8 Best Exercises For Polycystic Ovary Syndrome (PCOS)
Introduction
People assigned to females at birth, frequently during their reproductive years, are affected by the prevalent hormonal condition known as polycystic ovarian syndrome (PCOS). The appearance of tiny cysts on the ovaries, excessive levels of androgens (male hormones), and irregular menstrual cycles are some signs that define it. Numerous health concerns, such as insulin resistance, infertility, and an elevated risk of diabetes and cardiovascular disease, can be brought on by PCOS.
Exercise is a crucial component of PCOS management since it can enhance insulin sensitivity, maintain hormonal balance, and enhance general well-being. However, since every person’s condition is different, it’s imperative to speak with a healthcare provider before beginning any fitness regimen, particularly for those with PCOS.
People with PCOS may benefit from combining strength training and cardio workouts in their fitness regimen. Brisk walking, running, cycling, and swimming are examples of aerobic exercises that can help manage weight and enhance cardiovascular health. Resistance training and bodyweight exercises are examples of strength training activities that can help build muscle, which may help control insulin levels.
What is PCOS?
The most prevalent endocrine disorder affecting fertile women globally is called polycystic ovarian syndrome, or PCOS. Depending on the diagnostic criteria used, the prevalence can vary from 5% to 15%. Polycystic ovaries, clinical or biological hyperandrogenism, and chronic anovulation are the three criteria that must be present for PCOS to be diagnosed, under the standards of the specialized society.
Conditions that share clinical features with PCOS must be ruled out because it is an exclusion diagnosis, such as thyroid-related disorders, hyperprolactinemia, as well as non-classical congenital adrenal hyperplasia. A more comprehensive workup can be required for a specific patient if clinical features suggest other causes.
Despite being quite prevalent, PCOS is often misdiagnosed and requires numerous visits or evaluations by multiple doctors, all of which take place over more than a year. It is an annoying process for the sufferer. Delays in evaluation may exacerbate symptoms, making it more difficult for patients to adopt lifestyle changes that are necessary to improve PCOS symptoms and quality of life.
Obstructive sleep apnea (OSA), depression, endometrial cancer, obesity, metabolic syndrome, impaired glucose tolerance, type 2 diabetes mellitus (DM-2), endometrial cancer, and nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH) are among the morbidities that are linked to PCOS. The practitioner must have a low bar for workup if the patient has PCOS, even though there are different screening recommendations for each of these disorders.
Causes of PCOS:
PCOS is a complex disease. It has been demonstrated that a large number of susceptibility genes contribute to the pathophysiology of the disease. To varying degrees, these genes are involved in steroidogenesis and androgenic processes. According to twin studies, heritability is approximately 70%.
The environment has a big impact on how these genes are expressed, as well as how the disease starts and progresses. Two well-recognized ideas state that individuals with a genetic predisposition and exposure to particular environmental factors exhibit PCOS symptoms. Insulin resistance and obesity are two of the most common environmental factors. Another explanation that has been proposed is fetal androgen exposure.
Epidemiology of PCOS:
According to the diagnostic criteria, PCOS affects 5% to 15% of girls in the reproductive age range globally, making it the most prevalent endocrine disorder. The Rotterdam guidelines include a larger range of prevalence than the National Institutes of Health standards from 1990. According to the NIH 2012 workshop study, approximately 5 million women of reproductive age in the US suffer from PCOS. Without accounting for the significant comorbidities linked to PCOS, the healthcare system is expected to spend $4 billion annually on PCOS diagnosis and treatment.
Infertility, metabolic syndrome, obesity, poor glucose tolerance, DM-2, cardiovascular risk, depression, OSA, endometrial cancer, and NAFLD/NASH are among the disorders that have been linked to PCOS. Premature adrenarche, congenital virilizing diseases, prepubertal obesity, above-average or low birth weight for gestational age, first-degree blood relatives with PCOS, and the use of valproic acid as an antiepileptic medication have all been linked to an increased prevalence. Additionally, statistics show that Mexican Americans are more prevalent than African Americans and non-Hispanic whites.
