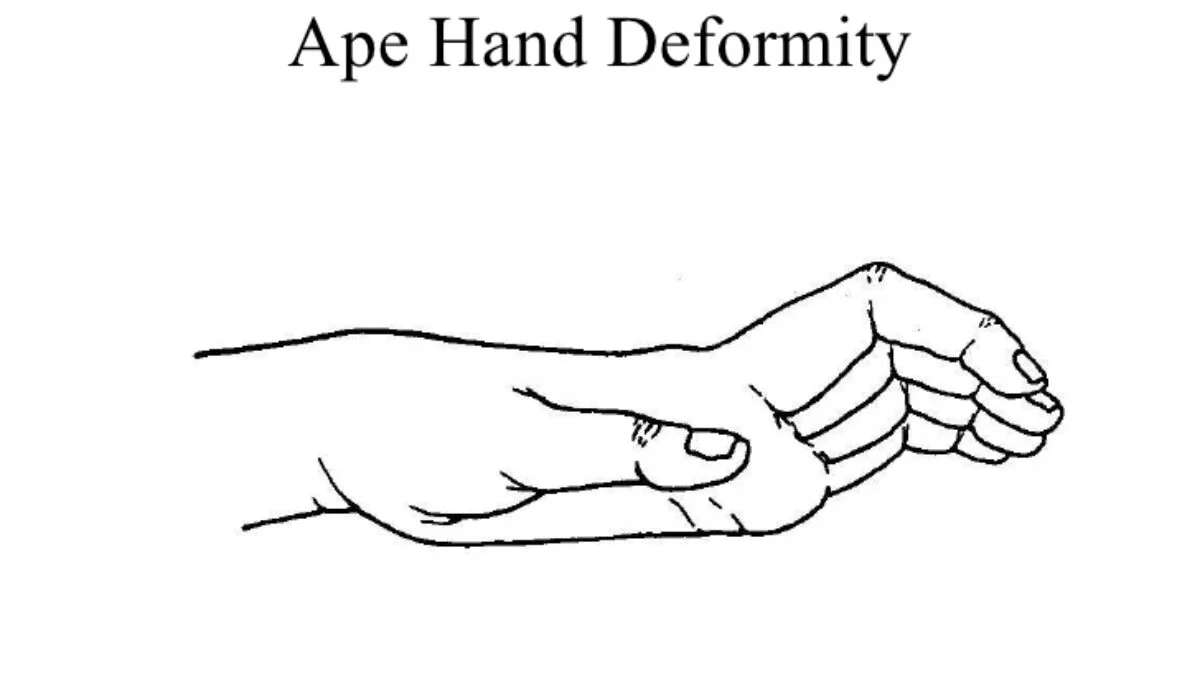
Ape Hand Deformity
What is an Ape hand deformity?
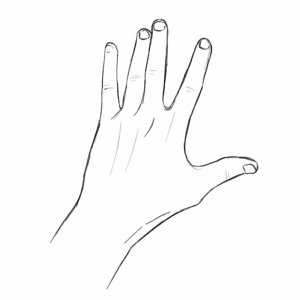
Ape Hand Deformity is a particular condition characterized by the inability to move the thumb away from the rest of the hand, resulting in a hand posture where the thumb is aligned with the other fingers. This deformity primarily arises from damage to the median nerve, which impairs the muscles responsible for thumb opposition and abduction.
The ape hand is a physical defect in humans where the thumb has little to no abduction and opposition because the hand is unable to oppose or abduct the thumb. The ability to shift the perpendicular (90°) off the palm’s plane is known as abduction of the thumb.
The first metacarpal’s opposition is its capacity to swing along the palmar surface of the hand and make contact with the tip of the little finger and the thumb. There may also be restricted flexion and extension of the thumb.
The name “ape hand” is deceptive because, although primates have opposed thumb movement, people incorrectly think that the hand has an ape-like appearance due to functional movement constraints.
Loss of opponens pollicis muscle function and damage to the distal median nerve, commonly referred to as a Median Claw lesion, are the causes of the Ape Hand deformity. It may happen if the median nerve is injured at the wrist or elbow.
