is located medial to the union of the ventral rami to form the femoral nerve, the psoas major is innervated by the ventral between L2 and L4. The thigh may flex at the hip thanks to these muscles. Weakness of the iliopsoas leads to difficulty in flexing the thigh to go upstairs.
In the Pelvis
After that, the femoral nerve enters the thigh. It must travel beneath the inguinal ligament to reach the femoral triangle. The femoral triangle is made up of the superior inguinal ligament, the medial adductor longus, and the lateral sartorius. From lateral to medial, NAVEL serves as a memory aid to help recall the structures’ sequence. EL stands for space with lymphatics (femoral canal with lymph node of Cloquet); N, A, and V stand for femoral nerve, artery, and vein, respectively. The lateral femoral cutaneous artery separates the two femoral nerve divisions, making them easily identifiable.
Anterior Division
Additionally, these muscles aid in hip flexion of the thigh.
The anteromedial sensory innervation of the thigh is caused by these nerves working together.
Posterior Division
The greatest cutaneous branch of the femoral nerve is the sensory nerve, also known as the saphenous nerve. The femoral nerve changes into the saphenous nerve via the adductor canal. Up until around halfway down the tibia, it keeps moving along the medial portion of the tibia before splitting into two branches. The opposite branch, which is more anterior, ends at the hallux after continuing down the foot’s medial surface.
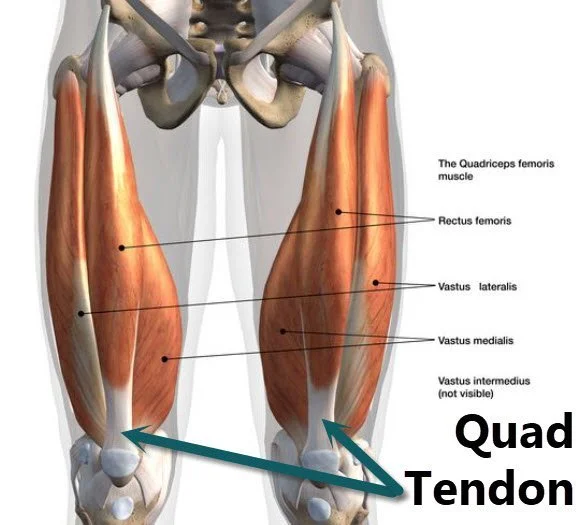
Together, these muscles make up the quadriceps femoris, which is the main extensor of the leg at the knee.
According to Hilton’s law, the articular nerves innervate the joints’ synovial membranes, ligaments, and fibrous capsules. The English surgeon Dr. John Hilton is credited with naming Hilton’s law after he observed that the nerve that innervates the muscles acting on a joint also innervates the joint and frequently the skin covering it.
Function
Motor Functions
The pectineus helps in the thigh’s medial rotation by flexing and adducting it.
The iliacus muscle works in tandem with the psoas major and minor to produce the iliopsoas, which flexes and stabilizes the thigh at the hip joint.
The sartorius muscle stretches the leg at the knee.
Knee extensors:
Additionally, the rectus femoris stabilizes the hip joint and helps the iliopsoas flex the thigh.
Course
The greatest branch of the lumbar plexus is the femoral nerve. It gives the front thigh muscles motor innervation and originates from the posterior cords of the lumbar plexus (L2-L4). The obturator nerve, on the other hand, nourishes the medial compartment of the thigh and originates from the anterior cords (L2-L4).
The femoral nerve emerges at the lower lateral edge of the psoas major. It passes lateral to the femoral artery and vein and passes beneath the midway of the inguinal ligament, entering the femoral triangle.
You can use the mnemonic NAVY to recall the content order of the femoral triangle, from lateral to medial:
- Nerve
- Artery
- Vein
- lymphatics (femoral canal)
It splits into an anterior (superficial) and a posterior (deep) division after passing beneath the inguinal ligament. The anterior division gives branches to the sartorius muscle and divides into the medial and intermediate cutaneous nerves of the thigh. The quadriceps femoris muscle is supplied by the posterior division. In the leg’s gaiter area, the femoral nerve ends as the saphenous nerve.
