Chronic Obstructive Pulmonary Diseases (COPD)
What is a Chronic Obstructive Pulmonary Diseases (COPD)?
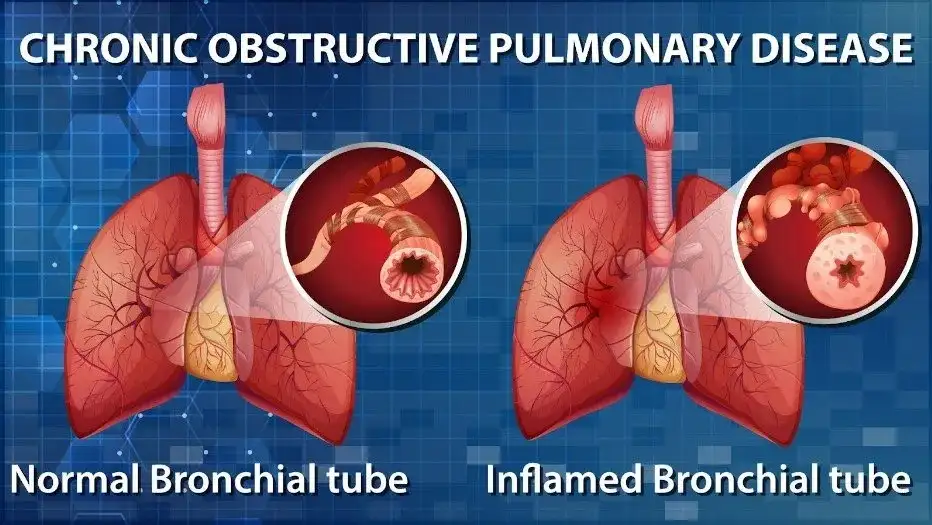
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that causes airflow obstruction, making breathing difficult.
People with COPD may experience lung damage or phlegm blockage. Symptoms include fatigue, wheezing, breathing difficulties, and coughing, occasionally with phlegm.
The most prevalent causes of COPD are air pollution and smoking. Other health issues are more likely to affect people with COPD.
Although there is no cure for COPD, symptoms can be lessened if a person gets vaccinated against illnesses and abstains from smoking and air pollution. Additionally, medications, oxygen, and pulmonary rehabilitation can be used to treat it.
When you have COPD, the airways and lungs will change as follows:
- Loss of flexibility in the lungs’ alveoli, or air sacs, and airways.
- Airway constriction, inflammation, and scarring (fibrosis).
- Mucous in your airways that is thick.
- The walls connecting your alveoli are destroyed. They get bigger and trap more air as a result.
- Flare-ups, or worsening of symptoms, such as coughing, wheezing, thicker mucus, and extreme difficulty breathing, are common in people with COPD. Significant exacerbations may require hospitalization.
- As time goes by, COPD grows worse. Flare-ups occur more frequently and become more severe. Although some people deteriorate more quickly, this often takes years or decades.
Pathophysiology
- The pathological alterations associated with COPD are caused by the aforementioned pathogenic processes. These lead to physiological anomalies, including ciliary dysfunction and mucous hypersecretion, obstruction of airflow and hyperinflation, abnormalities in gas exchange, pulmonary hypertension, and systemic consequences.
Hypersecretion of mucus and malfunctioning cilia
A persistent productive cough is the result of mucous hypersecretion. Although not always linked to airflow obstruction, this is a feature of chronic bronchitis, and not all COPD patients experience clinical mucus hypersecretion.
Squamous metaplasia, a rise in goblet cells, and enlarged bronchial submucosal glands are the causes of the hypersecretion, which is caused by persistent irritation by harmful particles and gases. Squamous metaplasia of epithelial cells causes ciliary malfunction, which manifests as an aberrant mucociliary escalator and difficulties expectorating.
Blockage of airflow and air trapping or hyperinflation
The tiny conducting airways with a diameter of less than 2 mm are the primary location of airflow restriction. This is due to inflammatory exudates in the tiny airways, as well as irritation and narrowing (airway remodeling). Loss of lung elastic recoil (caused by alveolar wall disintegration) and alveolar support (caused by alveolar attachments) are additional variables that contribute to airflow blockage.
During expiration, the airway blockage gradually traps air, causing resting hyperinflation and active hyperinflation during exercise. During exercise, hyperinflation lowers the inspiratory capacity and, consequently, the functional residual capacity. These characteristics lead to the dyspnea and restricted exercise ability that are characteristic of COPD. Spirometry is the most accurate way to measure airflow obstruction in COPD, and it is a requirement for the diagnosis of the condition.
