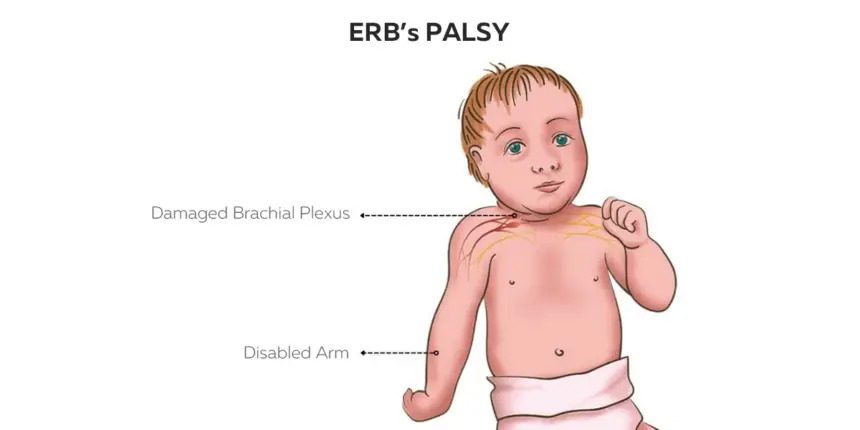
Erb’s Palsy
What is Erb’s Palsy?
Erb’s palsy, also known as Erb-Duchenne palsy or brachial plexus birth palsy, is a condition affecting the shoulder and arm that causes weakness or loss of skeletal muscle function
It is named after Wilhelm Erb, one of the first medical professionals to identify the condition.
Erb’s palsy is the most common form of brachial plexus condition that results from nerve injury during the childbirth process or accidental trauma.
The brachial plexus is a network of nerves that runs around the neck and supplies all of the arm muscles. These nerves carry movement and feeling to the shoulders, arms, hands, and fingers. Palsy signifies weakness
Erb’s point refers to the upper trunk of the brachial plexus. Six nerves merge here. An injury to the upper trunk of the brachial plexus causes Erb’s paralysis.
Epidemiology
One or 2 kids out of every 1,000 are born with brachial plexus birth palsy. Both genders equally affect male = female
Anatomy
- The brachial plexus has five sections: roots, trunks, divisions, cords, and branches. There are five “terminal” branches and multiple “pre-terminal” or “collateral” branches that exit the plexus at various points throughout its length.
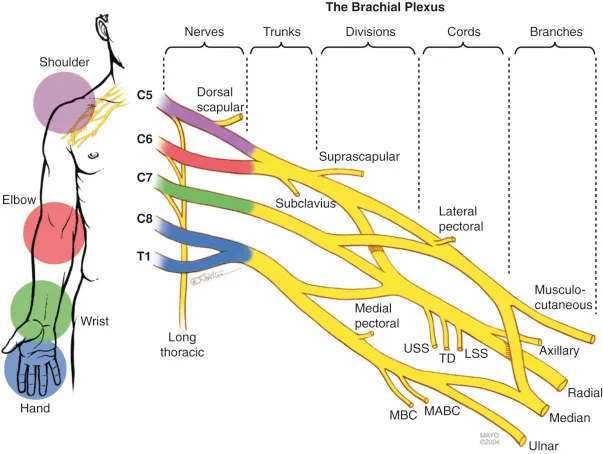
- Roots (C5-T1): These are the initial nerve fibers that emerge from the spinal cord. The five roots are C5, C6, C7, C8, and T1.
- Trunks: The roots converge to form three trunks: upper (C5-C6), middle (C7), and lower (C8-T1) trunks.
- Divisions: Each trunk has two divisions: anterior and posterior. The anterior divisions combine to form the lateral cord, while the posterior divisions form the posterior cord. The middle trunk’s anterior division joins the lateral cord directly.
- Cords: The brachial plexus has three cords:
- The lateral cord is made up of the upper and middle trunk’s anterior divisions (C5-C7).