Muscle supply
Psoas major -At the hip, the primary thigh flexor. It helps keep the body in an upright position when standing. It emerges from the T12-L5 vertebrae laterally. It attaches to the femur’s lesser trochanter together with the iliacus.
Iliacus – At the hip is another major thigh flexor. It emerges from the sacrum as well as the iliac fossa and crest. It attaches to the femur’s lesser trochanter together with the psoas major.
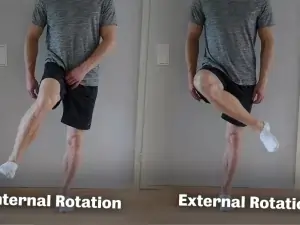
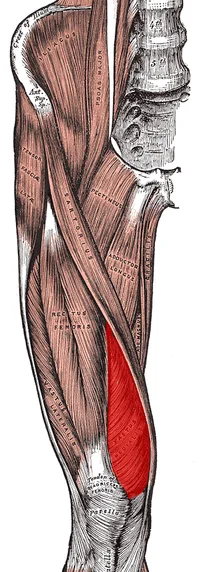
Sartorius -The thigh is laterally rotated at the hip, flexed, and abducted. Additionally, it can medially rotate and bend the leg at the knee. Additionally, it can bend the leg at the knee. The anterior superior iliac spine gives birth to the sartorius. It attaches to the tibia’s medial surface. The pes anserinus (Latin: goose’s foot) is formed at the insertion of the sartorius tendon, which combines with the gracilis and semitendinosus tendons. A web connects the three toes of a goose’s foot. The word “sartorius” comes from the Latin word “sartor,” which means “tailor.” With their leg flexed at the knee and their thigh abducted and medially rotated at the hip, tailors sit on the floor.
Pectineus -Flexes and adducts the thigh at the hip. It originates from the pubic bone’s superior ramus. It enters into the femur’s pectineal line. The muscle’s parallel fibers at its insertion resemble a comb’s teeth, thus the Latin word pecten, which means “comb.”
Branches
Motor branches
Several motor branches are produced by the femoral nerve:
- The iliacus muscle is supplied by the first, which are little branches that emerge in the belly.
- The pectineus, a little muscle in the medial compartment of the thigh, is innervated by the nerve to the pectineus, which splits off the medial aspect of the femoral nerve near the inguinal ligament.
- The anterior division of the femoral nerve gives rise to the sartorius nerve, which supplies the sartorius muscle, also known as the tailor’s muscle.
- The four heads of the quadriceps femoris—the vastus medialis, vastus lateralis, vastus intermedius, and rectus femoris—are supplied by the muscular branches that emerge from the posterior division.
Sensory branches
The medial and intermediate femoral cutaneous nerves of the thigh are produced from the anterior division of the femoral nerve. The skin across the anterior and medial regions of the thigh is sensed by these nerves.
The longest nerve in the body is the saphenous nerve, which produces the femoral nerve’s terminal branch. Together with the femoral vessels, it descends into the adductor canal. The nerve does not, however, pass through the adductor hiatus. To provide sensation to the skin above the greater saphenous vein in the gaiter area, it instead exits on the medial side of the knee.
The femoral nerve supplies articular branches that innervate the hip and knee joint capsules and enable proprioceptive feedback regarding the joints in addition to providing cutaneous innervation.
Examination
The Femoral Nerve Tension Test
To screen for sensitivity to stretch soft tissue in the dorsal part of the leg, which may be associated with nerve root impingements, the Femoral Nerve Tension Test, also called the Femoral Nerve Stretch Test (FNST), is utilized.