Abnormalities in gas exchange
They are characterized by arterial hypoxemia with or no hypercapnia and arise in advanced illness. The primary mechanism for improper gas exchange is an aberrant distribution of ventilation: perfusion ratios, which is caused by the structural alterations present in COPD. There is a strong correlation between the severity of emphysema and the degree of impairment of the diffusing capacity of carbon monoxide per liter of lung volume.
Hypertension in the lungs
This appears when major problems in gas exchange occur late in COPD. Endothelial dysfunction, pulmonary arterial remodeling (hypertrophy and hyperplasia of smooth muscles), pulmonary arterial constriction (due to hypoxia), and pulmonary capillary bed degradation are all contributing factors. Persistent hypertension of the lungs and right ventricular hyperactivity or enlargement and function (cor pulmonale) are caused by structural alterations in the pulmonary arterioles.
Chronic obstructive lung disease types
Emphysema and chronic bronchitis are also included in COPD. Both traits are frequently present in people with COPD.
When your alveoli get destroyed and expanded, you get emphysema. The most common symptom is dyspnea, or shortness of breath.
Your big airways get inflamed when you have chronic bronchitis. This causes your airways to narrow and produces a lot of mucus. The most typical symptom is coughing.
Chronic bronchitis
- Although the phrase “chronic bronchitis” may still be used, chronic obstructive pulmonary disease (COPD) is the most correct word today. Only a few individuals have chronic bronchitis without the airway blockage (obstruction) of COPD.
- An inflammation of the trachea, bronchi, or bronchioles in your lungs is known as chronic bronchitis. For two years or more, people with chronic bronchitis have symptoms including coughing and shortness of breath most days of the month, three months of the year.
- A virus, such as the flu or the common cold, is typically the cause of acute bronchitis. From just a few days to a few weeks, it lasts. When you experience bronchitis symptoms on a regular basis for two years or more, you have chronic bronchitis. Usually, smoke or other irritating substances for the lungs are the culprit.
People who smoke or used to smoke are frequently affected by chronic bronchitis, or COPD, but you may also be at risk if you:
- Are in close proximity to a smoker.
- Are regularly exposed to dust, chemicals, or air pollution.
- Suffer with asthma.
- Frequent coughing and feeling short of breath due to lung damage is known as chronic bronchitis.
- Your immune system reacts to irritation of your airways, causing them to expand and fill with mucus.
Although bronchitis is usually transient, recurrent irritation of the airways (such as through cigarette smoke or air pollution) can lead to damage that produces an excess of mucus-producing cells (goblet cells). Furthermore, cilia—tiny, hair-like structures—that remove mucus can occasionally malfunction. Your airways enlarge and frequently fill with mucus as a result of this injury. They cough and have breathing difficulties as a result.
Additionally, you have an increased risk of developing bacterial and viral lung infections, which can exacerbate your symptoms.
What is emphysema?
- Destruction to the walls of your lungs’ alveoli causes emphysema, a lung condition. It’s possible for an obstruction to form, trapping air in your lungs. Your chest may seem larger or barrel-chested if there is excessive air trapped in your lungs. Less oxygen enters your bloodstream when your alveoli are smaller.
- Deep within your lungs, at the tip of your bronchial tubes (airways), are clusters of tiny, delicate air sacs called alveoli. About three hundred million alveoli make up a normal set of lungs. The air goes through the bronchial tubes as you inhale, eventually arriving at the alveoli. The alveoli expand, take in oxygen, and deliver it to your blood once the air reaches it. Your alveoli contract when you exhale, forcing carbon dioxide from your body.
- Your lungs are like bubble wrap. Single bubbles in the bubble wrap are analogous to the alveoli. Your alveoli will eventually burst if you have emphysema. You create a giant air pocket, similar to a large shipping air pillow, in place of several tiny bubble wrap bubbles. This damage reduces the total surface area of your lungs, making it more difficult for new air to enter and exit your lungs. You become short of breath and have trouble breathing as a result.
Typically, emphysema appears after years of smoking. But there are additional causes of emphysema. These consist of:
- contaminants in the air at home or at work.
- Alpha-1 antitrypsin insufficiency is one example of a genetic (inherited) component.
- infections of the respiratory system.
- What are the emphysema stages?