Why is it called ape hand?
The hand muscles start to atrophy when the thumb can no longer pinch against a finger (pincer grip).
The hand exhibits what some people believe to be an ape-like look due to the inability to resist the thumb.
Since apes have opposable thumbs, the term “ape hand” contains several paradoxes.
Mechanism of Injury / Pathological Process
The mechanism of injury is a profound injury to the wrist, forearm, and arm that damages the median nerve, impairing the opponens policies and thenar muscles.
Anatomy of Median Nerve:
Starting from the spinal cord, the median nerve is one of the brachial plexus’s branches. The spinal cord’s C6, C7, C8, T1, and occasionally C5 nerve roots are the nerve roots. The medial and lateral cords of the brachial plexus branch into the axilla, where the axillary arteries unite to produce the nerve anterior to the artery on each side.
The median nerve goes from the axilla and enters the cubital fossa in the arm, where it is connected to the brachial artery. The nerve travels between the two heads of the pronator teres muscle and enters the cubital fossa, which is medial to the brachialis tendon. Between the flexor digitorum profundus and flexor digitorum superficialis muscles in the forearm, the nerve continues to run.
Just above the wrist, the median nerve is situated between the flexor digitorum superficialis and flexor carpi ulnaris muscles. The nerve that supplies the skin of the central part of the palm originates in the wrist area and gives rise to the palmar cutaneous branch. Located anterior and lateral to the tendon of the flexor digitorum superficialis muscle in the carpal tunnel, the nerve continues into the hand through the tunnel.
The nerve splits into palmar digital branches and a muscle branch in the hand. The palmar digital branch provides feeling to the lateral 3 ½ digits and the lateral two lumbricals, whereas the muscular branch provides feeling to the thenar eminence muscles.
The following four thenar muscles:
- Abductor pollicis muscle
- Adductor pollicis muscle
- Opponens pollicis muscle
- Flexor pollicis brevis muscle
Branches of the Median Nerve:
The whole upper limb is home to several branches of the median nerve.
A forearm produces two branches.
- Muscular branches
- Anterior interosseus nerve
Three branches are given on the hand.
- Cutenues branch
- Palmar digitorum nerve
- Recurrent branch
Median nerve injury:
There are two basic categories of median nerve injury: high and low. The location of a low median nerve damage is under the elbow, while a high median nerve injury is above the elbow.
This deformity happens if the median nerve is injured at the wrist for any cause, or if the nerve is squeezed there and impacts the thenar muscles.
Symptoms of Ape Hand Deformity
- This condition is a component of median nerve palsy and usually indicates difficulties with thumb movement in various planes.
- The thumb’s range of motion is either very restricted or absent.
- pain in the lateral side of the palm or wrist.
- The thumb is weak.
- might decrease the thumb’s sensation.
- unable to move the thumb on the interior of the palm (limited opposition movement).
- Thumb irritation might occur sometimes.
- the withering of the thenar muscles.
What are the causes of Ape Hand Deformity?
The ape hand is often caused by median nerve palsy, which is frequently caused by a severe lesion to the forearm or wrist. such that the thenar muscles’ ability to operate is compromised. According to a 2018 study, the most prevalent type of peripheral nerve neuropathy is called median nerve mononeuropathy.
Via the carpal tunnel, the median nerve enters the hand after passing through the forearm and down the arm. The little finger is unaffected by the median nerve, which supplies motor and sensory function to the wrist, hand, thumb, index finger, middle finger, and part of the ring finger. It does not supply motor function to the forearm.
One of the most prevalent deformities in simian apes is the thenar muscles. Pinch clutching is made possible by the thenar muscles.
A condition similar to the ape hand:
An ape hand malformation is linked to a wide range of hand conditions:
Compression of the median nerve, which runs through the carpal tunnel and into the wrist, causes carpal tunnel syndrome.
In the thumb, index finger, middle finger, and part of the ring finger, CTS symptoms include pain, tingling, or numbness. Forearm pain is a common symptom.