- The medial cord arises from the front section of the lower trunk (C8-T1).
- The posterior cord forms the posterior divisions of all three trunks (C5-T1)
5. Branches: The cords give rise to major branches that supply the upper limb:
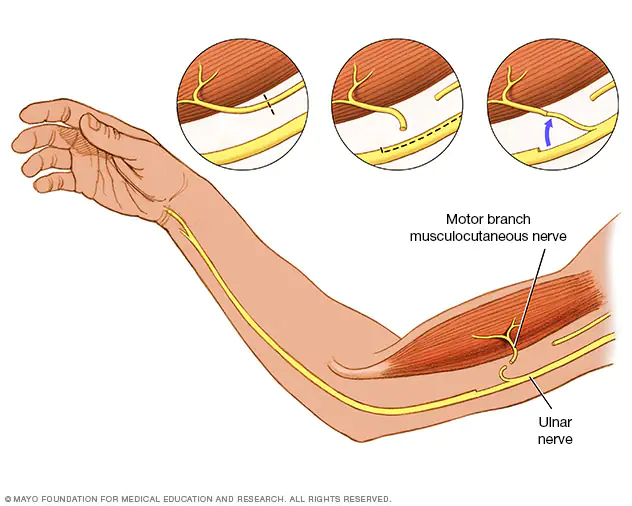
- Lateral cord branches include the Musculocutaneous nerve and the lateral root of the Median nerve.
- Medial cord branches include the Medial root of the median nerve and ulnar nerve.
- Posterior cord branches include the Axillary nerve and radial nerve.
6. Terminal Branches
- The muscles in the arm’s anterior compartment are innervated by the musculocutaneous nerve.
- Median nerve: Innervates muscles in the forearm and hand, and provides sensory innervation to the lateral palm and fingers.
- Ulnar nerve: Innervates muscles of the forearm and hand, and provides sensory innervation to the medial palm and fingers.
- The axillary nerve supplies the deltoid and teres minor.
- Radial nerve: Innervates muscles in the posterior compartment of the arm and forearm, and provides sensory innervation to the posterior arm and dorsal hand.
Mechanism of injury
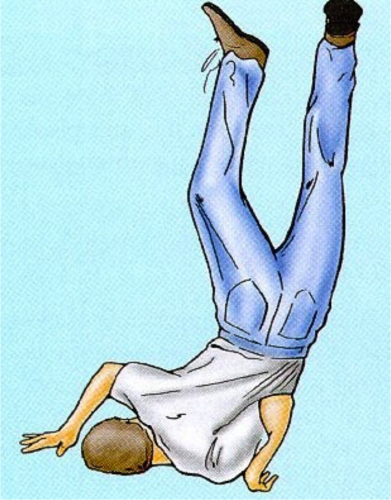
- Unwanted separation of the head from the shoulder, which frequently happens in birth injury, falls on the shoulder from height and during anesthesia.
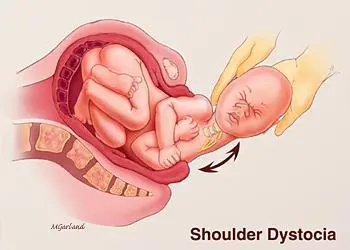
- Erb’s palsy is common in newborns after a difficult vaginal delivery or even following a cesarean surgery. During birth, your healthcare practitioner may have to shift your baby’s head to one side to allow for the delivery of their shoulders. In some cases, excessive pull or traction from the neck can cause nerve stretching resulting in injury, and potentially tears. This kind of Erb’s palsy is also known as brachial plexus birth palsy, obstetric brachial plexus palsy, or brachial plexus birth damage. It may be related to high birth weight, maternal diabetes, and extended labor.
- A newborn may develop Erb’s palsy as a result of the way they lie in the uterus throughout pregnancy and when labor begins
- Shoulder dystocia occurs when the baby’s shoulder becomes caught behind the mother’s pelvic bone during birth.
- Erb’s palsy can also affect people who have suffered serious traumas.
