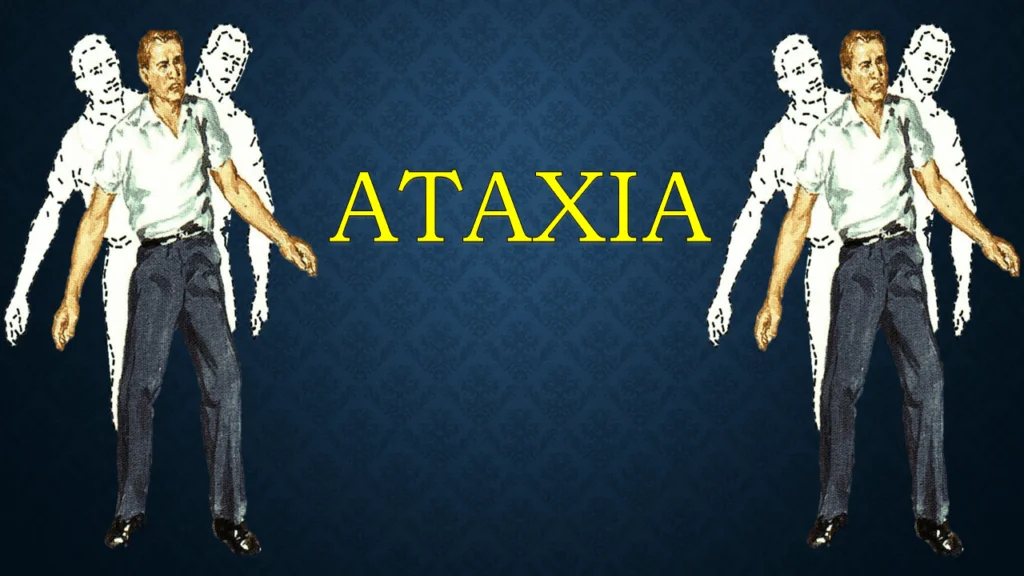
Ataxia
Ataxia: What is it?
Ataxia is the concept of a condition affecting your body’s coordination. You might move strangely if you have ataxia. Ataxia affects the cerebellum, the inner ear, and other elements of the central nervous system responsible for communicating muscle movements.
Ataxia may indicate a specific aliment or be the name of a group of related disorders.
The illness known as ataxia is less common and is frequently caused by a particular genetic mutation.
Atherosclerosis affects the coordination required for mouth, eyes, limbs, balance, and movement. It might manifest as a single condition or symptom of many other disorders.
Numerous factors, such as genetic alterations, trauma, inflammation, stroke, tumors, and infections, might contribute to ataxia symptoms. Depending on the underlying reason, ataxia may be treated or even reversed.
What distinguishes apraxia and ataxia from one another?
In addition to having similar sounds, ataxia and apraxia have numerous properties.
Apraxia: This brain disorder makes it difficult for you to do or explain tasks that you are already familiar with. It occurs as a result of an issue with how your brain interprets these movements.
Ataxia is a condition that inhibits muscle coordination, affecting all actions (known or novel). The tasks have no trouble at all being processed or described by your brain.
What causes ataxia?
Ataxia can be:
- inherited
- acquired
- idiopathic
Hereditary ataxia:
Two main methods are usually used to transmit inherited ataxia:
- Dominant: The condition can only exist in one mutant gene copy. Grandchildren of any parent can inherit the gene in question.
- Regarding recessive illnesses, two defective copies of the chromosome must be present, one coming from every pair of parents.
Here are a few instances of dominant hereditary ataxia:
Spinocerebellar ataxia: Numerous variations exist within the category of spinocerebellar ataxia. Each kind is defined based on the exact location of the altered gene.
Episodic ataxia: This kind of ataxia happens in spurts rather than gradually. It has been eight major forms of fluctuating ataxia.
Among the recessive inherited ataxia are:
Friedreich’s ataxia, or spinocerebellar degenerative alterations, is perhaps the most frequent kind of genetic ataxia. Not only might speech and movement problems arise, but muscular weakness can also happen. The heart may be impacted by this kind of ataxia as well.
Ataxia telangiectasia.Ocular and cheek blood vessel constriction is a common symptom in ataxia-telangiectasia patients. Along with the symptoms of traditional ataxia, those who have this kind of ataxia are also at higher risk of infections and cancers.
