Chronic Bronchitis
What is a Chronic Bronchitis?
Chronic bronchitis (CB) is a persistent cough and sputum production that lasts for at least three months out of the year for two years in a row.
A form of COPD called chronic bronchitis causes your lungs to become inflamed and fill with mucus. Although chronic bronchitis cannot be completely cured, it can be controlled with medication. Smoking is nearly always the cause.
An inflammation of your lungs’ trachea, bronchi, or bronchioles is known as chronic bronchitis. For two years or more, people with chronic bronchitis experience symptoms like coughing and shortness of breath on most days of the month, three months out of the year.
Chronic obstructive pulmonary disease (COPD) is frequently referred to as chronic bronchitis. The phrase “chronic bronchitis” may still be used, but it is now more appropriately referred to as COPD. Only a small percentage of people with chronic bronchitis do not also have COPD-related airway blockage.
Who is affected by chronic bronchitis?
Chronic bronchitis, or COPD, is common in smokers and former smokers, but you may also be at risk if:
- You are in close contact with a smoker.
- You are regularly exposed to dust, chemicals, or air pollution.
- You suffer from asthma.
Epidemiology
The incidence of chronic bronchitis:
It has been reported that between 3% and 7% of healthy adults in the general population have it.
Up to 74% of people with a COPD diagnosis are thought to have it.
Individuals with chronic bronchitis under 50 who are otherwise healthy are more likely to experience morbidity and death than healthy subjects.
Chronic bronchitis is believed to be more common as people age, smoke, are exposed to tobacco at work, and have a higher socioeconomic status.
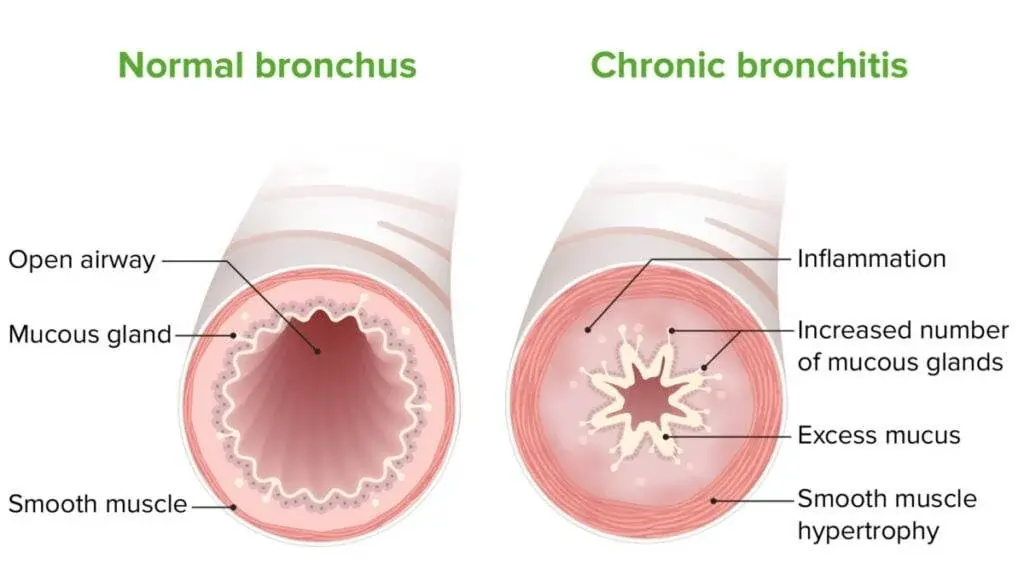
Pathophysiology
Goblet cells are thought to produce and secrete too much mucus, which results in chronic bronchitis. The airway’s epithelial cells react to harmful and infectious stimuli by releasing pro-inflammatory cytokines and other inflammatory mediators.
An acute episodes of chronic bronchitis results in decreased bronchial muco-ciliary function and hyperemic and edematous bronchial mucous membranes. Consequently, luminal blockage of small airways results in airflow obstruction.
