Anterior Cruciate Ligament
Introduction
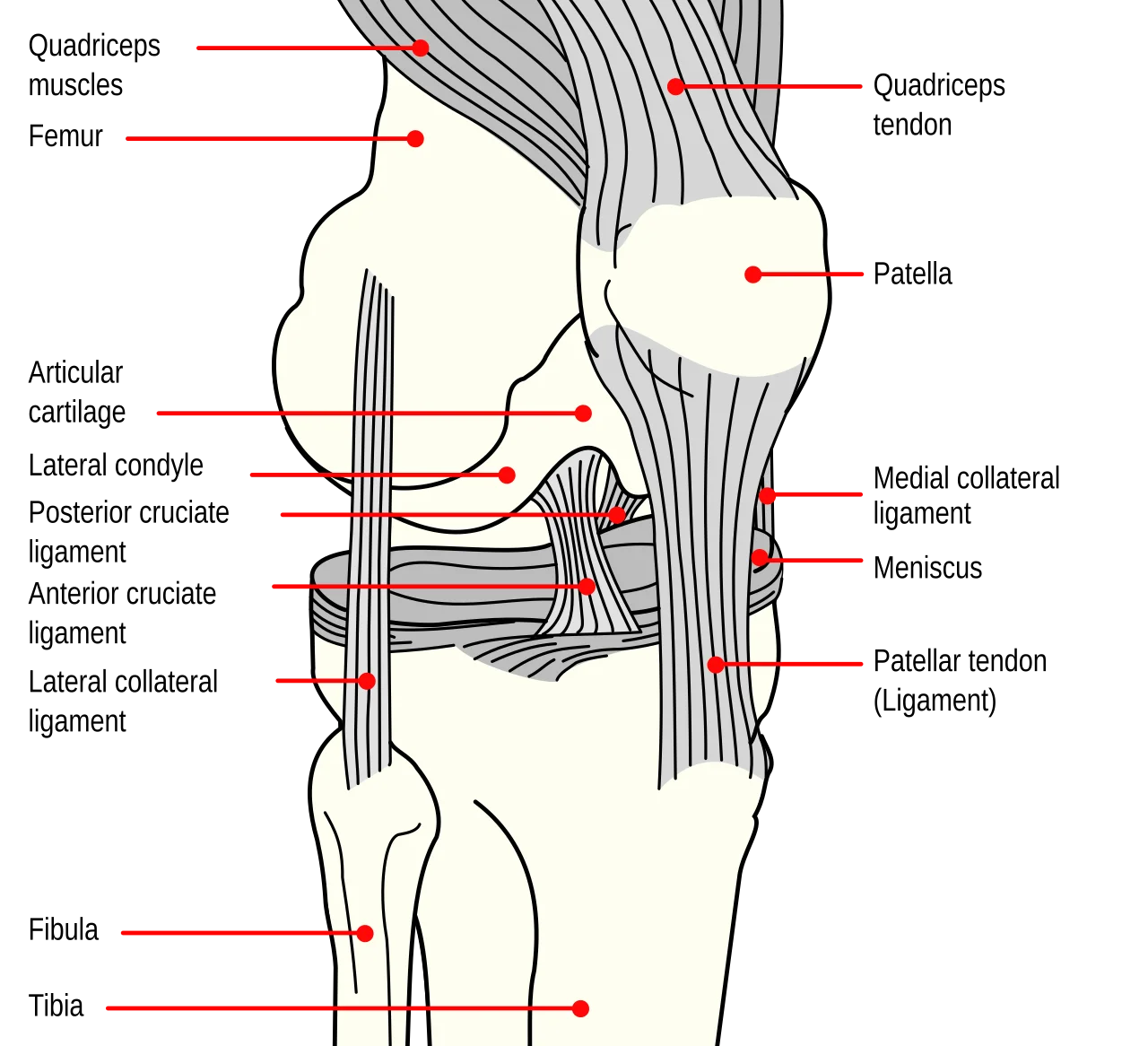
The Anterior Cruciate Ligament (ACL) is a key ligament located in the knee joint, connecting the femur (thigh bone) to the tibia (shin bone). It provides stability by preventing excessive forward movement of the tibia and controlling rotational forces. ACL injuries, often caused by sudden stops, changes in direction, or direct impact, are common in sports like soccer, basketball, and skiing.