Acquired causes:
alcoholic beverages. Chronic overindulgence in alcohol may result in chronic ataxia.
medications. One possible adverse effect of some medications is ataxia. Furthermore, anti-seizure drugs, specifically phenytoin, may be the cause. Ataxia is another unfavorable effect of various chemotherapy treatments.
toxic substances. Exposure to heavy metal poisoning, such as lead or mercury, and solvent toxicity, such as paint thinner poisoning, can also cause ataxia.
An excessive or insufficient amount of a specific vitamin. A lack of vitamin B-1, vitamin B-12, or vitamin E, occasionally referred to as thiamine, can cause ataxia. A person who does not get enough of a particular vitamin is said to have a vitamin deficit. Ataxia can frequently be treated when a vitamin deficit is the underlying cause.
Thyroid conditions. A hypothyroid or hypoparathyroid state may cause ataxia.
stroke. Following a stroke, ataxia can appear suddenly. Either cerebral hemorrhage or a blood vessel obstruction could be the cause of this.
Multiple sclerosis. Ataxia could result from this illness.
illnesses triggered by antibodies. Atherosclerosis can be brought on by several autoimmune illnesses, conditions where the body’s defenses target healthy cells. One condition that might lead to an accumulation of inflammatory cells in particular body parts is sarcoidosis. Alternatively, they could involve abdominal disease, a condition brought on by the body’s immune system reacting to gluten.
bacterial infections. Rarely, ataxia can indicate the presence of a viral disease like HIV, lymphoma, or childhood chickenpox. It could appear through the healing stage of the bacterial infection and last for a few days or weeks. Usually, the symptom improves with time.
The syndromes of paraneoplastics. These uncommon degenerative illnesses are brought on by the immune system’s reaction to a neoplasm, or malignant tumor. Most frequently, lymphomas or cancers of the breast, ovary, or lung cause paraneoplastic syndromes. Before the cancerous growth is discovered, ataxia may manifest for months or even years.
abnormalities in the brain. Furthermore, harm to the cerebellum may result from an amorphous or noncancerous tumor growing on the brain.
head injury. Ataxia may result from brain injury.
cerebral palsy. This umbrella term encompasses a variety of illnesses caused by pediatric brain damage. It affects the child’s ability to coordinate their bodily movements.
Idiopathic or sporadic ataxia:
There are situations where ataxia has no known etiology. We designate sporadic or idiopathic ataxia for these types of conditions.
What signs of ataxia are present?
whichever factors affect the person, several ataxia symptoms may appear.
Typical ataxia symptoms include:
- Difficulties with balancing and coordination
- Having trouble getting around or walking
- deficiency in motor control, manifested in hand, arm, and leg shaking
- difficulties in swallowing or slurred speech
- broad-based gait (walking style)
- Having trouble with writing and eating
- Unintentional motion
- sluggish or strange eye movements
Which three forms of ataxia are there?
Moreover, ataxia can be classified based on the area of the neurological system. Specific ataxia symptoms appear to correspond with the area of nerve injury.
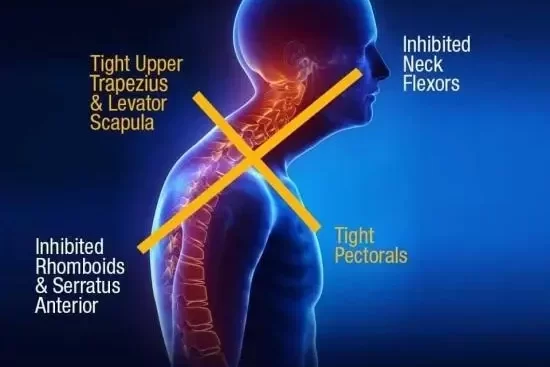
Cerebellar ataxia:
Most ataxias are categorized as “cerebellar,” suggesting a link to the cerebellum. Two subtypes of cerebellar ataxia exist:
The midline contains the major cerebellar region. It has been determined that this area belongs to the midline cerebellum. A midline cerebellar injury may result in issues including tremors during movement, clumsy walking, and altered eyesight.
The “lateral” cerebellum refers to the sections of its anatomy that do not form part of the body. Ataxia symptoms are typically felt on the same side of the body when there is damage to a nerve in the outer region of the cerebellum. Thus, if the left lateral cerebellum is gone, your left side is more likely to have symptoms. Communicating difficulties, trouble assessing the distance when reaching or moving around, and trouble performing swift, synchronized movements are among the most likely signs.