- De Quervain’s tendinosis:
De Quervain’s tenosynovitis, another name for Quervain’s tendinosis, is an inflammation of the thumb tendons. It is caused by thumb damage, thumb-grabbing repetitive motion, and inflammatory diseases such as rheumatoid arthritis. The base of the thumb is painful and sensitive as a result of this position.
Women are eight to ten times more likely than males to be impacted by this illness, according to the survey.
- Trigger finger:
A finger or thumb that becomes caught in a bent posture is called a trigger finger or trigger thumb, sometimes referred to as stenosing tenosynovitis.
The base of the thumb or finger will hurt if you have a trigger finger. Any movement of the thumb or finger causes the sufferer to experience a popping or cracking sound. There is a certain amount of stiffness that goes away when the thumb and fingers are utilized or moved in any way. It may be more severe in the morning.
- Pronator Syndrome:
When the pronator muscle in the forearm compresses the median nerve, pronator syndrome results.
The patient reports having limited forearm mobility and a lack of feeling over the thenar eminence muscle.
Differential Diagnosis
- Carpal tunnel syndrome.
- De Quervain’s tendinosis.
- Trigger finger.
Diagnosis
Clinical Presentation:
The condition is a component of median nerve palsy and is characterized by thumb movement affection in many planes. Usually, the opponent’s mobility is restricted such that the individual is unable to contact the tips of all fingers with their thumb.
Physical examination:
To verify the “bottle sign,” see if there is a space between the skin of the hand and the item when someone grasps a lengthy object, such as a bottle. This symptom indicates a thenar muscle weakness caused by a damaged median nerve.
Another was when the patient was asked to test whether or not they could touch the tips of each finger with their thumb. This is an indication that the patient is unable to accomplish that and their thumb is in the ape posture.
- Nerve Conduction Velocity, or NCV: Affected median nerves have some degree of electrical conductivity impairment.
- EMG Test: This test can detect any abnormality affecting the muscles that get supply from the median nerve. This will aid in the search for additional reasons, such as polyneuropathy.
Treatment of Ape Hand Deformity:
The primary factor influencing treatment is the cause of the median nerve damage. One treatment option for carpal tunnel syndrome is splints.
Medical Treatment:
- Anti-inflammatory medications to treat pain.
- The purpose of manual therapy techniques is to promote thumb movement.
- Avoiding the action that causes your thumb to hurt or get stressed.
- Use heat therapy or ice massage.
- It is recommended to use dynamic splints to facilitate thumb mobility.
Surgical Treatment:
Depending on the degree of the deformity, surgery may be required. The hand’s damaged portion functions better after surgery.
Surgical care might include:
- Decompression of the nerves
- nerve repair
- transplant of nerves
Surgery including tendon transfer is advised if nerve repair is not completed. To restore a function lost as a result of nerve damage, tendon transfers use additional tendons from other parts of the hand or forearm.
Physical Therapy Treatment in Ape Hand Deformity:
The objective of physical therapy care is:
- regain the strength of your muscles.
- Improve the functionality of your muscles.
- Increase the impacted area’s sensitivity.
- Reduce the pain.
- It aids in the restoration of muscular strength while braces and splints (C-splints) aid in the healing process.
Passive movement Exercise:
- Since the patient is unable to do the entire movement correctly, the therapist passively performs the entire thumb movement. For example, thumb flexion, thumb extension, thumb abduction, and thumb adduction movements.
Active movement Exercise:
- The patient was instructed by the doctor to actively move their thumb.
- The patient flexes their thumb in the direction of their palm.
- The patient extends their thumb, moving it away from their palm.
- Thumb abduction: the patient moves their thumb away from their palm’s lateral line.
- Thumb adduction: The patient moves their thumb in close proximity to the palm’s lateral line.
- Thumb Opposition Movement: The patient performs an opposition movement in which the thumb sequentially touches each fingertip.
Finger Stretch
- Stretch your hands with this exercise to help relieve pain and improve hand range of motion.
- Place the hand on a tabletop or other level surface, palm down.