The ACL joins the tibia (shin bone) and femur (thigh bone), which also stops the tibia from moving too forward to the femur. Additionally, it aids in regulating the knee joint’s rotational motion. Sports involving abrupt stops, direction changes, or jumping are prone to ACL injuries, which can cause severe knee pain and instability.
Origin and insertion of the ACL
The posterior aspect of the lateral femoral condyle, a bony protuberance on the outside of the thigh bone’s bottom end (the femur), is where the anterior cruciate ligament (ACL) begins. The intercondylar notch, a groove between the two bony prominences on the bottom end of the thigh bone, is directly behind the femoral attachment of the ACL.
The ACL crosses the posterior cruciate ligament (PCL) and attaches to the anterior aspect of the tibial plateau after passing diagonally downward and forward through the middle of the knee joint from its origin. The top portion of the knee joint is made up of the tibial plateau, which is the flat upper surface of the shin bone (tibia).
The anterior tibial spine, a tiny bony protuberance at the front of the tibial plateau, is where the ACL’s tibial attachment is situated. The ACL tibial insertion is a robust, fibrous band of tissue that connects the ACL to the tibial spine.
Mechanism of the anterior cruciate ligament
The anterior cruciate ligament’s (ACL) mechanism includes preventing rotational instability of the knee joint and excessive forward movement of the tibia to the femur. A combination of passive and active stabilization is used to achieve this.
The structural support that the ACL itself provides is referred to as passive stabilization. The ligament, which joins the tibia and femur, is made of robust, fibrous tissue. Its diagonal orientation across the knee joint enables it to withstand rotational and forward forces.
The term “active stabilization” describes how the muscles that surround the knee joint help to maintain healthy ACL function. During movement, the quadriceps, hamstrings, and calf muscles all help to stabilize the knee joint. By regulating the tibia’s movement to the femur, these muscles cooperate to lessen the strain on the ACL.
Running, jumping, and cutting motions are among the physical activities that put a lot of strain on the ACL. An ACL injury may result from these forces causing the ligament to stretch or tear. ACL injuries are frequently caused by abrupt stops or direction changes, direct knee injuries, or awkward jump landings.
In conclusion, the anterior cruciate ligament’s mechanism involves both passive and active knee joint stabilization. The surrounding muscles cooperate to regulate movement and lessen the strain on the ACL, while the ligament offers structural support to stop the tibia from moving too forward and rotating.
Symptoms of the anterior cruciate ligament injury
Depending on how severe the injury is, anterior cruciate ligament (ACL) symptoms can change. Typical signs and symptoms include:
- Abrupt pain: An ACL injury frequently results in abrupt, severe knee pain.
- Swelling: Swelling around the knee joint is a common indicator of ACL damage. It could take a few hours for the swelling to appear, or it could happen right away after the injury.
- Restricted range of motion: The knee joint may have a limited range of motion due to an ACL injury. There may be stiffness or trouble moving the knee.
- Stability: When standing or walking, the knee may feel unsteady or wobbly. This results from the ACL’s loss of stability.
- Some people may experience a popping sound at the moment of the injury, which may be a sign of an ACL tear.
- Weight-bearing difficulty: Pain and instability may make it difficult to bear weight on the injured leg.
- Muscle weakness: If an ACL injury causes muscle weakness in the injured leg, it could be difficult to perform daily tasks.
You must seek medical attention if you suffer from any of these symptoms following a knee injury. A doctor can perform imaging tests and a physical examination to detect an ACL injury and recommend the best option for treatment.
Injuries of the anterior cruciate ligament
Anterior cruciate ligament (ACL) injuries are usually caused by abrupt direction changes, rapid stopping, or landing from a jump. ACL injuries can result from several common activities, including:
- Sports: Due to the abrupt direction changes and pivoting motions required, high-impact sports like football, basketball, soccer, and skiing increase the risk of ACL injuries.
- Gymnastics: The high-risk jumps, landings, and twists that gymnasts frequently execute can cause a lot of strain on the knee joint and raise the possibility of ACL injuries.
- Dance: The repetitive strain that jumps and landings place on the knee joint can cause ACL injuries in dancers.
- Martial arts: Because of their training’s abrupt direction changes and pivoting motions, martial artists are susceptible to ACL injuries.
- Running: Overuse or abrupt direction changes during running can cause ACL injuries in runners.
- Falls: ACL injuries can also result from landing awkwardly after a fall or from falling straight onto the knee.