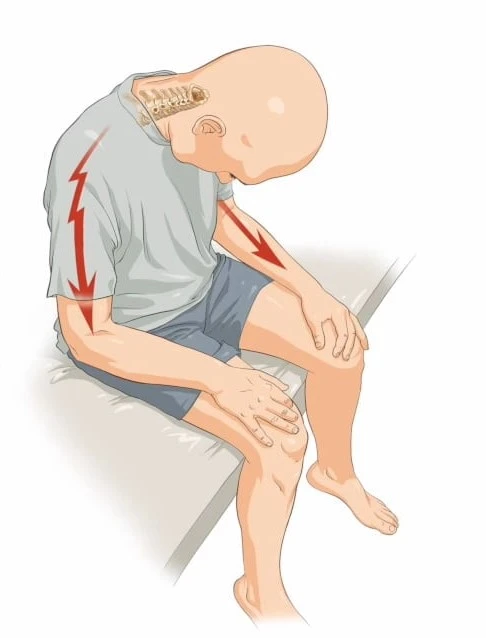
Sensory ataxia:
Neural abnormalities of the spinal cord, visual system, or peripheral nerves may be associated with sensory ataxia. Several nervous system mechanisms facilitate the sense of one’s own body’s position and motion. Problems with walking are typically linked to issues with these nerves.
It’s common to experience difficulty upright with your feet together in order and your eyes closed to indicate sensory ataxia. We call this the Romberg test.
Vestibular ataxia:
The vestibular system is connected to vestibular ataxia. The neural routes that link the inner auditory canal to the cerebellum (brain) are part of the vestibular system, also known as the vestibular nerve system. Hearing, balance, and vertigo issues can result from damage to this region.
Ataxia symptoms can result from damage or degeneration of nerve tissue caused by certain genes.
Other types of ataxia :
Friedreich’s ataxia
Because of an inheritable deficit in the FXN genes, this particular variety of ataxia is either genetic or hereditary. Since it is a degenerative disease, the peripheral nerves, spinal cord, and cerebellum will eventually be destroyed as the illness worsens over time. Among them are:
- Trouble walking
- diminished sensation in the thorax and arms after it started in the lower body
- Poor reflexes
- Tiredness
- Slow or slurred speech
- Loss of vision or hearing
- Chest pain
- Heart palpitations
- Shortness of breath
Limb ataxia
Limb ataxia prevents you from moving your arms in a coordinated manner. This could indicate that you have:
- Having difficulty in writing
- Having trouble in attaching or buttoning garments
- Having difficulty in picking up little items
Ataxia-telangiectasia
Ataxia-telangiectasia features often manifest in childhood and are inherited.
Telangiectasias are small red or pink lines that mimic spider veins, or broken blood vessels, close to the skin’s surface. Additional indicators consist of:
- Trouble walking
- Slow or slurred speech
- Difficulty swallowing
- Slow eye movements
- A weakened immune system
- Increased risk of cancer
Truncal ataxia
Your torso, or trunk, is affected by this kind of ataxia. When you sit, stand, or walk, your trunk may feel unsteady or uneven if you have truncal ataxia.
Gluten ataxia
In response to gluten, the human body may attack your nervous system, resulting in a condition called “gluten ataxia.” It might be connected to coeliac disease, which is brought on by the immune system’s reaction to gluten consumption. Among the symptoms are:
- difficulty moving your limbs or walking
- Inadequate balance or coordination
- Problems with speaking and eye movement
- a tingling sensation in your limbs
Episodic ataxia
When someone has ataxia episodes but either no symptoms or very minor symptoms the rest of the time, their condition is referred to as episodic ataxia.
During an ataxia episode, symptoms could include:
- Lack of balance and coordination
- Trouble with speech
- Muscle spasms
- Involuntary eye movements
- Vertigo (feeling like you’re spinning)
- Migraines
How is the condition identified?
While making a diagnosis, your healthcare provider will first want to go over your medical information. They’ll enquire as to whether hereditary ataxia runs in your family.
Additionally, they may ask you how much alcohol you consume and what substances you use. After that, they will conduct neurological and physical assessments using Trusted Source.