Pathophysiology of PCOS
PCOS is a hyperandrogenic oligo-anovulation disorder that cannot be explained by any other disease. The diagnosis is exclusionary. However, it is responsible for most hyperandrogenic appearances. The cause of almost all PCOS instances is functional ovarian hyperandrogenism (FOH).
Two-thirds of PCOS presentations include typical functional ovarian hyperandrogenism, which is characterized by dysregulation of androgen synthesis and an excess of 17-hydroxyprogesterone (17-OHP) in response to gonadotropin stimulation. Instead of overreacting to 17-OHP, residual atypical FOH PCOS is characterized by a rise in testosterone after adrenal androgen production is suppressed.
Separated effective adrenal hyperandrogenism is seen in around 3 percent of PCOS patients. Minor PCOS cases make up the remaining cases. Although there is no indication of steroid secretory problems in these patients, practitioners feel that the majority of these people are obese, which accounts for their atypical PCOS. There is currently minimal therapeutic benefit to particular testing for the FOH subgroup.
Ovarian hyperandrogenism in function:
The three basic indicators of PCOS are polycystic ovarian morphology, oligoanovulation, and hyperandrogenism. Functional ovarian hyperandrogenism has several underlying causes, including genetic and environmental factors. This dysregulation is caused by an intrinsic imbalance between intraovarian regulatory mechanisms and hyperinsulin, which is known to sensitize the ovary to luteinizing hormone (LH) and affects the normal ovulation cycle by interfering with the homologous desensitization to the LH mechanism.
The ca cells in PCOS overexpress most steroidogenic enzymes and proteins linked to androgen synthesis, indicating a substantial abnormality in the quantity and activity of steroidogenic enzymes, such as the well-known P450c17. High levels of androgen and insulin are the primary reasons for early luteinization of granulosa cells.
The androgen hormone speeds up the early recruitment of follicles into the growth pool. Meanwhile, it triggers early luteinization, which influences the primary follicle selection. This results in the distinctive PCOS histopathologic abnormalities and severe anatomic changes that comprise PCOM. LH-induced desensitization of theca cells reduces the likelihood that excess LH is the primary cause of ovarian androgen excess, even if excess LH is necessary for the production of sex hormone release and gonadal steroidogenic enzymes.
About half of people with functional ovarian hyperandrogenism have atypical levels of insulin-resistant hyperinsulinism, which acts on theca cells to boost steroidogenesis, prematurely luteinize granulosa cells, and cause fat accumulation. Hyperandrogenism causes excess LH, which affects both the theca and the cycle that sustains luteinized granulosa. Changes in the pulsatile release of gonadotropin-releasing hormone (GnRH) brought on by ovarian dysregulation may produce a proportionate rise in levotropin (H) production and secretion in comparison to follicle-stimulating hormone (FSH).
LH encourages ovarian androgen synthesis, however, the proportionate decrease in FSH prevents proper activation of aromatase activity inside the granulosa cells, decreasing androgen conversion to the potent estrogen estradiol. This turns into a self-replicating, noncyclic hormonal cycle.
On the periphery, estrogens, primarily estrone, are produced from high serum androgens. Since conversion primarily occurs in the stromal cells of adipose tissue, obese PCOS patients will make more estrogen. This conversion results in continuous feedback at the pituitary and brain, as opposed to the regular oscillations in feedback observed in the presence of a growing follicle and rapidly fluctuating estradiol levels. Endometrial hyperplasia may result from unopposed endometrial estrogen stimulation.
Symptoms of PCOS:
Around the time of their first menstrual cycle, some women experience symptoms. Some people are unaware that they have PCOS until they have problems getting pregnant or have gained a significant amount of weight.
Here are a few of the most typical The following are some of the most common symptoms of PCOS: PCOS symptoms include:
- Period irregularities: The absence of ovulation prevents the monthly elimination of the uterine lining.
- Excessive bleeding: As your uterine lining grows over time, you may experience heavier-than-normal periods.
- Hair growth: Over 70% of women with this condition develop hair on their faces and bodies, particularly on their backs, tummies, and chests. Excessive hair growth is called hirsutism.
- Acne: Male-specific hormones can cause breakouts on the face, chest, and upper back by increasing sebum production.
- Gained weight: Obese or overweight women make up at least 80% of PCOS patients.