- COPD is divided into four stages by the Global Initiative for Chronic Obstructive Lung Disease (GOLD). Although emphysema can cause COPD, not all emphysema patients also have COPD. Medical professionals explain emphysema using the phases of COPD. The phases are:
- The first stage of emphysema is the mildest. Your lungs function at least eighty percent as well as those of a healthy person of the same sex, age, and height.
- Stage 2: This type of emphysema is moderate. Like the normal lungs of a person of the same age, height, and sex, your lungs function between 50% and 79%.
- Severe emphysema is stage 3. Compared to the lung health of a person of the same age, height, and sex, your lungs function between 30% and 49%.
- Emphysema at stage four is really severe. Compared to a healthy person of the same age, height, and sex, your lungs function less than thirty percent as well.
Causes and Symptoms
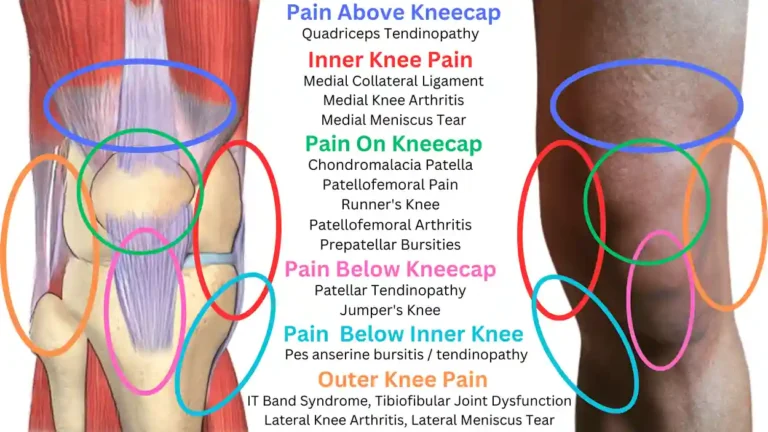
What signs of COPD are present?
COPD symptoms include:
- Cough up mucous that you’ve accumulated for a while (at least two years, three months at a time).
- Inability to inhale deeply.
- Breathlessness, particularly during routine tasks or with light exertion.
- Additional lung noises, such as wheezing.
- Chest fashioned like a barrel.
- Cyanosis (blue skin).
Why does COPD occur?
- The primary cause of COPD is lung damage from smoking. Other reasons are as follows:
- Lung injury may result from alpha-1 antitrypsin deficiency, a hereditary condition.
- Second hand smoke.
- Contamination of the air.
- Dust and fume exposure from your occupation or pastimes.
What are this condition’s risk factors?
- Although the largest associated risk for COPD is smoking, not all smokers will get the disease. You might be more susceptible to COPD if you:
- Are women and above 65 years old.
- Been exposed to pollutants in the air.
- Have dealt with dust, fumes, or chemicals.
- Have a lack of alpha-1 antitrypsin.
- Had numerous childhood respiratory illnesses.
What COPD problems exist?
Infections can result from bacteria being trapped in your lungs by COPD. Additionally, it can stop carbon dioxide from leaving your body and oxygen from entering. Serious issues could result from this, such as:
- Pneumonia.
- Elevated blood carbon dioxide levels (hypercapnia).
- Hypoxemia, or low blood oxygen levels.
- Respiratory malfunction.
- Hypertension of the lungs.
- Heart failure on the right side (cor pulmonale).
- Lung collapse (pneumothorax).
- Making too many red blood cells is known as polycythemia.
Testing and Diagnosis
How can someone be diagnosed with chronic obstructive pulmonary disease (COPD)?
A healthcare professional will examine you and inquire about your medical history in order to diagnose COPD. In addition to testing your lung function, they may take pictures of your lungs.
Which tests are used by medical professionals to diagnose COPD?
Testing for pulmonary function. Spirometry is and other tests can be used by healthcare professionals to assess the function of your lungs.
Oximetry of the pulse: This test measures the amount of oxygen in your blood using an instrument on your finger.
Imaging examinations: CT scans or chest X-rays can check for lung abnormalities caused by COPD.
Test for arterial blood gas: This blood test measures your levels of carbon dioxide and oxygen.
Test your muscles: This is how your doctor determines whether activity causes your blood’s oxygen level to decline.
EKG, or electrocardiogram: This test examines the function of the heart and eliminates heart disease as a potential cause of dyspnea.
blood examinations. To determine whether you may have Alpha-1 antitrypsin deficiency, your healthcare professional may measure your levels of the protein AAT.