The therapist stands on the side that is affected and uses one hand to stabilize the pelvis to avoid anterior rotation while the patient is lying prone. The therapist then flexes the knee to its maximum range using the opposite hand. The therapist continues to stretch the hip while keeping the knee flexed if no encouraging signals are observed in this posture. To determine which nerve is affected, the therapist might make a few changes to the test posture. While the Saphenous Nerve bias test involves prone-lying hip extension, abduction, and external rotation with knee flexion, ankle dorsiflexion, and eversion, the Lateral Femoral Cutaneous Nerve bias test involves prone laying with passive hip extension, adduction, and knee flexion.
The typical reaction is knee flexion, which permits the heel to contact the buttocks. The quadriceps feel stretched or pulled.
The test is deemed successful if unilateral pain is felt in the posterior thigh, buttocks, or lumbar region between 80 and 100 degrees of knee flexion in any combination of these areas. Positive results in this range may indicate a disc herniation impacting the L2, L3, or L4 nerve root because the dura is tensioned between 80 and 100 degrees. Based on the spectrum of pain reproduction, positive findings owing to a disc herniation can be distinguished from quadriceps issues. Injury or tight quadriceps may be the source of discomfort that appears before the knee flexes to 80 degrees. Additionally, when the hip flexes in reaction to passive knee flexion, the pelvis elevates on that side if there is tightness. It is crucial to do the test on both sides and compare the symptoms a since tight rectus femoris can also cause pain in the anterior thigh.
Electromyography can be used to capture muscle electrical activity and assess nerve function. Tests of nerve conduction velocity quantify the speed at which electrical impulses pass through nerves.
Additional tests: Trauma, hematoma, and other relevant variables can be diagnosed with the use of Conditions affecting the muscles and nerves can be diagnosed and treated with neuromuscular ultrasonography. It can assist in detecting alterations in the form of the nerve.
Additionally, medical specialists could suggest an MRI or CT scan, which creates pictures of the interior organs.
Clinical Importance
Radiculopathy and Loss of Reflexes
Irritation or inflammation of a nerve root causes radiating pain. Usually, disc herniation is the cause of this. Pain that goes dermatomally is one of the symptoms. Disc herniations can result in both sensory and motor impairments. Since reflexes include an afferent and an efferent limb, which are impacted in radicular pain, a disc herniation on the L4 spinal nerve root can also cause a person to lose their patellar reflex.
Femoral Hernia
Femoral hernias occur more frequently in elderly women but are less prevalent than inguinal hernias. They are outgrowths of the contents of the abdomen caused by a weakening of the femoral canal. If left untreated, they can cause strangulation and necrosis of the stomach contents in addition to creating a bulge in the groin area. The femoral vein will be situated lateral to the hernia sac as it is situated in the femoral canal.
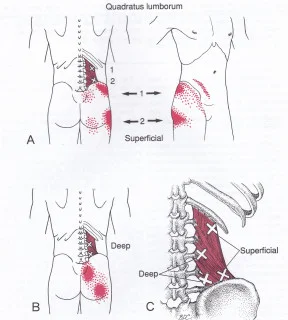
Psoas Abscess/Hematoma
Any infection or hematoma might cause mass effect injury around the psoas or iliacus muscles. The femoral nerve may start to be compressed by the expanding abscess or hematoma because of the connection between these muscles and the nerve. This may result in nerve damage, which might impact the femoral nerve’s motor or sensory innervation.
Femoral and Saphenous Nerve Blocks
Because they avoid the negative effects and addictive qualities of opioids, femoral nerve blocks are frequently used to treat hip pain in individuals who have had hip fractures. To relieve hip discomfort, the pericapsular nerve group (PENG) inhibits certain articular branches of the femoral nerve.
Femoral Nerve Damage
- Sharp, direct trauma is the most frequent cause.
- Hemostases and tumors are examples of compressive aetiologies that can cause ischemia-induced nerve injury.
