Anterior Interosseous Nerve
Introduction
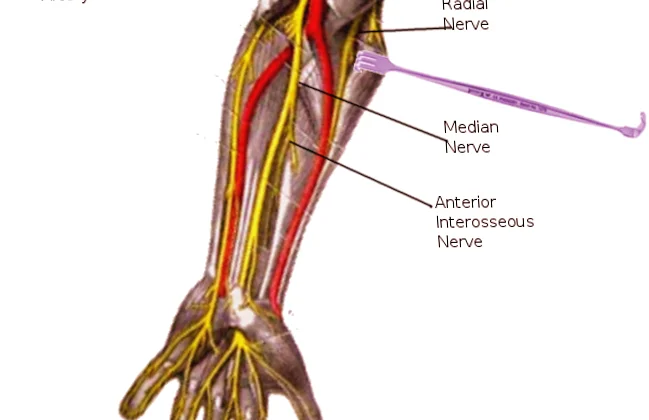
The Anterior Interosseous Nerve (AIN) is a branch of the median nerve that arises in the forearm. It supplies the flexor pollicis longus (FPL), the lateral half of the flexor digitorum profundus (FDP) (to the index and middle fingers), and the pronator quadratus (PQ). It is purely a motor nerve, with no sensory function.
The nerve passes between the flexor pollicis longus and flexor digitorum profundus muscles as it descends the proximal forearm. It goes beside the anterior interosseous artery.
The nerve runs alongside the pronator quadratus muscle in the distal forearm before branching off into tiny terminal branches at the wrist joint.
The anterior interosseous nerve’s primary job is to supply the forearm muscles, which include the
- Flexor pollicis longus muscle
- The flexor digitorum profundus muscle’s lateral aspect
- Pronator quadratus muscle
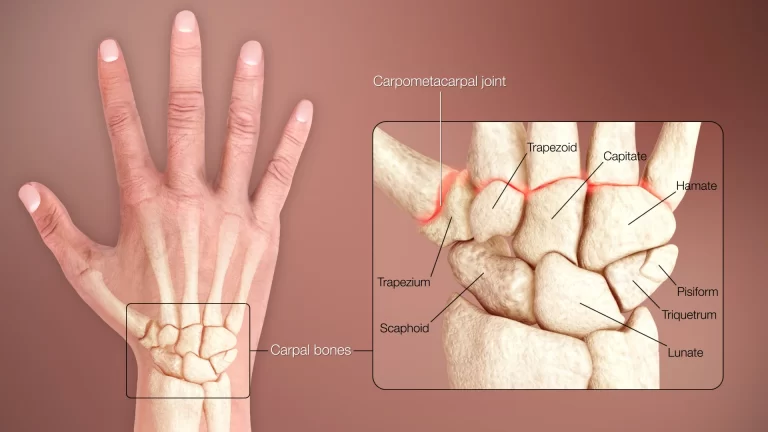
In addition, it supplies innervation for the distal radioulnar, radiocarpal, and certain intercarpal joints.
Structure
Originating from the median nerve in the proximal forearm, roughly 5-8 cm distal to the lateral epicondyle of the humerus, the anterior interosseous nerve is made up of the C5-T1 spinal nerve roots. According to a 2018 cadaver study (n=50), the anterior interosseous nerve branched from the median nerve anywhere from 1.5 to 7.5 cm (mean = 5.2 cm) distal to the intercondylar line.
Function
Sensory Functions
The distal radioulnar, radiocarpal, and intercarpal joints are where the anterior interosseous nerve ends in articular branches that aid with feeling.
Motor Functions
The deep compartment of the anterior forearm receives motor innervation from the anterior interosseous nerve:
- Flexor pollicis longus
- The lateral portion of the flexor digitorum, or the index and middle fingers
- Pronator quadratus
Branches
The deep muscles in the anterior compartment of the forearm are motor innervated by the anterior interosseous nerve, and these muscles include:
- Flexor pollicis longus
- Only the lateral portion of the flexor digitorum profundus is supplied by the ulnar nerve; the medial side is
- Pronator quadratus
The anterior interosseous nerve’s terminal branch passes through the pronator quadratus’ posterior side, where it also supplies sensory branches to the wrist’s carpal bones.
Course
In the proximal forearm, between the pronator and teres heads, the anterior interosseous nerve emerges from the median nerve.
Between the flexor digitorum profundus and the flexor pollicis longus, it descends the forearm. The anterior interosseous artery is present along with it.
The anterior interosseous nerve ends as little sensory branches at the wrist level after traveling deep to the pronator quadratus.
Clinical Importance
Lesions to the anterior interosseous nerve are considered uncommon because of their deep placement in the forearm; yet, under some situations, the overlaying tissues may induce compression.