Keep in mind that anyone can sustain an ACL injury, regardless of their level of fitness or physical activity. ACL injuries are more likely to occur in people who engage in high-impact sports or activities, though.
Treatment of the anterior cruciate ligament injury
The anterior drawer test
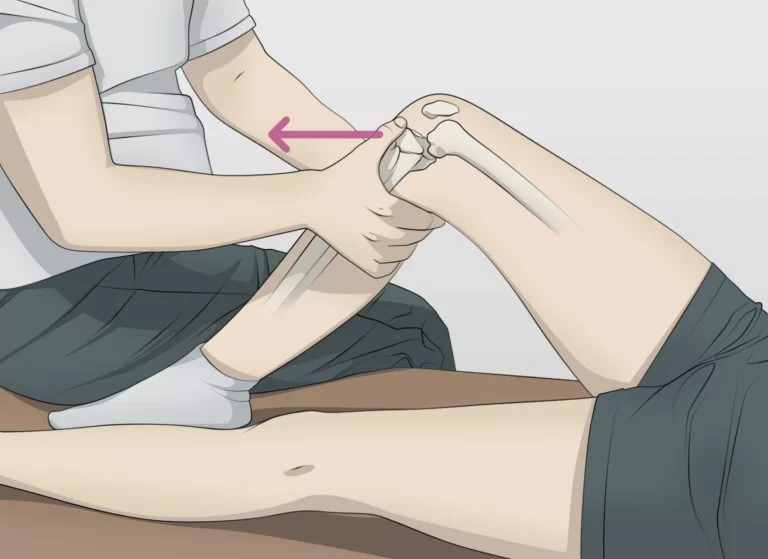
The anterior drawer test is a useful physical examination tool for assessing the knee joint’s anterior cruciate ligament (ACL) health. One of the four main ligaments supporting the knee joint, the ACL is frequently injured during sports or abrupt twisting motions.
The patient lies on their back with their knee bent at a 90-degree angle while performing the anterior drawer test. Placing both hands around the upper portion of the lower leg, just below the knee joint, the examiner sits on the foot of the affected leg.
The examiner then pushes the femur (thigh bone) backward and pulls the tibia (lower leg bone) forward. The way the tibia moves to the femur during an ACL injury is replicated by this motion. The tibia should move forward very little if the ACL is unbroken.
The tibia will move forward excessively if the ACL is torn or partially torn, though, which would indicate a positive test result. On a scale of 0 to 3, the degree of forward movement can be rated; 0 denotes no movement, while 3 denotes substantial movement.
It is crucial to remember that the anterior drawer test is not always accurate and can yield false-positive or false-negative findings. To confirm an ACL injury, it should therefore be used in combination with additional diagnostic procedures like MRI or arthroscopy.
In patients with suspected knee injuries, the anterior drawer test is a straightforward, non-invasive method that can be used to evaluate the ACL’s integrity.
Surgical treatment
ACL reconstruction surgery usually involves using a donor or graft from another area of the body to rebuild the ligament. The procedure is typically carried out under general anesthesia and can be done arthroscopically, which involves making tiny incisions and utilizing specialized tools and a camera to complete the activity.
To position the graft in the same location as the original ACL, tunnels are drilled into the thighbone and shinbone after the torn ligament is removed during surgery. The graft is fastened in position with buttons, screws, or other tools.
Patients usually need to use crutches and wear a brace for a while after surgery to allow for healing. A crucial component of recovery is physical therapy, which aids in regaining the knee joint’s strength, stability, and range of motion.
Although surgically repairing the ACL can be very successful in regaining knee joint function, there are risks involved, including infection, blood clots, and nerve damage. Patients must have a thorough conversation with their surgeon about these risks before the procedure.
Conservative treatment
Non-surgical techniques are used in conservative ACL treatment to control the injury and encourage recovery. This method is usually advised for patients with mild to moderate ACL sprains or partial tears, as well as those who might not be suitable candidates for surgery because of other medical issues.
For ACL injuries, conservative treatment consists of the following primary elements:
- Rest: The first line of treatment for an ACL injury is to keep the knee immobile and refrain from activities that could aggravate it. Limiting physical activity for a while and using crutches to relieve knee weight may be necessary for this.
- Ice: Since swelling and inflammation are typical signs of an ACL injury, applying ice to the knee can help lessen them. Ice should be applied multiple times a day for 20 to 30 minutes at a time.