- Male pattern baldness: Eventually, the hair on the scalp may weaken and fall away.
- Skin darkening: Dark patches of skin may appear in creases like those on the neck, groin, and under the breasts.
- Headaches: Some women might get migraine as a result of hormonal changes.
How does your body react to PCOS?
Your fertility and other elements of your health may be impacted by very high androgen levels.
- Infertility: You must ovulate to become pregnant. The quantity of eggs produced for fertilization is decreased by infrequent ovulation.
- Metabolic syndrome: Approximately 80% of women with PCOS are overweight or obese. Obesity and PCOS raise the risk of high blood pressure, diabetes, low HDL (good cholesterol), and high LDL (bad cholesterol). These elements work together to form the metabolic syndrome, which raises the risk of stroke, diabetes, and heart disease.
- Sleep apnea: Sleep is disturbed by this disease, which causes many breathing pauses during the night. Sleep apnea is more common in women who are overweight, particularly those who also have PCOS. Obese women with PCOS have a five to ten times higher risk of developing sleep apnoea than women without PCOS.
- Endometrial cancer: During ovulation, the uterine lining sheds. If you do not ovulate each month, the lining may accumulate. Your chance of developing endometrial cancer may rise if your uterine lining is thicker.
- Depression: Hormonal changes and their side effects, such as increased hair growth, might negatively affect one’s emotional state. Anxiety and despair are common side effects for many PCOS patients.
Exercise and PCOS
When compared to women without PCOS, women with hormonal imbalances had higher rates of insulin resistance. Your body’s ability to use blood glucose as fuel is impacted by insulin resistance.
Physicians have connected obesity and inactivity to insulin resistance, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Not all women with PCOS are overweight. Fortunately, if you have PCOS, you can still benefit from physical activity for your health regardless of your weight.
- Reducing BMI:
- A meta-analysis of 16 research on PCOS and exercise found that high-intensity aerobic exercise was the most effective strategy for reducing insulin resistance and body mass index (BMI) in women with PCOS, per a study published in Frontiers in Physiology.
- Intense and moderate activity were compared by the researchers. They also found that treatments incorporating a balanced diet and vigorous exercise produced the largest BMI decreases.
- Managing weight:
- A study evaluating lifestyle therapies for PCOS found that exercise helped reduce weight, abdominal fat, and fasting insulin levels.
- Additionally, the study found that exercise may help women with PCOS of all weight ranges maintain or lose weight to enhance their general health and looks.
- Any kind is beneficial:
- A review of studies on the advantages of various forms of exercise, such as aerobic and strength training, for women with PCOS was unable to pinpoint one as being especially beneficial. The findings were reported in the journal Sports Medicine.
- A few studies contrasted moderately intense treadmill walking or running with severe intensity, strength training with aerobic activity, and stationary bike riding with outdoor cycling. The researchers did find that certain types of exercise may help patients with PCOS.
According to these and other research, exercise, particularly regular exercise, can help persons with PCOS. If you can incorporate an activity you enjoy into your workout, you’ll get extra credit.
Why is working out helpful for PCOS?
- Hormone balance: By increasing endorphin levels and decreasing insulin and estrogen levels, exercise contributes to hormonal balance.
- Enhancing your mood: Because of hormone imbalances and other symptoms, people with PCOS may be more susceptible to depression. Endorphins are feel-good hormones released by regular exercise.
- Helping with weight loss: For people with PCOS, losing weight can be depressing. You can lose weight by eating a healthy diet and engaging in frequent, fun exercise.
- Enhancing the quality of your sleep: Engaging in physical activity promotes restful sleep. Sleep apnea, snoring, and other issues are more common among PCOS patients. Obesity also exacerbates these problems.
- Lowering your chance of diabetes: The risk of diabetes can be reduced by engaging in exercise that improves insulin sensitivity.
- Aiding in cholesterol management: High cholesterol, which can be reduced with diet and exercise, is more common in women with PCOS.
- Reducing the risk of cardiovascular diseases: You are more likely to get cardiovascular disease and high blood pressure. Engaging in physical activity can help heart health.
What are the types of Exercises for PCOS?
The list below might contain the finest choices for you.