Debris blocks the airways, which worsens the irritation. The excessive mucus secretion in chronic bronchitis is the reason that causes the typical cough of bronchitis.
There were more goblet cells in the peripheral airways of smokers with moderate COPD and CB, which raises the possibility of mucus in the lungs (the more small airways blocked with mucus, the more severe the disease).
Chronic bronchitis in adults is triggered by exposure to cigarette smoke, recurrent or chronic bacterial and viral infections, or toxic environmental exposures. Inflammatory and humoral mediators also trigger the release of mucin to protect the airway from harmful stimuli. Furthermore, the transcription of the mucin gene is triggered by inflammatory cells activating the epidermal growth factor receptor (EGFR).
The increased activation and degranulation of neutrophils as a result of neutrophil-mediated elastase causes an excess of mucus to be produced and secreted.
Mucus hypersecretion is primarily caused by EGFR receptor expression and activation, with activated neutrophil involvement playing a crucial role. Macrophages eliminate neutrophils that go through apoptosis in healthy people.
The airway conditions in patients with COPD or chronic bronchitis cause neutrophils to necrotize and release their intracellular contents, which raises the levels of elastase and reactive oxygen species in the sputum.
Tumor necrosis factor (TNF)-α, which is secreted by activated neutrophils that have been obtained to the airways, raises the expression of EGFR in airway epithelial cells and releases reactive oxygen species that directly activate EGFR.
In order to activate EGFR in a ligand-dependent manner, neutrophil elastase also breaks down the EGFR proligand, pro-transforming growth factor (TGF)-α, releasing mature TGF-α. Mucus hypersecretion gets worse by neutrophil elastase, which also causes strong goblet cell degranulation.
Because of mucus hypersecretion and the thickening of the epithelial cell layer, mucous metaplasia restricts airflow. Furthermore, too much mucus changes the surface tension of the airways, making them more susceptible to expiratory collapse.
Infection and inflammation of the airways result from inadequate mucus clearance. Regardless of smoking status, a persistent cough and sputum production raise the risk of developing COPD.
Investigation indicates that individuals under 50 years of age who have chronic bronchitis without airflow restriction are more likely to develop COPD and die from all causes.
The lung’s defenses are weakened in children by early abuse such as bacterial pneumonia or viral infections, which results in bacterial overgrowth, most likely in a biofilm, which is decreased mucociliary clearance, and excessive mucus production.
Microbes on the surface of a biofilm are covered in a matrix of extracellular polymeric substances that promotes bacterial persistence and shields the bacteria from antibiotics, requiring long-term antibiotic treatment.
Maternal and childhood influences, as well as genetic and environmental factors, are important.
For example, exposure to air pollution or tobacco smoke worsens mucosal dysfunction and airway inflammation, which encourages the growth of bacteria.
One of the risks of exposure to cigarette smoke, bacterial, viral, or inflammatory cell activation is mucus hypersecretion. Clearing secretions is very difficult and energy-intensive when accompanied by weak respiratory muscles, distal airway occlusion, ineffective coughing, poor ciliary function, and decreased peak expiratory flow.
Risk factors for chronic bronchitis
Risk factors for chronic bronchitis include the following:
- Smoking: This is the primary risk factor. Smoking or former smoking is a factor in up to 75% of cases of chronic bronchitis.
- Prolonged exposure to additional lung irritants, including air pollution, secondhand smoke, and dust and fumes from chemicals in the environment or at work.
- Age: The majority of people with chronic bronchitis start experiencing symptoms when they are at least 40 years old.
- Genetics: One of these is alpha-1 antitrypsin deficiency, a genetic disorder. Additionally, smokers with a family history of chronic obstructive pulmonary disease (COPD) are at a higher risk of developing chronic bronchitis.
Causes
The causes of chronic bronchitis are numerous.