- Traffic accidents, especially those involving motorcycles, are the main reason for injuries to the brachial plexus in teens and adults.
- Other causes of these injuries include
- gunshot or knife wounds,
- industrial accidents,
- falls from a height on the shoulder,
- contact sports injuries such as football,
- surgical complications,
- and tumors.
- Men are more prone to sustaining these sorts of injuries.
What are the symptoms and Signs of Erb’s palsy?
Erb’s palsy symptoms vary according to the severity of the nerve damage. Common signs and symptoms include:
- Weakness or paralysis in the affected arm.
- The shoulder, arm, and elbow are paralyzed or weak. Lack of muscle control, leading to difficulty moving the arm. You can’t move your arm away from your body or bend your elbow.
- Limited range of motion in the shoulder, elbow, or wrist.
- Feeling numbness or tingling in the arm or hand or uncomfortable in your arm or hand.
Signs of Erb’s palsy

- It causes the paralysis of Mainly: the biceps, deltoid, brachialis, and brachioradialis muscles
- Partly Rotator cuff muscles supraspinatus, infraspinatus, and supinators
- it causes the inability to do
- Abduction, lateral rotation of the arm
- flexion and supination of the forearm and
- Biceps and supinator jerks are lost
- it leads to deformity in the upper extremity which
- The arm: hangs by the side, is adducted, and turned medially
- Forearm: Extended and pronated
- Wrist flexed and fingers curled.
- The deformity is additionally identified as “policeman’s deformity” or “waiter’s hand deformity.”
How is Erb’s palsy diagnosed?
Doctors diagnose Erb’s palsy using a combination of physical examinations, imaging tests (such as X-rays or MRIs), and nerve investigations (electromyography or nerve conduction studies) to measure nerve function and determine the severity of the injury.
- Electromyography (EMG). This test determines how well muscles and nerves function.
- Magnetic resonance imaging (MRI) of the shoulder might show shoulder dislocation; the presence of pseudomeningoceles indicates avulsion damage to the affected spinal roots.
- A computed tomography (CT) scan of the shoulder might show shoulder dislocation; the presence of pseudomeningoceles indicates avulsion damage to the affected spinal roots.
Physical Examination
- To confirm the diagnosis, a complete history and physical examination are performed, with a special focus on the neurological examination.
History- to learn about pregnancy issues such as maternal obesity, gestational diabetes, prenatal macrosomia, protracted second-stage labor, shoulder dystocia, and the usage of assistive methods such as forceps during delivery.
Physical examination typically reveals that the afflicted arm moves just slightly or not at all. - Neurologic examination: Determine muscular strength, feeling, and reflexes; the Moro reaction is missing on the afflicted arm.
How is Erb’s palsy treated?
Treatment for Erb’s palsy depends on the severity of the condition and may include the following approaches:
Medications
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain medications may be prescribed to manage discomfort associated with muscle tightness or nerve irritation.
Physiotherapy Treatment
Aims
- Decrease the pain and discomfort
- prevent contracture and deformity
- decrease muscle tightness and muscle spasm
- improve the mobility
- improve muscle strength and power
- improve the functional activities
Pain Relief
- Heat therapy: The application of heat, such as moist heat packs or warm baths, can help relax muscles, improve blood flow, and reduce pain and stiffness.
- Cold therapy: Cold packs or ice application can reduce inflammation, numb pain, and alleviate acute pain symptoms.
- Electrical stimulation: Transcutaneous electrical nerve stimulation (TENS) or electrical muscle stimulation (EMS) can help reduce pain perception and promote muscle relaxation.
- Ultrasound therapy: High-frequency sound waves applied to the skin can generate heat deep within tissues, which can help reduce pain, inflammation, and muscle spasms.
improve mobility
- Soft tissue mobilization: Therapists use hands-on techniques such as massage, myofascial release, and stretching to reduce muscle tension, improve circulation, and alleviate pain.