- Prolonged compression, retraction, or stretching of the nerve has been known to cause iatrogenic damage after hip and intraabdominal surgery.
- Femoral IM nailing, which involves the implantation of proximal interlocking screws, may increase the risk of femoral nerve iatrogenic damage.
- Femoral nerve neuropathy is rare, however it has been documented in cases of complicated anterior and posterior spinal surgery.
Because the iliacus and pectineus muscles are involved, patients will clinically have quadriceps atrophy, loss of knee extension, and to a lesser extent, hip flexion. Because the anterior and medial cutaneous nerves of the thigh are involved, there will be a loss of feeling over the anterior and medial thigh on the sensory side. Additionally, the involvement of the saphenous nerve will result in a loss of sensation over the medial aspect of the lower leg and foot. While the majority of cases have a fair prognosis, some require nerve grafting or repair, and others result in long-lasting residual neurologic impairments.
Obstetric Patients Having Vaginal Delivery with Femoral Neuropathy
During vaginal birth, femoral neuropathies may develop. Patients are frequently placed in the dorsal lithotomy position, which involves flexing the leg at the knee and the thigh at the hip. The blood supply to the femoral nerve is compromised in this posture because it is compressed against the inguinal ligament. Because the quadriceps femoris muscle no longer receives innervation from the femoral nerve, the patient tries to stand after delivery but collapses to the ground. The patella is where the quadriceps femoris muscle attaches.
The tibial tuberosity is where the patellar ligament is attached. The quadriceps femoris muscle extends the leg at the knee when it contracts. To keep the leg from buckling, this motion is essential. Therefore, one must be prepared to catch the patient if she falls owing to femoral neuropathy if they are helping her get off a gurney after delivery.
Patients who exhibit symptoms and indicators of femoral neuropathy show an intriguing variety. They do, however, also exhibit other symptoms that show this is not a real femoral neuropathy. For instance, the patient seems to have both a foot drop and femoral neuropathy. The occurrence of foot drop suggests that the patient has a lumbosacral plexopathy rather than a genuine femoral neuropathy. A challenging delivery is also linked to this disease.
Surgery for Patella Fractures Can Cause Femoral Neuropathy
Femoral neuropathy may result after surgically repairing a patellar fracture.
Testing the Femoral Nerve
The following method can be used to test the femoral nerve. The posture of the patient is prone. The examiner elevates the leg while it is flexed at the knee (Reverse Lasegue test). The femoral nerve is stretched when the hip is hyperextended while the leg is bent at the knee, resulting in discomfort.
Testing the Patellar Tendon Reflex
The quadriceps femoris muscle contracts reflexively when the patellar tendon is tapped with a reflex hammer to test the patellar tendon reflex. The femoral nerve and the L2-L4 ventral main rami are involved in this reflex. Tapping the patellar tendon stimulates the quadriceps femoris muscle spindle fibers. Because they are innervated by the femoral nerve, they activate sensory axons from L2 to L4 that have their cell bodies in the dorsal root ganglia. The dorsal roots allow the central processes of the dorsal root ganglion cells to reach the spinal cord, where they subsequently go to the ventral horn’s alpha-motor neurons. The quadriceps femoris muscle contracts in response to stimulation of these neurons, whose axons are found in the femoral nerve. The quadriceps femoris muscle’s tone is maintained via this reflex. Neurons from higher influences can regulate the activity in this circuit.
Reasons for performing a patellar tendon reflex
Decreased Patellar Tendon Reflex: There are several types of diseases affecting the lower motor neurons that link the quadriceps femoris muscle to the ventral horn of the spinal cord. For instance, the virus that causes poliomyelitis targets and destroys the spinal cord’s alpha-motor neurons. The quadriceps femoris muscle and other lower limb muscles may become paralyzed or die as a result. A lower motor neuron syndrome is the outcome in this instance. Reduced or nonexistent patellar tendon reflexes (hyporeflexia) are caused by damage to the femoral nerve (femoral neuropathy), which can result from a variety of conditions, including spinal cord injuries, poliomyelitis, and trauma.