Cigarette smoke exposure, whether from active smoking or passive inhalation, is the primary contributing factor. Other reasons are as follows:
- Chronic bronchitis can be caused by inhaled respiratory tract irritants such as smoke, industrial pollutants, and airborne chemicals like sulfur and ammonia.
- Chronic bronchitis can be caused by repeated exposure to viral infections.
- Chronic bronchitis is more likely to develop in people with a history of respiratory conditions such as asthma, cystic fibrosis, or bronchiectasis.
- Although it is less common, chronic gastroesophageal reflux is a well-established cause of chronic bronchitis.
- Another genetic component associated with COPD is a deficiency in alpha-1-antitrypsin. Although many patients on the COPD spectrum exhibit characteristics of both Emphysema and Chronic Bronchitis, this genetic marker is suggestive of Emphysema.
Signs and symptoms
Signs and symptoms may include:
- Mucus production
- coughing
- Fatigue
- chest pain
- Breathlessness
- Disability
- Airway infections that are severe and frequent
- Narrowing and blockage of breathing tubes (bronchi)
Other symptoms may include:
- Reduced oxygen levels can cause bluish skin, lips, and fingernails.
- Wheezing and crackling sounds with breathing
- Swollen feet
- Heart failure
A productive cough lasting at least three months with recurrent episodes lasting at least two years is commonly referred to as chronic bronchitis. There will probably be times when your cough or other symptoms get worse if you have chronic bronchitis. Additionally, acute infection can coexist with chronic bronchitis.
Complications
A single round of bronchitis is usually not a serious condition, but in certain cases, it can result in pneumonia. However, recurrent episodes of bronchitis could indicate chronic obstructive pulmonary disease (COPD).
Prevention
Use the following tips to lower your risk of developing bronchitis:
Obtain a yearly flu vaccination: A virus called influenza causes a lot of cases of acute bronchitis. You can avoid having the flu by getting vaccinated every year. Additionally, find out from your physician or clinic if you require a vaccination to prevent specific forms of pneumonia.
Clean your hands: Use alcohol-based hand sanitizers and wash your hands often to lower your risk of contracting a viral infection. Additionally, avoid touching your mouth, nose, or eyes.
Avoid close contact with individuals who are infected with a virus: Avoid contact with those who are ill with the flu or another respiratory disease.
Avoid cigarette smoke: The risk of developing chronic bronchitis is increased by cigarette smoke.
Put on the proper face covering: If you are exposed to dust or fumes at work and you have COPD, you might want to think about wearing a face mask.
Discuss the proper protection with your supervisor: When you’re going to be around crowds, wearing a face mask helps lower your risk of contracting an infection.
Is it possible to spread chronic bronchitis?
COPD, or chronic bronchitis, is not communicable. Contagious illnesses like the flu or a cold, however, may increase the likelihood that your symptoms of chronic bronchitis will worsen.
Testing and Diagnosis
How is chronic bronchitis diagnosed?
A medical professional will assess your lung function to diagnose chronic bronchitis, also known as COPD. They will listen to your heart and lungs and inquire about your medical history and symptoms. In addition to testing your lung function, they may prescribe imaging tests, such as chest X-rays.
Which tests will be conducted?
Among the tests for chronic bronchitis are:
Tests for pulmonary function: Your doctor can get a sense of how well your lungs are functioning by performing pulmonary function tests. If your doctor believes you have chronic bronchitis, they may perform a common lung function test called spirometry.
Spirometry. A spirometer is used in this test to measure the function of your lungs. It’s among the most straightforward and widely used pulmonary function tests. It can be applied to any or all of the following purposes:
- To assess the efficiency of your lungs’ air intake, retention, and movement
- To monitor a lung condition
- To assess the effectiveness of the treatment
- To determine the severity of your lung condition
- To determine whether your lung condition is obstructive or restrictive. Less air will enter your lungs if it’s restrictive. Less air will exit your lungs if it’s obstructed.