- Joint mobilization: Gentle movements applied to the joints help improve joint mobility, reduce stiffness, and relieve pain associated with joint dysfunction.
- Passive movement: slow passive movement to maintain muscle property.
- Range of motion exercises: Physical therapy focuses on maintaining or improving the range of motion in the affected arm and shoulder joints.
- Hydrotherapy combines exercise with water. Water gives support, making exercise less difficult.
Decrease muscle tightness and spasm
- Gentle stretching exercises targeting the tight muscles can help reduce muscle tightness and improve flexibility.
- Static stretching involves holding a stretch position for some time to elongate the muscle and release tension.
- Dynamic stretching involves controlled, repetitive movements that gradually increase the range of motion and reduce muscle tightness.
- Applying heat to the affected area can help relax muscles, increase blood flow, and reduce muscle spasms.
- Heat can be applied using warm packs, heating pads, warm baths, or infrared therapy
- TENS can interfere with pain signals, while EMS can stimulate muscle contractions to promote relaxation.
Myofascial Release Techniques:
- Foam rolling: Using a foam roller or similar tool on the affected muscles can help release tightness in the fascia (connective tissue surrounding muscles) and reduce muscle tension.
- Massage therapy: Therapeutic massage techniques, such as deep tissue massage, trigger point therapy, and myofascial release, can help loosen tight muscles, improve blood flow, and reduce spasms
Prevent contracture and deformity
- Specific stretching exercises target tight muscles and connective tissues to prevent contractures. Stretching should be performed regularly and gently to avoid causing injury or discomfort.
- Focus on stretching muscles that are prone to tightness due to imbalance or reduced mobility, such as the shoulder internal rotators and elbow flexors in cases of Erb’s palsy.
- Proper positioning is crucial to prevent contractures and deformities. Physiotherapists teach parents and caregivers how to position the child’s body correctly during rest and activities to maintain optimal alignment and joint integrity.
- Orthotic devices such as splints or braces may be recommended to support proper positioning, prevent contractures, and promote alignment during periods of rest or activity.
- Splints or braces: Orthotic devices may be used to support the affected arm, improve positioning, and prevent contractures (shortening of muscles or tendons).
- Slings: A sling may be used to support the arm and promote proper alignment during healing.
- airplane splint can be used in patients with Erb’s palsy.
- splint should be worn for 23 hours a day
- Electrical stimulation can be given to initiate muscle movement
- Galvanic and Faradic currents can be given in the initial stage.
Sensory stimulation:
- Activities aimed at stimulating sensory input in the affected arm can help improve awareness and function.
Strengthening Exercise
- Strengthening exercises: Specific exercises target the muscles affected by Erb’s palsy to improve strength and function.
- Isometric Exercises: Contracting the muscles without movement can also help strengthen them. For example:
- Isometric Shoulder Press: Press the affected hand against a stable surface, such as a wall, without moving the arm. Hold a contraction for a few seconds before releasing.
- Isometric Bicep Contraction: Bend the affected arm at the elbow and press the palm against the abdomen. Hold a contraction for a few seconds before releasing.
- Resistance Band Exercises: Using resistance bands can provide gradual resistance to strengthen the muscles. Some exercises include:
- Shoulder External Rotation: Attach a resistance band to a stable object and hold the other end with the affected hand. Keep the elbow at your side and rotate the forearm outward against the resistance.
- Shoulder Flexion: Hold one end of the resistance band with the affected hand and the other end with the unaffected hand. Lift the affected arm forward and upward against the resistance.
- Shoulder Abduction: Attach the resistance band to a stable object at waist height. Hold the band with the affected hand and lift the arm sideways against the resistance.
- Functional Training: Incorporate functional activities into the exercises to improve overall arm strength and coordination. This can include reaching, lifting objects of varying weights, and practicing daily tasks using the affected arm.
- Neuromuscular re-education: Therapists work on retraining the nerves and muscles to improve coordination and control.