- Without straining the joints, slowly extend your fingers so they are as flat on the surface as possible.
- Release after thirty to fifty seconds of holding.
- Repeat with each hand for a minimum of four more times.
Strengthening Exercise:
- Before the therapist moves on to the strengthening exercise, the patient performs the movement actively.
- This workout uses a little flexible belt, rubber, or finger spring. The finger spring is used by the patient to perform the thumb opposition action. The thumb and finger grasp the spring, which is subsequently squeezed by each finger.
- To strengthen the muscles, the patient exercises their thumb by wearing rubber on their finger and thumb.
Grip Strengthener
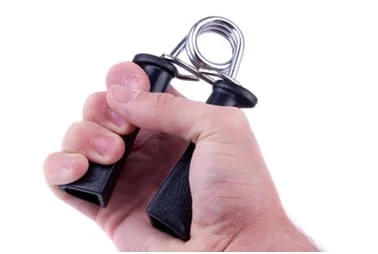
- Certain tasks, such as keeping objects in place without dropping them and turning knobs on doors, can be made simpler with this practice.
- Squeeze as hard as you can on a soft ball that is in your hand.
- After a brief period of holding, release.
- Repeat five to ten times with both hands.
- Two or three times a week, perform this exercise; however, allow the hand to rest for 48 hours in between.
- If you have any injury to your thumb joint, avoid doing this exercise.
Pinch Strengthener
- The thumb and finger muscles are strengthened by this motion.
- It can make tasks like using the gas pump, opening food packages, and turning keys easier for the individual.
- Place a soft foam ball or putty between the thumb and the tips of your fingers. For 20 to 40 seconds, hold.
- Repeat with both hands ten to fifteen more times.
- Do this exercise two or three times a week, allowing your hands to rest for 48 hours in between.
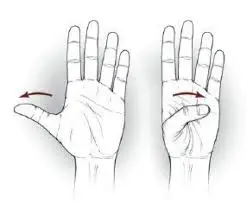
Thumb Extension
- Developing stronger thumb muscles will make it easier for you to pick up and move heavy objects, such as bottles and cans.
- Lay the hand down flat on a surface. Encircle the hand at the base of the finger joints with a rubber band.
- As far as possible, slide the thumb gently away from the fingers.
- Release after 20 to 40 seconds of holding.
- Ten to fifteen repetitions for each hand.
- You may perform this exercise two or three times each week, but give your hands a 48-hour break in between sets.
Thumb Flexion
- The thumbs’ range of motion is aided by this action.
- First, extend your hand in front of you, palm up.
- The thumb should be extended as far away from other digits as feasible.
- Next, bend the thumb such that it contacts the tiny finger’s base by bending it across the palm.
- For 20 to 40 seconds, hold.
- Make sure you repeat each thumb at least four times.
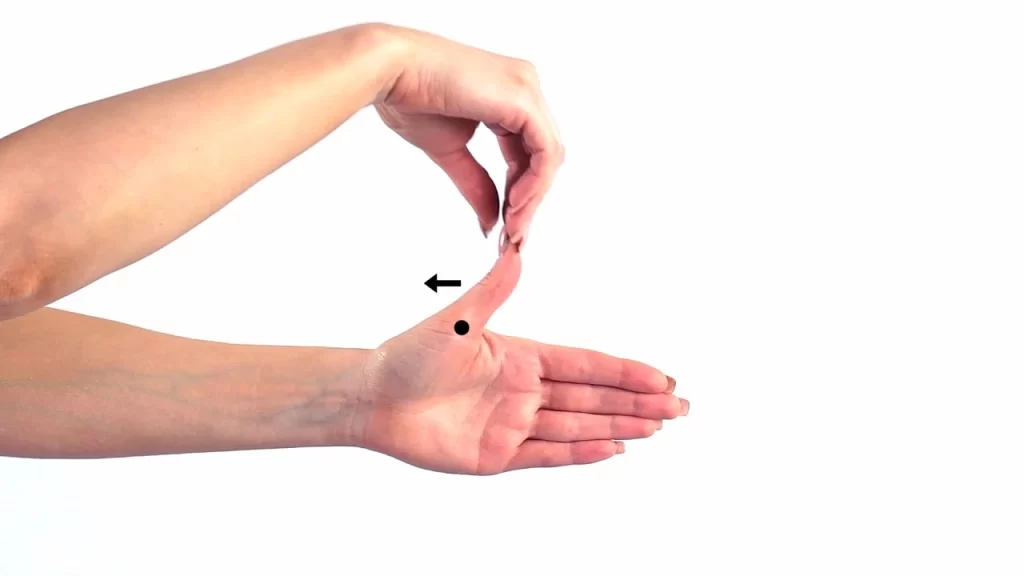
Thumb Touch

- This exercise helps the thumbs have more range of motion, which is beneficial for tasks like picking up the toothbrush, fork, spoon, and writing pens.