These tests can assist your physician in evaluating items such as:
- coordination
- balance
- movement
- reflexes
- muscle strength
- memory and concentration
- vision
- hearing
Your doctor can also recommend that you undergo more testing or be referred to a neurologist for additional treatment. A healthcare professional or neurological specialist could recommend additional testing like:
Imaging tests: A comprehensive image of your brain can be obtained using an MRI or CT scan. This can assist your physician in identifying any anomalies or tumors.
Blood testing: Blood tests can help determine whether an infection, a vitamin deficit, or hypothyroidism causes your ataxia.
Lumbar puncture: Through a spinal puncture, a small amount of the cerebrospinal fluid (CSF) in the back part of the spine is extracted between the two vertebrae.
What should you expect from your physician?
The physician or medical practitioner will probably ask you about items like:
- What time did your symptoms begin?
- What troubles you initially?
- Do you constantly notice your symptoms, or only sometimes?
- What appears to make your symptoms better?
- What appears to make your problems worse?
- Are there any family members you know who have gone through comparable things?
- Do you take drugs or alcohol?
- Have poisons ever exposed you?
- Have you recently become infected with a virus?
How is ataxia treated?
The most beneficial course of action for treating ataxia will depend on its degree of severity and type. It is occasionally possible to lessen acquired ataxia symptoms by treating its underlying cause, which could be an illness or vitamin deficiency.
There’s no cure for many kinds of ataxia. Nevertheless, several interventions (Trusted Source) might help control or lessen your symptoms and enhance your quality of life.
These include:
- Medications consist of A few medications that could be taken to address the symptoms of ataxia. As an example, consider:
- amitriptyline or gabapentin for nerve pain
- muscle relaxants for cramps or stiffness
- antidepressants for depression
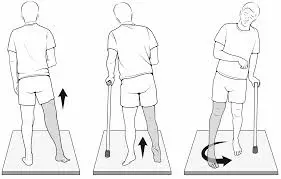
Assistive equipment includes wheelchairs and walkers, which can be used to increase movement. Communication aids can help with speaking.
Physical treatment: Physical therapy is a useful tool for improving balance and movement. It could be beneficial to maintain the flexibility and strength of your muscles.
Speech therapy: In this kind of treatment, a speech therapist will instruct you on ways to improve the clarity of your speech.
Occupational treatment: You can learn some skills from occupational therapy that will make your daily tasks easier.
Ataxia Complications:
The difficulties you encounter will depend on the type of ataxia you have. They could consist of:
- Dizziness
- The rigidity or spasticity (many forms of tense muscles)
- Tremor
- Pain
- Fatigue
- Reduced blood pressure while standing or sitting
- Disruption of the bowel, bladder, or sexual
- A tracheostomy, a treatment that entails making a hole in your neck and inserting a breathing tube, or continuous positive airway pressure devices (CPAP) may be necessary to treat breathing issues brought on by ataxia.
More importantly, ataxia-related falls or bedriddenness might result in pressure sores and injuries.
Ataxia Rehabilitation and Physiotherapy Treatment:
Strengthening the patient’s ability to function through rehabilitation techniques is the physiotherapist’s aim while relating to ataxia resulting from deficiencies in neurological structures that influence the patient’s functions. In situations when this isn’t achievable, the therapist employs compensatory techniques to help the patient function as independently as possible at their current functional level. Enhancing postural responses to external stimuli and gravity shifts, as well as balance, are the main objectives of restorative physical therapy.
Once joint stabilization has taken hold, postural stabilization should be strengthened and expanded.
Functions of the upper extremities developing.
By developing a self-sufficient and functional gait, the patient’s quality of life can be improved by allowing them greater freedom to perform daily duties.
Fundamental training principles:
- Exercises should be done consciously at first for the duration of the training program, and then automatically in subsequent phases.
- Include workouts ranging from simple to sophisticated in the routine.
- The coordinated movement of the distal segments should be considered when the proximal tonus and stabilization are achieved.
- When required, compensatory techniques as well as equipment and supportive aids should be used.
- Sports and a suitable at-home fitness regimen should complement treatment.
Evaluation and measurement:
- To achieve the intended outcome of the physiotherapy and rehabilitation program, it is critical to identify treatment plans appropriate for the patient and his or her needs when treating ataxia.
- This may be performed by employing correct measurement and assessment methodologies, as well as interpreting the data.
- Measurement and evaluation are essential not only for developing a suitable treatment plan but also for monitoring changes in the patient’s condition over time and tracking the therapy’s effectiveness.
- In cases of ataxia, the measuring and assessment standardization issues that are among the most upsetting parts of neurological rehabilitation applications become even more problematic.