- Walking:

Let’s start with the simplest. As previously mentioned, PCOS patients are typically advised to continue exercising to a certain extent. Even if one lacks the time or energy to accomplish anything else, walking is a simple activity that one can do.
Walking for five minutes every day may also help you control the symptoms and effects of PCOS. The morning is the ideal time to complete this task. You will achieve better benefits more quickly if you walk or jog quickly.
- Cardio:

For people with PCOS, maintaining an increased heart rate is essential. Exercises that target the heart can help you achieve this. Swimming is the most popular activity while walking is the least. You can push yourself to establish goals for pace and distance once or twice a week if you can swim. It will help you keep up your physical fitness and vitality.
You can also try dancing and aerobics if you have talent in this area. There are further cardiovascular advantages of cycling. While managing PCOS, these mild exercises may help you maintain your regular physical activity routine.
- Lightweight Exercise:

Women with PCOS usually have high levels of androgen, which causes them to grow muscle mass quickly. As a result, they also experience issues and challenges with weight gain and enhanced muscle strength. To avoid such a situation, it is therefore better to burn the extra calories. Lightweight training should be done at least twice a week for this.
If you are new to weight training, always consider working with a professional trainer. Every few weeks, set up a time to meet them for a basic weight training session. In this way, you can control your weight even if you have PCOS.
- Zumba or Aqua Aerobics:
Recently, working out in the pool has become increasingly popular. While recovering from PCOS, these are both calming and helpful. Aqua aerobics, or Zumba, has gained popularity among women. With the help of these simple and fun routines, women with PCOS can maintain their physical fitness levels without needlessly gaining weight.
- Exercise for Strength:

Bodyweight and strength exercises should be incorporated into the best PCOS workouts. Exercises that engage the triceps, like as squats, push-ups, and dips, can improve how well your body uses insulin. However, they can also aid in the development of muscle. Unless drugs are utilized, bulking up is not dangerous.
You can use weights, resistance bands, or your own body weight for this type of workout to gain muscle. This technique may help you become more fit and healthy. If you have PCOS and wish to control your weight, this can help.
- HIIT Exercises:

It is believed that exercises like high-intensity interval training (HIIT) are essential for PCOS problems. It comprises a strenuous exercise program punctuated by downtime. This is how you may include exercises like burpees, tuck jumps, and mountain climbers.
With more strenuous training, it aims to boost the advantages of cardio. Most individuals believe it’s a good way to maintain a healthy weight and heart. Additionally, it speeds up the improvement of insulin resistance.
- Core Strength:

If you weigh more than you should, you might get lower back pain frequently. It may exacerbate your PCOS problems. By strengthening your core, you might be able to prevent these problems. By strengthening these muscles, which support your spine, you can improve your posture in general.
Exercises that increase pelvic, leg, and upper abdominal core strength and endurance are beneficial for PCOS-affected women who are attempting to conceive. Strengthening these core muscles will help ensure a safe pregnancy.
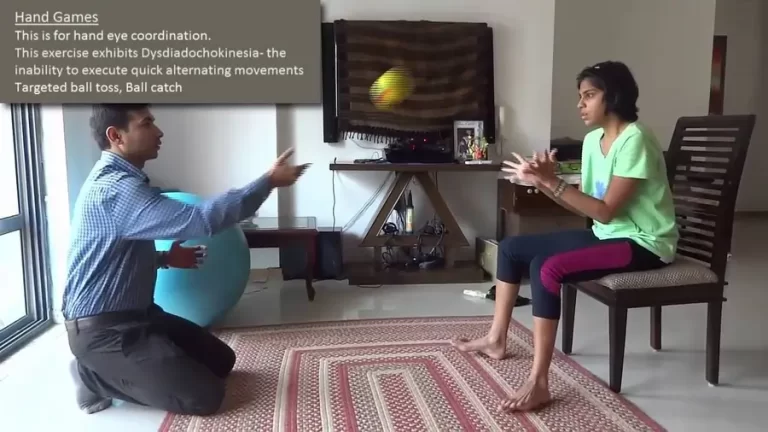
- Mind-Body Practices:

The link between the mind and body is evident in current clinical research. Women who are in good mental health are likely to recover from PCOS rapidly. It also makes it possible to react quickly to stress and anxiety without compromising one’s mental or physical health.