Genetic analysis: Your doctor may perform a blood test to look for genetic alterations if they believe a genetic condition may be the source of your lung problems.
What phases does COPD go through?
The results from your forced expiratory volume in one second (FEV1) might be used by your healthcare professional to stage COPD. Your FEV1 can inform your doctor how restricted your airways are because it measures how much air you can exhale in a second. Your provider uses spirometry to determine FEV1.
The severity-based COPD phases are:
- FEV1 is 80 or higher in stage 1.
- Stage 2: FEV1 ranges from 50 to 79.
- Stage 3: FEV1 ranges from 30 to 49.
- FEV1 is less than 30 in stage four.
- Additionally, your provider can use groups with the numbers A, B, and E to assess your symptoms and risk of exacerbation:
A: Your symptoms are minor, and there is little chance that they will worsen.
B: You are less likely to experience exacerbations and your symptoms are more severe.
E: Your risk of exacerbations is high.
Your symptoms aren’t always correlated with your stage; for example, you may be in stage 3 or 4, yet still have minor symptoms. Your stage, symptoms, and frequency of exacerbations can all be used by your healthcare professional to inform your course of treatment.
Handling and Therapy
What is the treatment for COPD?
COPD has no known cure. Reducing your symptoms and preventing and managing exacerbations are the main goals of treatment. Your healthcare practitioner might suggest:
Programs to help people stop smoking. The development of COPD can be slowed down by quitting smoking.
Inhaled drugs: Steroids and bronchodilators help expand your airways and lessen inflammation. These may be available as a liquid to use in a nebulizer or as an inhaler.
Oxygen treatment: To raise your oxygen levels, you could require more oxygen.
Rehabilitation for the lungs: This regimen of information and exercise will help you manage COPD and improve your lungs.
Corticosteroids: During an exacerbation, you may require a course of steroids to alleviate inflammation.
Positive airway pressure: To assist you breathe, particularly during an exacerbation, your doctor may prescribe a BiPAP machine.
antibiotics.
Your doctor can recommend antibiotics if you frequently get bacterial lung infections in order to stop infections and flare-ups.
Lowering of lung volume (LVR): Your doctor might recommend surgery or a valve operation that lowers the amount of air trapped in your lungs if you have severe COPD and are a good candidate.
Clinical experiments: New medicines are tested in clinical trials to determine their efficacy and safety. If a new treatment seems like a good fit, your provider may suggest one.
rehabilitation for the lungs. Exercises and other techniques to help you breathe more easily and enhance your quality of life are taught in pulmonary rehabilitation.
Steroids.: To lessen inflammation, your doctor may recommend corticosteroids, either as a tablet or in an inhaler.
Surgery to reduce lung volume (LVRS): A section of your damaged lung tissue is removed during LVRS, and the remaining tissue is joined together. By removing the damaged tissue, you may be able to enhance the flexibility of your lungs and reduce pressure on your breathing muscles. Results from LVRS are often encouraging. But not every emphysema patient is a good candidate for this procedure.
Lowering of lung volume by bronchoscopy: A clinician inserts a one-way valve into your airways during a bronchoscopic lung volume reduction procedure. Air can exit those parts of your lungs through the valve, but it cannot enter. By decreasing the amount of “trapped” air in your lungs, this makes breathing easier. This treatment is not appropriate for all emphysema patients.
Prevention
Is it possible to prevent COPD?
Avoiding smoking, secondhand smoke, and other lung-damaging pollutants is the greatest method to prevent COPD.
Respiratory infections are more common in people with COPD, and they can cause significant exacerbations of symptoms or even pneumonia. You can lower your chance of contracting illnesses by:
Getting all the recommended immunizations, such as those for COVID-19,
- pnumococcal pneumonia, and the flu.
- frequently washing your hands.
- Cleaning surfaces.
- If your healthcare physician advises it, wearing a mask around other people.
- Avoiding busy areas, particularly when COVID instances are high and the cold and flu seasons are upon us.
How can someone with COPD take care of themselves?
Here are some self-care suggestions for people with COPD:
- Avoid anything that exacerbates your symptoms, including lung irritants. This includes dust, air pollution, smoking, secondhand smoke, and overpowering scents.
- Attend programs for pulmonary rehabilitation. This covers education sessions as well as occupational and physical therapy. Even when your sessions are over, stick to the strategy they provide.