Increased patellar tendon reflexes: may be observed in strokes and other cerebrovascular events. Here, there is damage or destruction to the neurons that are part of the pathway from the motor cortex to the corticospinal tracts to the alpha-motor neurons. This results in either outright paralysis (plegia) or weakening (paresis). Furthermore, suppressor fibers connect the alpha-motor neurons to the lateral corticospinal tracts. The patellar tendon reflex is suppressed by these neurons. Hyperreflexia (increased deep tendon reflexes) is a result of the loss of suppressor neurons in the brain following a stroke or trauma.
Femoral nerve damage
The lateral border of the adductor longus, the medial border of the sartorius, and the inguinal ligament (the floor of which is created by the pectineus and iliopsoas) make up the femoral triangle. It includes the femoral nerve, artery, and vein from lateral to medial.
One centimeter below the mid-inguinal point, which is halfway between the pubic symphysis and the anterior superior iliac spine, or ASIS, is where the femoral artery may be felt
This is not the same as the inguinal ligament’s midpoint, which lies halfway between the ASIS and the pubic tubercle. Penetrating trauma to the thigh might cause injury to the femoral nerve. Additionally, it may sustain injury during hip surgeries, especially the less usual anterior approach, where the nerve may be stretched and harmed. The knee reflex is also mediated by the femoral nerve fibers.
Surgical Importance
For arterial access in a variety of operations, including the repair of aortic aneurysms, surgeons utilize the femoral artery. Before performing such an operation, the femoral nerve must be identified since injury to the nerve may cause any of the muscles innervated by the femoral nerve to stop functioning.
The rectus femoris has between one and four branches, according to research, with two branches being the most typical innervation pattern. Therefore, it’s critical to recognize and be aware of the potential variations and landmarks of the several potential branches.
Anesthesia is often administered across the medial leg as far distally as the medial malleolus when the great saphenous nerve is severed for use in heart bypass surgeries. To prevent the patient from becoming alarmed by the abrupt onset of loss of sensation in the saphenous nerve distribution, one should notify them beforehand.
FAQs
What symptoms and indicators point to femoral nerve damage?
symptoms. A few examples of symptoms are as follows: alterations in thigh, knee, or leg feeling, including discomfort, tingling, burning, numbness, or diminished sensation. weakness of the leg or knee, including trouble climbing and descending stairs, particularly while descending, and a sensation of the knee buckling or giving way.
What does the femoral nerve do?
In the lumbar plexus, the femoral nerve is the largest. The dorsal divisions of the L2-L4 ventral rami are its source. It aids in the lower limbs’ motor and sensory processes. Consequently, it regulates the main hip flexor muscles and the muscles involved in knee extension.
How to test a femoral nerve?
The patient lies prone while the knee is flexed to perform the femoral nerve stretch test. When the patient has anterior thigh discomfort, the test is considered positive.
How long does it take for injury to the femoral nerve to heal?
The stage of your injury, your ability to adhere to your rehabilitation plan, and other medical and lifestyle considerations are just a few of the variables that will affect this. The typical recovery time is two to three months for the first recovery and three to six months for the full recovery.
What is the best exercise for femoral nerve damage?
Pelvic tilts
To flatten your lower back against the floor or bed, try using your abdominal muscles. Then, as if you were trying to put your palm on the small of your back, try arching your lower back. Repeat this slowly and continuously, alternating between a flat back and an arch back.
References
- Femoral nerve. (2023, May 25). Kenhub. https://www.kenhub.com/en/library/anatomy/femoral-nerve
- TeachMeAnatomy. (2025, February 12). The femoral nerve – course – motor – sensory – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/nerves/femoral-nerve/
- Femoral nerve. (2023, July 24).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK551640/