- Compression: Supporting the knee with a brace or compression bandage can help minimize swelling. Wearing these devices as prescribed by a healthcare professional is advised.
- Elevation: Another way to lessen swelling and encourage healing is to raise the leg above the level of the heart.
- Physical therapy: A physical therapist can collaborate with patients to create an exercise regimen that enhances knee joint stability, strength, and range of motion. This could involve training for balance and agility as well as quadriceps and hamstring strengthening exercises.
- Medications: To treat pain and inflammation, doctors may prescribe over-the-counter painkillers like ibuprofen or acetaminophen.
Depending on the severity of the injury and the patient’s reaction to treatment, conservative treatment for ACL injuries usually takes a few weeks to several months. Over time, patients may be able to resume their regular activities because this method can help reduce pain and increase mobility, even though it might not fully restore knee joint function.
Physiotherapy treatment
ACL (Anterior Cruciate Ligament) physiotherapy exercises are a crucial component of the healing process. The knee joint’s strength, range of motion, and stability are all improved by these exercises. Here are specific physiotherapy exercises for the ACL:
Range of Motion Exercises
Exercises involving range of motion aid in increasing the knee joint’s flexibility and range of motion. Among these exercises are:
- Heel slides involve lying on your back with your legs straight, bending your injured knee slowly, and sliding your heel toward your buttocks. Hold the position for a few seconds, then slowly straighten your leg. Do this ten times.
- Knee Flexion Stretch: Place your feet flat on the floor while sitting in a chair. Sliding your injured foot back slowly will cause your knee to stretch. After a few seconds of maintenance, return to the initial position. Ten times over, repeat.
- Knee Extension Stretch: Place your feet flat on the floor while sitting in a chair. Straighten your injured leg and lift it off the ground. Hold for a few seconds, then drop your leg again. Do this ten times.
Strengthening Exercises
The muscles surrounding the knee joint can be strengthened with the aid of strengthening exercises. Among these exercises are:
- Straight Leg Raises: Maintain a straight posture while lying on your back. Take your injured leg off the ground slowly, then hold it there for a short while. Ten times over, lower your leg back down.
- Wall Squats: Place your feet shoulder-width apart and stand with your back to a wall. Slide down the wall while bending your knees slowly until your thighs are parallel to the floor. After a few seconds of holding, push yourself back up to the beginning position. Do this ten times.
- Hamstring curls: Place a pillow under your hips while lying on your stomach. Raise your heel toward your buttocks while bending your injured knee. Hold for a few seconds, then drop your leg again. Do this ten times.
Balance and Proprioception Training
Training in balance and proprioception aids in increasing knee joint stability. These workouts consist of:
- Single Leg Stance: Keep your other foot off the ground while standing on your injured leg. After a few seconds of holding, move on to the other leg. Do this ten times.
- Bosu Ball Squats: Place your feet shoulder-width apart while standing on a Bosu ball. Squat down while bending your knees slowly. After a few seconds of holding, push yourself back up to the beginning position. Do this ten times.
- Walking on Uneven Surfaces: To test your balance and coordination, walk on uneven surfaces like grass, sand, or gravel.
Gait Training
Teaching the patient how to walk normally with their injured knee is known as gait training. Among these exercises are:
- Heel-to-Toe Walking: Step with your heel squarely in front of your toes while walking in a straight line.
- Sidestepping: Start with your injured leg and move to the other side as you walk sideways.
- Crossover Steps: With each step, cross one foot over the other as you move forward.
Functional Training
Simulating real-life activities that the patient might experience after recovery is known as functional training. Among these exercises are:
- Jumping: To get better at jumping, clear small obstacles or cones.
- Running: Increase your speed gradually after beginning with a slow jog.
- Cutting and Pivoting: To get ready for sports requiring quick direction changes, practice cutting and pivoting movements.
ACL physiotherapy exercises are, in summary, a crucial component of the healing process. The knee joint’s strength, range of motion, and stability are all improved by these exercises. A customized exercise regimen will be created by the physiotherapist based on the patient’s unique requirements and objectives. Consistently following the exercise regimen is crucial, as is discussing any pain or discomfort experienced during the exercises with the physiotherapist.