- Speak with a certified dietitian. They can advise you on which things to eat or stay away from in order to maintain your health.
- As directed, take all of your prescription drugs. Before you run out, make sure you have your daily prescriptions on hand.
- Prepare yourself for flare-ups. Create a plan with your healthcare professional about what to do in the event of an exacerbation. This could entail knowing when to visit the hospital and keeping specific prescriptions on hand.
- Understand how to operate your medical equipment. This can include CPAP machines, nebulizers, inhalers, and other equipment. Request that your provider illustrate proper usage.
- Look after your emotional well-being. It might be detrimental to your mental health to have a chronic condition. You can manage social, emotional, and other mental health concerns with the assistance of a mental health professional, such as a psychiatrist, psychologist, or counselor.
COPD Physical Therapy
Individuals experiencing chronic obstructive pulmonary disease (COPD) can benefit from physical therapy.
Physical Therapy for respiratory disorders
Breathing can be challenging if you have lung illness.
Common issues may include the following, based on the type of lung disease:
- Breathlessness is the inability to effectively breathe.
- Difficulty supplying oxygen to your body or surrounding tissues, an accumulation of phlegm fluid in your lungs,
- Development of a tumor within or near your lungs
- You may find it more difficult to walk, exercise, and carry out daily tasks as a result of these issues.
Physical therapy employs a variety of methods to address these issues.
You will discuss your problem and symptoms with your Physical Therapist.
How you are treated will depend on:
- your health, your symptoms, and your ability to handle the projected course of therapy for your illness or disease
- Plan of treatment
Together, you and your Physical Therapist will create a treatment plan that could involve:
Breathing exercises are methods to help clear mucus or phlegm manually or to lessen shortness of breath. To aid in lung expansion and phlegm clearance, use vibrations and percussion to release mucus or phlegm placement.
Enhancing exercise and fitness education and self-management; providing guidance on the use of inhalers, nebulizers, and oxygen prescriptions; offering guidance and instruction on the use of devices to help clear your airway or lung volume loss; and offering pulmonary rehabilitation sessions in both community and hospital settings
Exercises for Breathing with COPD
- Shortness of breath is one of the symptoms of chronic obstructive pulmonary disease (COPD) that breathing exercises can help you manage.
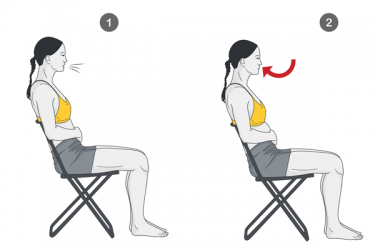
- Try the huff cough and pursed lip breathing as exercises.
- Pursed lips breathing exercise
- synchronized breathing
- Deep breathing Exercises
- coughing, huffing, and diaphragmatic breathing
Breathing with pursed lips

- The following are some advantages of pursed lip breathing:
- lowering dyspnea, boosting lung airflow, promoting relaxation, and expelling air that has been trapped in the lungs.
- Using this method four to five times a day can be beneficial. Use these procedures to practice pursed lip breathing:
- Breathe deeply via your nose while counting to two, keeping your mouth shut. Repeat the following sequence in your mind: “Inhale, 1, 2.” It is not necessary to take a deep breath. A normal breath will suffice.
- Press your lips together as if you were blowing out the candles on a birthday cake or beginning to whistle. It’s called “pursing” your lips.
- Breathe out slowly while keeping your lips pursed and counting to four. Avoid trying to expel the air. Breathe through your mouth slowly.
Synchronized breathing
- Anxiety caused by shortness of breath can drive you to hold your breath. You can use these two strategies to learn synchronized breathing and avoid this:
- Before starting a workout, take a breath through your nose.
- During the hardest portion of the workout, exhale through your mouth while pursing your lips. Curling upward on a bicep curl could serve as an illustration.
Deep breathing

- Breathing deeply helps keep air from becoming stuck in the lungs, which can make you feel out of breath. You are able to take in more fresh air as a result.
- To practice deep breathing, follow these steps:
- Keep the elbows slightly back while standing or sitting. Your chest can enlarge more completely as a result.
- Take a deep breath through your nose.
- Hold your breath while you count to five.
- Exhale slowly and deeply through your nostrils until you feel as though the air you’ve breathed has been expelled.
Coughing huff
- Mucus might accumulate in your lungs more readily if you have COPD. The purpose of the puff cough is to assist you cough out mucus efficiently with making you feel overly exhausted.