These exercises mostly come from tai chi, yoga, and pilates. These can help you lose weight and also greatly reduce mental stress and anxiety. These exercises are therefore your one-stop shop for most of your PCOS symptoms and effects.
The best workout plan for PCOS
- Cardiovascular steady-state workouts:
- When you are exercising lightly, these routines will increase your heart rate to a maximum of 50 to 70 percent. Dancing, walking, riding, and aerobics classes are a few examples of this kind of aerobic exercise.
- Workouts that alternate high-intensity exercise intervals with rest periods are known as HIIT workouts. High-intensity interval training often uses exercises like burpees, tuck jumps, and mountain climbers. How long you can maintain a habit depends on how much you enjoy working out.
- Unlike HIIT, interval training does not necessarily require you to attain your maximal heart rate, but it does allow you to exercise at varying intensities. To keep your heart rate elevated, this type of exercise typically consists of many different exercises performed in one session.
- Exercises for the mind and body:
- Stress and worry have a greater physical impact on women with PCOS. Yoga, Pilates, and tai chi are examples of mind-body exercises that can lower stress levels and burn calories, two things that might make PCOS symptoms worse. Therefore, you ought to include this in your exercise routine for PCOS.
- Strengthening exercises:
- To gain muscle, use resistance bands, weights, or your body weight. This kind of training can aid in the development of strong bones and muscles.
Aerobic exercise should be performed for at least 30 minutes each day as part of PCOS treatment. You can incorporate exercise into your life in several ways, such as the following:
- Establish a fitness routine that involves setting up six stations and working out for one to two minutes at each one. Exercise examples include:
- Lunges.
- Crunches.
- Bicep curls.
- Jumping jacks.
- Walking outside or on a treadmill for 30 to 45 minutes each day is recommended.
- Enroll in an online or in-person aerobics course. Examples include spinning, boxing, and dancing.
- Make use of online or in-person HIIT training. There are several exercise videos on YouTube that you can follow at home. Just make sure the provider of the regimen is reliable.
- Use a studio, a gym, or an online course for tai chi, yoga, or pilates. If you have never practiced, seek advice from a trainer so they can assess your form and safety.
Effects of Exercise on PCOS
Modifying one’s lifestyle for the better is essential to managing PCOS. Two of the best methods to do that are through diet and exercise, and both must be maintained for these lifestyle changes to be effective. Women with PCOS can benefit greatly from routine physical activity in methods that go far beyond weight loss.
- Strengthens insulin sensitivity: Studies have shown that regular strength and aerobic exercise can enhance your body’s response to insulin, reducing your risk of diabetes and other issues.
- Reduces cholesterol: Women who have PCOS are more likely to have elevated triglycerides and cholesterol. Additionally, this may exacerbate metabolic syndrome, which is more common in PCOS patients. Exercise and a nutritious, low-fat diet can help reduce cholesterol.
- Boosts endorphin production: Depression symptoms are more common in women with PCOS. Your body releases feel-good compounds called endorphins when you exercise. You can lessen some depressive symptoms and enhance your stress management by doing this.
- Better Sleep: Regular exercise can speed up your sleep rate and enhance the quality of your sleep. Women with PCOS are more likely to experience sleep apnea, snoring, and even insomnia. Find out if regular exercise—but not right before bed—can improve your quality of sleep at night.
- Control of Hormones: Your body burns the fat that is already stored in your body as fuel when you consume more calories than you consume. This naturally lowers insulin levels and aids in weight loss. Moreover, the body’s production of estrogen is impacted by increased body fat. Reducing some of those excess fat deposits will help with PCOS and possibly hormone balance.
The following advice can be helpful if you’re unsure of how to start or alter your exercise regimen:
- Pay attention to the motions that make you happy. It should be enjoyable to work out! To find what makes you happy, take your time examining a variety of possibilities.
- Put things in order and sort it. In the same way, you might schedule time for an appointment or other commitments.
- Keep an open mind. The context is important as usual. Always be prepared to adjust your training regimen as necessary, and keep an eye on factors like sleep, stress, and nutrition.