Risk factors for ACL Injury
The anterior cruciate ligament, or ACL, is one of the knee joint’s four main ligaments. It serves to stabilize the knee during movement by joining the tibia (shin bone) and femur (thigh bone). However, the ACL is also prone to injury, especially in athletes who play high-impact sports like football, basketball, and soccer. The following are specific risk factors for ACL injuries:
- Gender: Women are more likely than men to sustain an ACL injury. This can result in a greater angle between the thigh and shin bones, placing more strain on the ACL, as women typically have a wider pelvis and a smaller notch in the femur.
- Age: Adolescents and young adults are more likely to sustain an ACL injury than older people. This is because their muscles and bones are still growing, which leaves them more vulnerable to harm.
- Sports Participation: Players who play high-impact sports like football, basketball, and soccer are more likely to sustain an ACL injury. The knee joint may be strained by the abrupt stops, starts, and direction changes that these sports require.
- Prior Injury: People who have previously sustained an ACL injury are more likely to experience another one. This is because the ligament might still be weak from the prior injury or might not have completely healed.
- Poor Conditioning: People who lack physical fitness or who have weak, strained muscles are more likely to suffer an ACL injury. This is because weak muscles put more strain on the ligaments by failing to adequately support the knee joint.
- Footwear: The risk of an ACL injury can be raised by wearing inappropriate footwear, such as shoes that don’t offer enough support or traction.
- Playing Surface: Playing on too-hard or too-soft surfaces, like sand or concrete, can make an ACL injury more likely.
Ultimately, some risk factors for ACL injuries include age, gender, participation in sports, prior injuries, poor footwear, playing surface, and poor conditioning. Playing on safe surfaces, wearing appropriate footwear, and maintaining a high level of physical fitness are all important ways to lower these risk factors. ACL injuries can also be prevented and healing accelerated by getting medical help as soon as possible and adhering to a rehabilitation program.
Preventing injuries to the anterior cruciate ligament
ACL injuries can be avoided by a combination of strategies that target the risk factors mentioned above. The following strategies can help you avoid ACL injuries:
- Strengthening exercises: To support the knee and lessen the strain on the ACL, strengthen the muscles surrounding the knee joint, especially the hamstrings and quadriceps. Leg presses, lunges, and squats are a few examples of beneficial exercises.
- Exercises for flexibility: Stretching can help increase knee joint range of motion and flexibility, which lowers the chance of injury. Examples include stretches for the quadriceps, hamstrings, and calves.
- Wearing shoes that offer sufficient traction and support can help lower the risk of an ACL injury. It is advised to wear shoes with a non-slip sole and adequate arch support.
- Safe playing surface: You can lower your chance of suffering an ACL injury by playing on safe surfaces like grass or turf. Steer clear of hard or uneven surfaces like sand or concrete when playing.
- Technique: Playing sports with the right technique can lessen the strain on the knee joint and lower the chance of suffering an ACL injury. Trainers and coaches can offer advice on appropriate techniques.
- Protective equipment: For athletes who have already experienced an ACL injury, wearing protective equipment like knee pads or braces can help lower the risk of an ACL injury.
- Rest and recuperation: ACL tears and other overuse injuries can be prevented by taking some time to rest and recover after intense exercise. For general health and injury prevention, getting enough sleep, staying hydrated, and eating a healthy diet are essential.
In conclusion, a comprehensive approach that considers the various risk factors is required to prevent ACL injuries. By taking these precautions, people can lower their chance of suffering an ACL injury and keep their knees healthy.
FAQs
How is a diagnosis of an ACL injury made?
A physical examination, which includes the anterior drawer test, and imaging tests like MRIs and X-rays are usually used to diagnose an ACL injury.
How does an ACL injury manifest itself?
Pain, swelling, instability, or a giving-way sensation in the knee, and trouble walking or bearing weight on the injured leg are all signs of an ACL injury.
How do you treat an ACL injury?
Physical therapy, bracing, rest, ice, compression, and elevation (RICE), and in certain situations, surgery to rebuild or repair the ligament are all possible treatments for an ACL injury.
Is it possible to prevent an ACL injury?
Although preventing an ACL injury isn’t always possible, some steps can help lower the risk, like stretching and warming up properly, exercising or playing sports with the right form, and wearing the right protective gear.
References
- Patel, D. (2023b, July 29). Anterior cruciate ligament – anatomy, structure, function, injury. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/anterior-cruciate-ligament/




2 Comments