- Straighten your wrist as you hold out your hand in front of you.
- Form an “O” with the thumb and each of the four fingertips by slowly touching them one at a time.
- For thirty to forty seconds, hold each stretch.
- Continue doing it on each hand for a minimum of four to five times.
Thumb Stretches
- For the thumb joints, try these two stretches:
- Hold out your hand, palm facing you.
- Bend the thumb tip slightly in the direction of the index finger’s base.
- For 20 to 30 seconds, hold. Let go and do it four or five more times.
- Hold out your hand, palm facing you.
- Using only the lower thumb joint, slowly extend the thumb across the palm.
- For 20 to 40 seconds, hold.
- Let go and repeat four more times.
Play With Clay
- A better technique to increase finger range of motion and strengthen hands simultaneously is to play with clay or putty.
- It won’t even feel like physical activity.
- Simply compress the clay into a ball, roll it into long “snakes” using your hands, or crimp the spikes on a dinosaur with your fingertips, following the children’s example.
Hot and Cold therapy:
It aids in sensory improvement and the reduction of pain and inflammation.
Electrical modality:
In order to excite the muscles of the opponent, therapists first apply Ig current to the thenar muscles. then go progressively to the SF current, which aids in muscular strengthening.
Prognosis of the Ape Hand Deformity:
Usually, the prognosis is favorable and early. Conservative therapy aids in the early relief of symptoms; however, this relies on the extent of the nerve injury, the patient’s age, and their knowledge of it. In two to six weeks, the illness starts to get better. The entire recovery period following surgery ranges from four months to two and a half years.
For those who have Ape Hand abnormalities, the prognosis is dependent on a number of factors, such as the degree of nerve damage, the effectiveness of therapy, and the patient’s commitment to preventive measures.
Many people might see an improvement in their quality of life and hand function with an early diagnosis and suitable therapy. Severe or untreated instances, however, may result in functional restrictions and long-term impairment. While creating a treatment plan and providing continuing care, healthcare professionals should take the patient’s unique requirements and circumstances into account.
Preventive Measures
Although certain hand malformations cannot be prevented, taking preventative steps might lessen the likelihood of acquiring ape hand. Ergonomics and lifestyle adjustments are critical in jobs or pursuits involving repeated hand motions or extended pressure on the median or ulnar nerves.
These might include practicing good hand and wrist placement during activities, taking frequent pauses, and utilizing ergonomic tools and equipment. Additionally, nerve compression and associated hand abnormalities can be avoided by maintaining general wrist and hand health with stretches, and exercises, and avoiding undue force or strain.
Complications
The extensor hood mechanism’s changed balance after intrinsic tendon transfers presents additional problems in comparison to adductor surgery.
The transfer may not be suitable if the chosen muscle lacks sufficient strength or excursion. When transferring onto the lateral bands of the extensor covering, an additional extension issue occurs.
Although a strengthening program to increase muscle mass can treat insufficient tendon transfers, they often require surgical correction.
The transfer may also be inappropriate if the chosen muscle is very strong or if its excursion is too short.
If the transfer is stitched too tightly into the lateral band, the finger may develop a swan-neck deformity.
Treatment using a passive range of motion can be utilized to treat tendon transfers that are either too strong or too tight to allow for flexibility.