Everybody has a slightly different fitness regimen, and there is no one ideal way to train. Our ultimate objective is to develop a movement program that supports PCOS recovery and overall wellness. This entails continuously assessing the situation and making adjustments in response to your body’s response.
Which exercises should PCOS patients avoid?
Even though HIIT activities are among the best for PCOS, patients should be cautious about how intense they are. For instance, if you engage in an intense activity that isn’t healthy for your body, you may worsen the symptoms and effects of PCOS.
A persistent attempt to prevent weight gain could be interpreted by your body as self-inflicted stress in response to an outside threat. It will cause the hormones to react strongly. Excessive weightlifting or regular push-ups can cause these symptoms in PCOS patients.
What safety measures need to be taken?
Therefore, it is always recommended to receive training and sessions from fitness professionals. You should discuss any medical problems you may have with your doctor before choosing an exercise regimen.
In addition, it would be helpful if you maintained regular communication with the gym’s trainers and doctors. To ascertain whether exercising is the source of these issues, find out whether you are at risk for any physical or mental health issues. Reduce the intensity of your workout in these circumstances.
With any luck, you now comprehend the PCOS control workouts. According to this article, regular exercise and a healthy diet may help you manage and recover from the symptoms of this condition more rapidly. However, since rigorous exercise routines might worsen PCOS symptoms and related problems, it would be wise to avoid them.
PCOS and diet
The “best” diets for PCOS sufferers have been the subject of numerous research. The Androgen Excess and PCOS Society has advised women to do the following in light of this research:
- Reduce your daily caloric intake by 500–1,000 if you are overweight.
- Saturated fats, including those found in full-fat dairy products, butter, cheese, and high-fat steak, should make up less than 10% of your caloric intake.
- Whole-grain bread and cereals, fruits, fiber, and “healthy” fat sources like nuts and avocados can all be used to replace high-fat meals.
- Avoid trans fats as much as possible.
- Increase your daily intake of fiber by five to ten grams.
If you’re not sure how to start making these dietary changes, consult your physician. For women with PCOS, your doctor might also recommend consulting a dietician to develop a customized food plan.
- An instance of a diet and exercise plan:
- Weekly exercise hours are not required to improve PCOS. Exercise sessions that last anywhere from 30 minutes a day, three times a week, to three hours a week have been shown in studies to alleviate the metabolic and reproductive symptoms linked to PCOS.
- Exercise Routine:
- The Androgen Excess and PCOS Society recommends aiming for at least 30 minutes of moderate-to-intense physical activity each day and increasing your exercise intensity when you can. The following are some suggestions for making fitness a part of your life:
- Set up six stations and work out there for one to two minutes at a time to create your interval training program. Among the examples are:
- Squats
- Jumping jacks
- Lunges
- Bicep curls
- Crunches
- Set up six stations and work out there for one to two minutes at a time to create your interval training program. Among the examples are:
- Every day, spend 30 to 45 minutes walking outside or using a treadmill.
- Attend a gym or take an aerobics lesson online. Examples include dancing, spinning, boxing, and stepping.
- Take a HIIT class online or at a fitness facility. YouTube has a lot of videos about working out at home. Just make sure the software comes from a reliable source.
- Practice yoga, pilates, or tai chi online, at a studio, or at a gym. If you have never practiced, you may want to consult a trainer to evaluate your form and safety.
- Try switching up your workout routine by doing a different type of session three times a week if you discover that your commitment to a fitness routine waned because you were bored.
- The Androgen Excess and PCOS Society recommends aiming for at least 30 minutes of moderate-to-intense physical activity each day and increasing your exercise intensity when you can. The following are some suggestions for making fitness a part of your life:
- A healthy eating plan: Try to include one or more of the following healthy eating habits into each meal and snack:
- Every meal should contain some lean protein, such as skinless chicken, fish, or tofu.
- Add some veggies, like spinach, kale, broccoli, or peppers.
- Add some beans, nuts, or lentils.
- Select fruits with vivid colors, such as red grapes, oranges, blueberries, and cherries.
- Choose wholegrain bread and pasta substitutes.