Peak flow monitor: The fastest rate at which you can exhale air is measured by this test. The lungs’ large airways are constricted by mucus and inflammation. As a result, air leaves the lungs more slowly. A peak flow monitor is able to measure it. This metric is crucial for determining how effectively your illness is being managed.
Arterial blood gas: The purpose of this blood test is to measure the levels of carbon dioxide and oxygen in your blood. Additionally, it measures how acidic your blood is.
Pulse oximetry: A tiny device called an oximeter measures how much oxygen is in your blood. A tiny sensor is attached to a finger or toe with tape or a clip in order to obtain this measurement. A tiny red light appears in the sensor when the machine is turned on. The red light doesn’t get hot, and the sensor doesn’t hurt.
CT scan or chest X-ray: Your doctor can use imaging to determine whether your lungs are damaged or have any areas of concern. Your heart and lungs will be observed by a machine. They will search for indications of illnesses that might be the source of your symptoms.
Blood examinations: To assess your general health, your doctor might perform blood tests, which involve inserting a needle into your arm. An arterial blood gas test, a specialized blood test drawn from the artery in your forearm, might be performed. This measures the amount of carbon dioxide and oxygen in your blood.
EKG, or electrocardiogram: An ECG or EKG may be used by your healthcare provider to assess the function of your heart.
Differential Diagnosis
Other differential diagnoses to take into consideration when assessing chronic bronchitis include:
- Acute bronchitis
- Acute sinusitis
- Alpha-1 antitrypsin (ATT) deficiency
- Asthma
- Bacterial pharyngitis
- Bronchiectasis
- Bronchiolitis
- Bronchomalacia
- Chronic sinusitis
- COPD
- Cystic fibrosis
- Diffuse panbronchiolitis
- Endemic fungal and parasitic infections
- Gastroesophageal reflux disease
- Immunodeficiency
- Influenza
- Lung cancer
- Medication effects
- Obstruction or anatomic abnormality in the airway
- Obstructive sleep apnea
- Pertussis
- Pneumonia
- Postinfectious cough
- Primary ciliary dyskinesia
- Pulmonary fibrosis
- Heart failure
- Tracheomalacia
- Tuberculosis
- Upper airway cough syndrome
Treatment
How can chronic bronchitis be treated?
Symptom management is the main goal of treatment for chronic bronchitis/COPD. Various forms of therapy may be recommended by your provider based on the severity of your symptoms, such as:
Smoking cessation: You can improve your breathing and prevent the worsening of chronic bronchitis by giving up smoking.
Bronchodilators: Bronchodilators are medications that facilitate airway opening. To take them, you typically use an inhaler.
Steroids: Your physician may recommend corticosteroids, either as a pill or in an inhaler, to help lower inflammation.
Pulmonary rehabilitation: Exercises and other techniques for improving breathing and your quality of life are taught during pulmonary rehabilitation.

Oxygen treatment: You might not be getting enough oxygen if your chronic bronchitis is severe. Through a tube in your nose or a mask on your face, oxygen therapy provides additional oxygen.
Antibiotics: When your healthcare provider suspects an infection, they may prescribe antibiotics because chronic bronchitis can make you more prone to illness.
Lung transplant: You might live longer if you get a new lung or lungs.
Physical therapy
The physical therapist should help with sputum clearance, enhance thoracic mobility and lung volume, decrease worsening symptoms and hospitalization, improve exercise tolerance, and provide education.
Treatment for chronic bronchitis includes both respiratory physical therapy and pulmonary rehabilitation.
Education
Morbidity and quality of life are greatly affected by chronic bronchitis. The psychological effects of having a chronic condition may be lessened and an active approach to management may be encouraged if the treating clinical staff educates the person with CB about the presenting condition, medication use, treatment options, and self-management.
Stop smoking is the most important nonpharmacological intervention. Smoking cessation reduces goblet cell hyperplasia and enhances muco-ciliary function. It has also been demonstrated that quitting smoking lessens airway damage, which lowers the amount of exfoliated mucus in tracheobronchial cells.