Conclusion
Although the effects of Ape Hand abnormalities on hand function may be comparable, there are notable differences in their underlying causes, clinical presentations, and therapeutic modalities. Healthcare providers may give patients with hand abnormalities the best care possible and improve their results by knowing the unique features of each disease and tailoring therapeutic approaches accordingly.
For those with Ape Hand abnormalities, early diagnosis, appropriate care, and preventative actions are essential to reducing disability and optimizing hand function.
FAQs
What other name is there for the ape hand deformity?
The thumb is described as an “ape-like hand” because it is usually rotated and adducted. The paralysis of the flexor digitorum superficialis causes injury to the median nerve in the mid-forearm, resulting in the deformity known as the “pointing finger.”
Which nerve in the ape hand is injured?
Overview. The disorder known as ape hand deformity causes the thumb to become permanently twisted and adducted, impairing its ability to move opposably. Damage to the distal median nerve, which supplies the thumb’s controlling muscles, is the reason for this deformity.
What differentiates ape hands from human hands?
A small thumb combined with long, curled fingers characterizes the normal monkey hand (Midlo, 1934). The human hand, on the other hand, consists of fingers that have gotten shorter and straighter together with a thumb that is considerably bigger, stronger, more flexible, and completely opposable.
What is a median nerve palsy deformity?
It is referred to as “ape-hand deformity”. lack of sensation in the radial portion of the ring fingers, long fingers, thumbs, and index fingers. Median nerve damage may make ordinary tasks like writing, turning doorknobs, brushing teeth, tying shoes, and making phone calls difficult.
Which muscles are used in the hand of an ape?
Damage to the recurrent motor branch of the median nerve results in ape hand deformities. The opponens pollicis muscle, one of the thenar eminence’s muscles, becomes denervated and dysfunctional as a result. Opposition to using the thumb is impossible for those who have this condition.
What differentiates the claw hand from the ape hand?
The term “ape-like hand” refers to the thumb’s predominant rotation and adduction, whereas “claw hand” describes a condition in which the fingers are bent or curled. This may make it difficult for you to pick up or hold items in your hands. One hand, both hands, or all fingers on one hand may be affected.
In what kind of nerve damage might an ape-like hand result?
Mostly rotated and adducted, the thumb is referred to be an “ape-like hand.” Damage to the median nerve in the mid-forearm results in paralysis of the flexor digitorum superficialis, which causes ape-like hand deformities.
Why does ape hand occur?
Damage to the distal median nerve, commonly known as a Median Claw lesion and the subsequent loss of opponens pollicis muscle function result in the Ape Hand Deformity. There are apes who lack opposable thumbs, which is why the term “ape hand deformity” is misleading.
What is the duration required for the regrowth of an atrophied muscle?
The degree of atrophy that happened and the preexisting physical state will determine how long it takes. Physical therapy must be completed for a minimum of two weeks before you start to see any changes in your muscles. Physical treatment may be necessary for several months in order to fully regain muscle growth and strength.
Which muscles may atrophipate following nerve injury to result in the malformation of the ape hand?
The distal median nerve damage, also known as a Median Claw lesion, and the subsequent disposition of the opponens pollicis muscle function are the causes of the Ape Hand Deformity.
What’s the name for ape hands?
All (except humans) have prehensile feet, and all have prehensile hands, albeit to varying degrees.
A monkey hand is what?
The inability to abduct the thumb—that is, to have the thumb orientated perpendicular to the palmar surface of the hand—distinguishes the ape hand deformity in humans.
References
- Maurya, J. (2023, March 8). Ape Hand Deformity: Cause, Symptoms, Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/ape-hand-deformity/
- Parmar, D. (2024, April 21). Ape Hand Vs Claw Hand: Understanding the Differences. Physical Therapy Treatment and Exercise. https://physical-therapy.us/ape-hand-vs-claw-hand/
- Thakkar, D. (2023, December 13). Ape Hand Deformity – Cause, Symptoms, Treatment, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/ape-hand-deformity/






One Comment