- By following these recommendations, you may often stay within the daily calorie requirements given your weight, height, and overall health.
- Fertility, PCOS, and exercise:
- 80% of women who are infertile due to irregular ovulation are estimated to have PCOS, according to a survey published in the journal Physical Exercise for Human Health.
- Exercise and, ideally, weight loss of at least 5% of body weight can help women reestablish their ovulation cycles and boost the regularity of their periods. Exercise and nutrition together are more effective than diet alone in the treatment of PCOS and infertility.
- When to consult a physician:
- When you have PCOS, it’s a good idea to talk to your doctor about changing your lifestyle to improve your general health. When treating PCOS, you should see your doctor about any other medical disorders that may affect your ability to exercise. Arthritis and heart conditions are two examples.
Conclusion
A key component of PCOS management may be exercise. In addition to improving your physical health, exercise also helps you feel less stressed.
If you’re unsure where to start, seeing your physician and working with a personal trainer could help steer you in the right direction. PCOS symptoms can be lessened by sticking to a regular exercise routine, at least three times per week.
FAQ
Is yoga or the gym better for PCOD?
Yoga, Pilates, and tai chi are examples of mind-body exercises that can lower stress levels and burn calories, two things that might make PCOS symptoms worse. Therefore, you ought to include this in your exercise routine for PCOS. Strengthening exercises: To gain muscle, use resistance bands, weights, or your body weight.
Which food is best for PCOD?
High-Fibre Foods: Including foods high in fiber in your diet might help normalize blood sugar levels because insulin resistance is a typical consequence of PCOD. Legumes like beans and lentils, as well as whole grains like brown rice, quinoa, and whole wheat bread, should be a part of your PCOD diet plan for weight loss.
Which fruit is not good for PCOS?
Apricots, dried.
Overripe bananas.
Dried figs.
Lychee is in syrup cans.
Peaches in a thick syrup can
Raisins.
Can PCOS affect breast size?
Women with PCOS may gain weight because of diabetes and metabolic disorders. This suggests that they are more likely to become obese, which is known to disrupt breastfeeding. Insulin resistance is also thought to affect breast development, milk synthesis, and secretion.
Can walking reduce PCOS?
Even a half-hour daily walk could be helpful if you’re not into workout and weightlifting. You may try taking a walk in a park or using a treadmill. For optimal effects, incorporate intervals into your walking routine. Take a five-minute walk at a moderate pace after five minutes of fast walking or jogging.
What does a PCOS belly look like?
It is often large and bloated, but it might be small and spherical, depending on genes and other factors. It feels hard to touch and usually includes visceral fat buildup in the lower belly. Another indicator of a PCOS belly is an apple-shaped physique with a waist-to-hip ratio of more than 0.87.
Can I get pregnant with PCOS?
Indeed. Having a PCOS diagnosis does not preclude being pregnant. PCOS constitutes one of the most common and curable causes of female infertility. The ovaries of women with PCOS are unable to produce and release eggs during ovulation due to a chemical imbalance.
When is the ideal time to work out if you have PCOS?
Some ladies get up earlier in the morning to work out, or they try to do it during their lunch break or after work. There is no perfect time to exercise; it is best done on a regular basis.
References:
Rasquin, L. I., Anastasopoulou, C., & Mayrin, J. V. (2022, November 15). Polycystic Ovarian Disease. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459251/
Vaghela, M. (2023, December 13). 8 Best Exercises For Polycystic Ovary Syndrome (PCOS). Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/exercises-for-polycystic-ovary-syndrome-pcos/#Is_yoga_or_the_gym_better_for_PCOD
Sullivan, T. (2024, October 17). Exercise for PCOS: what are the best and worst exercises for PCOS? Fertility Family. https://www.fertilityfamily.co.uk/blog/exercise-for-pcos-what-are-the-best-and-worst-exercises-for-pcos/
Watson, S. (2023, February 26). Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment. Healthline. https://www.healthline.com/health/polycystic-ovary-disease
Crna, R. N. M. (2020, December 1). The Best Types of Exercise for Polycystic Ovarian Syndrome (PCOS). Healthline. https://www.healthline.com/health/womens-health/exercise-for-pcos