- Scales, observational techniques, and computerized systems designed to measure balance are more prevalent in the literature than those designed to measure in-coordination.
- While most balance-related observational methods and scales are simple to use and easily applied in clinical settings, their capacity to produce consistent readings is restricted, and the outcomes can fluctuate based on the observer.
- Despite their great dependability, computerized systems are expensive and need to be used in a laboratory setting. Tools for assessing balance are widely used by physiotherapists.
Techniques for evaluating balance:
- External Perturbation Test – The goal of the push-and-release test for external perturbation is static balancing.
- Pull test (External Perturbation Test) – Objective of static balance under varying sensory circumstances.
- Clinical Sensory Integration Test – The goal of dynamic equilibrium under various sensory situations is examined in the clinical sensory integration test.
- Static and Dynamic Posturography: Static equilibrium is the goal of both static and dynamic posturography.
- Single-Leg Stance Test: achieving static equilibrium is the aim of this assessment.
- Berg Balance Scale: This scale was initially developed to assess the functional equilibrium in both static and dynamic situations.
- Functional dynamic balance and gait – The purpose of the five times sit-to-stand test.
- Four Square Step Test: Dynamic balance goal.
- Variables including step length, step breadth, and gait duration may be useful. In addition, patient-completed self-perception scales like the Dizziness Handicap Inventory, the Activity Specific Balance Confident Scale, and scales for everyday life activities like the FIMTM and Barthel Index can be used to support assessment techniques.
- A few validity and reliability-tested scales have been created to evaluate both extremities ataxia and truncal ataxia jointly.
- Tandem Walking: Dynamic equilibrium is the primary objective of tandem walking.
Ataxia scales:
- Ataxia Functional Composite Scale: Assessing visual acuity, upper extremity ataxia, and gait speed using the Ataxia Functional Composite Scale.
- Computer Graphics Tablet: Assessment of upper extremity ataxia using a computer graphics tablet.
- Short Ataxia Rating Scale: Speech, nystagmus, truncal and extremity ataxia, and gait ataxia are all evaluated using this scale.
- Friedreich’s ataxia impact scale: Speech, upper and lower limb functionality, bodily movement, difficult tasks, loneliness, mood, and self-perceptions are all included in Friedreich’s ataxia impact scale.
Physiotherapy procedures:
The analysis of measurement and assessment data is required before developing a physical therapy plan.
Depending on the kind and features of ataxia, the treatment plan’s contents may change.
For example, stabilization training is more crucial to diminish truncal and extremities ataxia in patients with cerebellar ataxia, even if techniques that increase proprioception and involve visual aids are more widely utilized in patients with sensory ataxia.
To enhance balance and lessen vertigo, the patient with vestibular ataxia should be administered vestibulo-ocular and vestibulo-spinal reflex stimulation.
Sometimes a difficult condition like mixed ataxia may develop that calls for a combination of strategies.
In these situations, the program is mostly determined by the patient’s effort and the physiotherapist’s experience.
The proprioceptive, vestibular, and visual systems, as well as the cerebellum, are closely related, and balance and coordination are the outcome of this relationship, which should be considered while creating the treatment plan.
Proprioceptive exercises, for example, help to increase perception of position and balance. This also holds oppositely. Treatment strategies for extremities ataxia may improve proprioceptive input and foster the development of balance by creating stabilization.
Because proprioception and balance are interdependent, it is therefore impossible to categorize ataxia rehabilitation techniques as solely proprioceptive or balanced procedures.
In simple terms, the following describes how therapeutic applications are classified:
Methods to enhance their proprioception:
- To enhance proprioceptive input, the joint surfaces, muscles, and tendons are manually stimulated. It also seeks to improve body awareness, which should lessen postural instability.
- These include the following: plyometric exercises, balance board-ball and minitrampoline exercises, proprioceptive neuromuscular facilitation (PNF), rhythmic stabilization, slow reversal techniques, resistive exercises, use of Johnstone pressure splints, gait exercises both with and without eyes on various surfaces (hard, soft, incline surfaces).
- These days, vibration is a frequently utilized application.
- Suit therapy is another approach. The outfit includes knee pads, a vest, shorts, and unusual shoes that are secured to the wearer’s body with bungee cords. These bands are made to provide resistance and guarantee that the body is positioned correctly when moving.