The following structures have the potential to compress the anterior interosseous nerve:
- Struthers ligament
- Bicipital aponeurosis
- The pronator teres muscles’ fibrous arch, which lies between the superficial and deep heads
- Fibrous arch where the flexor digitorum muscle origin
- Anamalous muscles. i.e., Gantzer muscle
The brachialis fascia and the origin of the deep head of the pronator teres muscle are the most often compressed structural sites. However, it is thought that “fibrous bands from the superficial head of the pronator teres, bands from the superficial arcade, the nerve running deep to both heads of the pronator, and compression by a double lacteous fibrous” are less common causes of compression.
The following are other reasons for compression:
- Trauma, such as proximal third forearm fractures and supracondylar humeral fractures
- vascular illness. For example, vascular hypertrophy and thrombosis
- Cysts
- Abscesses
- Hemostases
- Cancers
- Iatrogenic. For example, medication injections in the forearm, fracture reduction
Anterior Interosseous Nerve Compressive Syndrome
The flexor digitorum profundus of the index finger, the flexor pollicis longus, and the pronator quadratus are paralyzed by this uncommon upper extremity compressive neuropathy. Hyperextension of the thumb results in hyperextension of the interphalangeal joint and flexion of the metacarpophalangeal joint, which is defined by the “inability to flex the distal interphalangeal joints of the thumb and index finger, causing an inability to make a pulp pinch, resulting in a distal interphalangeal joint and flexion of the proximal interphalangeal joint. the contact area of the thumb pulp with the indicator much more proximal than normal”.
To test the pronator quadratus muscle, ask the patient to oppose forearm pronation while keeping the elbow completely extended. This will lessen the activity of the pronator teres muscle.
In cases of anterior interosseous nerve compressive syndrome, a sensory examination of the hand and forearm will reveal nothing unusual.
Paresis or paralysis of the index finger’s flexor pollicis longus or flexor digitorum profundus is known as incomplete anterior interosseous nerve syndrome, and it impairs the thumb or index finger’s distal phalanx’s ability to flex. The flexor tendon-related differential diagnoses of incomplete anterior interosseous nerve syndrome include stenotic tenosynovitis, adherence or adhesion, and rupture.
For the spontaneous etiology of anterior interosseous nerve syndrome, electrodiagnostic investigations are essential. Since the anterior interosseous nerve lacks sensory innervation, sensory nerve conduction testing of the median nerve should be normal.
The pronator quadratus, the radial part of the flexor digitorum profundus, and the flexor pollicus longus will all exhibit findings from electromyography. These will assist in distinguishing between compressive neuropathy and neurologic amyotrophy. In assessing these patients, magnetic resonance imaging is also helpful.
Surgical Importance
Following several months of unsuccessful nonoperative methods, surgical therapy includes investigation, neurolysis, and decompression.
The idea of surgical intervention is usually explored after at least three months of unsuccessful conservative therapy, and it is usually only provided in select situations until a definite reason can be found.
To determine the precise areas of compression during median nerve surgical decompression, careful dissection is required. It is essential for locating and releasing fibrous bands or compressing edges.
FAQs
What are anterior interosseous nerve damage symptoms?
An isolated palsy of the flexor pollicus longus, the pronator quadratus muscles of the forearm, and the index and long fingers of the flexor digitorum profundus is known as anterior interosseus syndrome. It usually presents as forearm discomfort with weakness in the pincer action of the thumb and index fingers.
What is the special test for the anterior interosseous nerve?
Another sensitive test is the Pinch Test: a patient with the anterior interosseous syndrome will also not be able to pinch a sheet of paper between the thumb and index finger, instead of clamping the sheet between the extended thumb and index fingers, akin to a tong rather than a clamp.
What fracture is an anterior interosseous nerve injury?
According to several studies, nerve-related problems occur in between 6.6 and 31% of pediatric supracondylar elbow fractures. Anterior interosseous nerve (AIN) palsy accounts for one-third of these and is often characterized by a lack of active thumb and index flexion.
What is anterior nerve pain in the forearm?
Inflammation or compression of the arm’s anterior interosseous nerve can result in Forearm Nerve Compression Syndrome, a rare and excruciating nerve entrapment syndrome. An enlarged biceps tendon bursa, trauma, fractures, and a shift in the pronator teres muscle’s position can all contribute to it.
What distinguishes anterior interosseous nerve syndrome from pronator syndrome?
The symptoms of PS include minor motor findings, median nerve paresthesias, and nonspecific volar forearm discomfort. The flexor pollicis longus, the flexor digitorum profundus of the index and middle fingers, and the pronator quadratus are among the muscles innervated by that nerve that might have pure motor palsy or AIN syndrome.
References
- Anterior interosseous nerve. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/anterior-interosseous-nerve
- TeachMeAnatomy. (2024b, April 21). Anterior interosseous nerve – course – Motor functions – TeachMeAnatomy. https://teachmeanatomy.info/encyclopaedia/a/anterior-interosseous-nerve/
- Anterior interosseous nerve. (2023, August 4). StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK525956/