- The puff cough can be practiced as follows:
- Ensure that you are sitting comfortably. Breathe in through your mouth, a little wider than you would normally do.
- Make the sounds “ha, ha, ha” while you contract your abdominal muscles to expel the air in three even breaths. To make a mirror steam, picture blowing upon it.
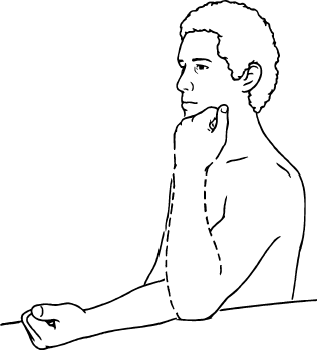
Diaphragmatic breathing
- The primary breathing muscle is the diaphragm.
- In order to breathe, people with COPD typically use their neck, shoulders, and lower back auxiliary muscles more than their diaphragm.
- Abdominal or diaphragmatic breathing aids in retraining this muscle to function better. Here’s how to accomplish it:
- Place one hand on your chest and the other on your stomach when you are sitting or lying down with your shoulders relaxed.
- For two seconds, inhale through your nose while feeling your tummy expand. If your tummy moves more than your chest, you’re performing the exercise correctly.
- Gently press your tummy against your lips while you exhale gently through your mouth. This will improve the air-release capacity of your diaphragm.
- Do the exercise as many times as you can.
Conclusion
- Shortness of breath and tightness in the chest are two symptoms of COPD that breathing exercises can frequently assist you alleviate.
- Deep breathing and pursed lips are examples of slow, focused activities that may assist you recover from physical activity and enhance your daily quality of life.
FAQs
Does COPD pose a threat to life?
Despite being fatal, COPD and oxygen deprivation are not the exclusive causes of death. Cardiovascular disease is one of the numerous medical issues that some persons with COPD suffer. Within five years of diagnosis, COPD is also a risk associated with sudden cardiac mortality on its own.
What is the etiology of COPD?
Smoking. The primary cause of COPD, which is believed to be caused by smoking in about 90% of cases, is smoking. Smoke contains dangerous compounds that can destroy the outer layer of the airways and lungs. Quitting smoking can help stop the progression of COPD.
Which four phases of COPD are there?
COPD can be divided into four stages: moderate, severe, mild, and extremely severe. The findings of a breathing test known as a spirometry, which evaluates lung function through determining the amount of air you can breathe in and out and the speed at which you can exhale, will be used by your doctor to identify your stage.
Which medication works best for COPD?
Inhalers with short-acting bronchodilator are the initial treatment for the majority of COPD patients. Bronchodilators are medications that relax and enlarge your airways to facilitate breathing. Short-acting bronchodilator inhalers come in two varieties: beta-2 agonists, which include terbutaline and salbutamol.
What is lung function physical therapy?
The methods and tools utilized in chest physical therapy are designed to facilitate the removal of thick, sticky, or extra mucus from the lungs. Some of these methods use vibration or percussion (force) to break up the mucus in the affected lung area.
Which breathing technique is most effective for those with COPD?
Inhale as deeply as you can, slowly, via your nose. Slowly exhale through pursed lips. Tighten the muscles directly beneath your ribs as you exhale. As you tighten the muscles, softly push in and up with your hand.
Can breathing techniques help people with COPD?
Are you having trouble breathing because of COPD? You can manage shortness of breath and take in air more easily by strengthening the muscles that you use to breathe with simple workouts.
Will walking help people with COPD?
When you have COPD, exercise can help you breathe better and manage some of your symptoms. Joining a singing or walking group is beneficial for many people.
Reference
- World Health Organization: WHO & World Health Organization: WHO. (2024b, November 6). Chronic obstructive pulmonary disease (COPD). https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- Chronic Obstructive pulmonary Disease (COPD). (2025, February 9). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8709-chronic-obstructive-pulmonary-disease-copd
- Chronic bronchitis. (2024, December 3). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24645-chronic-bronchitis
- Emphysema. (2025, February 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9370-emphysema
- Physical therapy for COPD. (n.d.). HSE.ie. https://www2.hse.ie/conditions/copd/physical therapy-for-copd/
- Crna, R. N. M. (2023, July 17). Breathing Exercises with COPD. Healthline. https://www.healthline.com/health/copd/breathing-exercises#conclusion





3 Comments