- Its primary goals are to improve proprioception (the sense of feeling from joints, fibers, and muscles) and weight-bearing for normalized sensory input about posture and movement.
- The learning material can also incorporate techniques that promote body awareness, such as yoga, body awareness exercises, and the Feldenkrais and Alexandre Techniques.
Exercises to strengthen your balance:

- The proximal muscles should be strengthened initially, followed by trunk stabilization. Mat exercises from the PNF techniques are advised for this aim.
- Following the neuro-developmental sequence, the patient needs to be trained to crawl, get onto the knees, half-knees, and sit position, as well as to establish both static and dynamic stability when in these positions. It additionally serves as important to teach the person being treated how to crawl, get onto the forearms from a lying face down posture, and transition from a backward posture to a bridging position.
- After achieving the ideal posture for the patient with approximations and vocal commands, the patient should be further stabilized by external perturbation (pulling and pushing in different directions).
- To prepare for dynamic stabilization, the patient should then be taught in these positions for functional extension and weight transfer.
- To make the balancing exercises challenging, the patient should then be taught in postures where the center of gravity is shifted or the support surface is narrowed. (For instance, balancing on two or three limbs while crawling, or raising the arms to raise the center of gravity while sitting on the knees).
- After adjusting weight to the front, rear, and sides, narrowing the support surface, and smooth balance in tandem, balancing training on one leg should be performed while standing.
- To gain from the visual input that comes from seeing the patient’s capacity to maintain their postural oscillation in the center of gravity, another alternative is to use the posturography device for balance training.
- For constant equilibrium and stabilization, gait is the most accurate metric. Consequently, the following exercises related to gait training should be included: walking in two narrow lines; tandem gait; backward gait; slowed down gait (soldier’s gait); stopping and turning in reaction to abrupt movements; left and right head rotations, flexions, and extensions.
- Activities in disciplines like yoga and tai chi help people strengthen their balance.
Vestibular exercises:

- Repetitive head movements and the Cawthorne and Cooksey exercises are very important since dizziness often coexists with balance impairment in vestibular disorders.
- A vestibular training program consists of a sequence of repeated, increasingly difficult head, body, and eye movements designed to help with sensory substitution and encourage movement. Physical and occupational therapists use many of the exercises in this program today.
How to treat ataxia of the extremities:
- Fixation is achieved by creating a balance between the eccentric and concentric contractions during multi-joint motions of the lower extremities, and the upper extremities specifically, using exercises intended for the treatment of extremity ataxia.
- It is crucial to establish calm, controlled, reciprocal multi-joint movement as well as stabilization when performing these exercises. For this reason, Frenkel device his coordination exercises. PNF-like actively repeated contractions can be used alone or in conjunction with Frenkel’s coordination exercises.
- When ataxia of the extremities is more severe, these two types of exercise might not be sufficient, even though they are helpful for people with milder symptoms.
Utilizing assistive technology:
- The use of supportive equipment helps the patient to perform more comfortably within his current functional level when restorative physical treatment approaches are insufficient. It may be better to utilize weighted walkers and suspend weights from the extremities in cases of severe ataxia.
Sports:
- This kind of patient is suitable for swimming, darts, billiards, horseback riding, and golf.
Therapy:
- Ataxia patients frequently experience frustration and depression; this is typically the result of adjusting to symptoms that impair their physical coordination and movement.
Nutrition and supplements:
- Due to extremely low vitamin E levels, some ataxia patients need to follow a particular diet in addition to taking supplements. A diet without gluten might be good for them since several ataxia patients may also have gluten sensitivity.
Medication:
- Gamma-globulin injections are recommended for certain ataxia telangiectasia patients to strengthen their immune systems. Medication is also available for involuntary eye movements and spasms of the muscles.
Can I use natural therapies or treat ataxia on my own?
What triggered your ataxia may determine whether or not home treatments are helpful. Taking vitamin E supplements could be beneficial, especially if there is a vitamin shortage at the root of the issue.
Avoiding triggers like stress or alcohol might also be helpful in some situations. Nevertheless, a lot of the causes call for medical attention.
What is the prevention of ataxia?
Ataxia can have some avoidable causes. You cannot, however, prevent or avoid many of the reasons since they occur unpredictably. Moreover, it’s not always possible to reduce the chance of having this symptom.