- Functional activities: Therapy includes activities that simulate daily tasks to help the child develop functional use of the affected arm.
- Close kinematics exercise:
- close kinetic exercise: Closed kinetic chain exercises involve movements where the distal part of the limb (such as the hand) is fixed or stabilized, while the proximal part of the limb (such as the shoulder) moves. These exercises are often recommended in Erb’s palsy rehabilitation because they provide stability to the affected limb while engaging multiple muscle groups. Here are some closed kinetic chain exercises that may be beneficial for Erb’s palsy
- Wall Push-Ups
- Assisted Pull-Ups
- Plank Variations
- Bosu Ball exercise
Surgical Management
If your baby’s palsy does not improve by 6 months old, your physician might suggest surgery, such as
- Nerve surgery:
- Surgical interventions such as
- nerve grafting
- nerve transfers
- Nerve Repair
- or neurolysis (nerve decompression) may be considered to repair or reconstruct damaged nerves.
- It’s important to understand that any form of nerve healing and rebuilding occurs gradually; the outcomes aren’t immediate.
- Surgical interventions such as
- Muscle or tendon surgery: Procedures like muscle releases, tendon transfers, or lengthening surgeries may be performed to improve muscle function or release contractures.
Prevention
There are certain risk factors for shoulder dystocia (a baby’s shoulder becoming caught within the mother’s pelvis, which is linked to Erb’s palsy). These factors include:
- High newborn birth weight and/or a gestational parent who is overweight or obese.
- Diabetes in the gestational parent (pre-pregnancy or gestational diabetes).
- A previous pregnancy involving shoulder dystocia.
- Being pregnant with more than one baby.
- Mother is Using medicine eg. oxytocin or an epidural.
- Breech birth position (your baby is not head-first in the delivery canal).
FAQ
When should I visit my doctor regarding Erb’s palsy?
The longer nerve damage goes untreated, the more difficult it will be to get a positive outcome. As a result, you should consult with a physician as soon as possible to monitor your or your infant’s recovery and assess whether or not intervention is required.
That is true if you are an adult with Erb’s palsy. Please notify your healthcare physician if anything feels worse, if you are having difficulty with the exercises, or if you have any other concerns.
Which splint is used for Erb’s palsy?
An Airplane splint can be used for Erb’s Palsy.
it will provide stability at the shoulder, elbow, and wrist joints
it will keep your arm abducted and forearm straight and supinated
it is Lightweight, and well-padded splints will support the forearm.
Can Erb’s palsy be fully cured?
Mild cases of Erb’s palsy resolve in a few months with appropriate and timely therapy. But even with therapies and surgery, extreme instances might never fully recover. Early detection of Erb’s palsy is the best defense against ineffective treatment for your child.
References
- ERB’s Palsy Causes, Diagnosis and Treatment | Baptist Health. (n.d.). Baptist Health. https://www.baptisthealth.com/care-services/conditions-treatments/erbs-palsy
- Center, B. I. J. (2023, November 26). Erb’s Palsy – Causes, Symptoms, Treatment, and Prognosis. Child Birth Injuries. https://www.childbirthinjuries.com/erbs-palsy/
- Brachial Plexus. (n.d.). Physiopedia. https://www.physio-pedia.com/Brachial_Plexus
- Professional, C. C. M. (n.d.-h). Erb’s Palsy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21986-erbs-palsy
- Cerebra Palsy Guidance. (2023, December 13). ERB’s Palsy Overview | Symptoms, causes, treatment. Cerebral Palsy Guidance. https://www.cerebralpalsyguidance.com/birth-injury/erbs-palsy/
- Brachial plexus injury – Symptoms and causes – Mayo Clinic. (2024, March 27). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/brachial-plexus-injury/symptoms-causes/syc-20350235
- Landis, M. N., & Adams, D. H. (2013). Drugs for the internist. In Elsevier eBooks (pp. 408-423.e3). https://doi.org/10.1016/b978-1-4377-2003-7.00034-0





One Comment