Exercise
The prevention, management, and treatment of CB and COPD can all benefit from regular exercise. Aerobic exercise and upper and lower limb resistance training have been shown to improve sputum expectoration, airway clearance, reduced airflow blockage, improved functional abilities, and increased energy levels.
Before beginning any exercise program, a consultation with the general practitioner should be held, and the treating clinical team (such as a physical therapist) should oversee the program.
Physical Fitness
Aerobic exercise and resistance training for the upper and lower limbs can decrease hospitalizations, worsening, and dyspnea while increasing energy, functional tolerance, and physical fitness. Particular suggestions are made regarding exercise for people with COPD and chronic bronchitis. Before beginning any exercise program, a discussion with the treating clinical team should be held.
Avoiding irritants
Reducing risk factors and exacerbations of chronic bronchitis can be achieved by being mindful of potential irritants in the home, workplace, and recreational areas. Air pollution, smoke, chemicals, dust, and vapors are some examples of irritants to be mindful of. If occupational contact with irritants is frequent, it is important to have the appropriate respiratory protective equipment on hand.
Practice Proper Hygiene
Maintaining proper hygiene can prevent bacteria, infections, and germs from spreading. As a result, bronchitis risk factors and chronic bronchitis exacerbations may be lessened.
Prognosis
There is no cure for chronic bronchitis. The damage to your lungs is irreversible and typically worsens with time. The bad news is that the disease has varying effects on different people. It’s possible that your chronic bronchitis is not severe.
If your doctor detects the illness early, numerous treatment options can reduce symptoms, slow the progression of the disease, and keep you out of the hospital. You may be able to live a long, comfortable, and healthy life with treatment. Quitting smoking and sticking to your treatment plan are the best things you can do for yourself.
FAQs
Can someone with chronic bronchitis lead a full life?
In addition to reducing symptoms, medication and lifestyle modifications can prevent or slow the progression of chronic bronchitis. Many people breathe on their own without the need for additional oxygen and have moderate symptoms for a long time.
Can your lungs be harmed by bronchitis?
The severity of chronic bronchitis/COPD can range from mild to severe. It typically indicates lung damage, which can worsen over time. Although there is no way to repair the damage, your healthcare provider can help you control your symptoms, delay its progression, and lessen flare-ups.
Can someone with chronic bronchitis lead a full life?
In addition to reducing symptoms, medication and lifestyle modifications can prevent or slow the progression of chronic bronchitis. Many people breathe on their own without the need for additional oxygen and have moderate symptoms for a long time.
Can pneumonia develop from bronchitis?
A single episode of bronchitis is usually not a serious condition, but in certain cases, it can result in pneumonia. However, recurrent episodes of bronchitis could indicate chronic obstructive pulmonary disease (COPD).
Is chronic bronchitis irreversible?
The majority of people with COPD also have emphysema and chronic bronchitis. Breathing becomes difficult with these conditions, and they get worse over time. In contrast to acute bronchitis, COPD and chronic bronchitis are incurable. You can still take action to control symptoms and slow the course of the illness.
How can someone with bronchitis sleep?
Lying on your back with your head up is the ideal sleeping position for treating bronchitis. Breathing becomes easier and mucus buildup in the throat can be avoided by using additional pillows to support your head and upper body.
Which tea helps treat bronchitis?
The thyme herb plant is used to make thyme tea, which is an excellent remedy for coughing and congestion. Thyme tea helped treat acute bronchitis with a productive cough in a recent study. According to the findings, patients who drank this tea recovered from their coughs more quickly than those who took a placebo.
References
- Widysanto, A., Goldin, J., & Mathew, G. (2025, February 6). Chronic bronchitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482437/
- Chronic bronchitis. (2024b, December 3). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24645-chronic-bronchitis#management-and-treatment
- Chronic bronchitis. (n.d.). WebMD. https://www.webmd.com/lung/copd/copd-chronic-bronchitis
- Chronic bronchitis. (2024a, August 22). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-bronchitis