Generally speaking, though not constantly, certain variables can be avoided:
drunkenness caused by alcohol. If you consume alcohol in moderation or not at all, you can prevent ataxia from this. Ataxia is significantly more difficult for certain people to avoid when they drink because they may also have medical issues like alcohol intolerance that make it much easier to get drunk.
Traumatic brain injury and concussions. You can lower your chance of acquiring ataxia from brain injuries by using safety gear and helmets.
Drugs (both for recreational use and prescribed, particularly drugs for seizures and depressive disorders). You should not discontinue using a prescription medicine if you have ataxia without first consulting your doctor. It’s safer to talk to your doctor about stopping your medicine suddenly to prevent any possible harmful side effects.
exhaustion and tension. Getting enough sleep is a key method to prevent ataxia brought on by fatigue. Stress management is also crucial.
breathing in the fumes from substances that have been inhaled, including gasoline, glue, spray paint, and toluene. One of the numerous issues that might arise from puffing is ataxia.
Reaching and maintaining a healthy weight. Your weight and physical health are related to numerous disorders that impact the blood flow to your brain, particularly stroke. Taking good care of your physical health might occasionally stop or at least postpone the onset of disorders that may lead to these issues.
toxic exposure to metals, chemicals, or other materials (such as lead, mercury, etc.). Toxic substances should be avoided as one method of preventing ataxia. When working around potentially dangerous substances, you must wear safety gear and follow all safety protocols.
Nutritional issues and vitamin deficits (e.g., low B12 levels). The dietary deficiencies that lead to ataxia can be avoided by eating a balanced diet.
When to consult a physician:
You must consult a physician if you have ataxia symptoms for which there is no recognized reason. They can assist in making a diagnosis and start any necessary follow-up care.
It’s critical to be aware of symptoms like issues with:
- balance or coordination
- strolling, conversing, or swallowing
- Abrupt alterations in these abilities may signify a medical crisis, like a stroke. Get in touch with your local emergency services straight once if you think someone is experiencing a stroke or any other medical emergency.
Conclusions
There are numerous varieties of ataxia. While each has its unique origins and symptoms, they are all characterized by difficulties with balance and coordination. It is important to consult your physician if you experience ataxia symptoms since they may indicate a more serious issue.
FAQs
Is ataxia ever addressed?
While there are medicinal treatments for ataxia, many underlying causes cannot be resolved and need further research.
Is ataxia a harmful condition?
Oftentimes, ataxia can be a hazardous condition, depending on the cause. For example, many people with Friedreich ataxia are wheelchair-bound by the age of 45. Dependable source Heart problems account for the majority of deaths, which occur at an average age of 36.5 years.
Is ataxia a kind of dementia?
There may be dementia symptoms in some spinocerebellar ataxia instances.
What is ataxia’s primary cause?
Atherosclerosis typically arises from damage to the cerebellum or its neural pathways. The cerebellum governs the coordination of muscles. Ataxia can be brought on by a variety of illnesses, such as alcohol abuse, degenerative diseases, multiple sclerosis, stroke, tumors, and hereditary disorders.
How long does ataxia last?
Temporary ataxia may occur after drinking alcohol, using drugs, or taking prescription medications. Alternatively, it may result from a stroke or other long-term (permanent) brain or nerve injury. Furthermore, it may worsen (advance) due to a degenerative illness. The reason will determine your prognosis.
Which vitamin can help with ataxia?
Vitamin E supplements should be administered to patients whose ataxia is caused by a vitamin E deficit.
References
- Professional, C. C. M. (n.d.-a). Ataxia. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/17748-ataxia
- Seladi-Schulman, J. (2023, December 19). Everything to Know About Ataxia. Healthline. https://www.healthline.com/health/ataxia#bottom-line
- Burtka, A. T. (2024, April 18). Ataxia: Causes, Symptoms, and Treatment. WebMD. https://www.webmd.com/brain/ataxia-types-brain-and-nervous-system
- Ataxia – Diagnosis and treatment – Mayo Clinic. (2024, January 30). https://www.mayoclinic.org/diseases-conditions/ataxia/diagnosis-treatment/drc-20355655
- Ataxia – UF Health. (n.d.). https://ufhealth.org/conditions-and-treatments/ataxiacopy
- Ataxia – Neurological condition. (n.d.). https://www.brainresearchuk.org.uk/neurological-conditions/ataxia
- Ataxia Types. (2023, June 10). News-Medical. https://www.news-medical.net/health/Ataxia-Types.aspx



5 Comments