Allergic Reactions
Allergic reactions occur when the immune system overreacts to a normally harmless substance, such as pollen, food, or medication. They can range from mild symptoms like sneezing, itching, or rashes to severe, life-threatening responses such as anaphylaxis. Early recognition and proper management are key to preventing complications.
Introduction
When the immune system overreacts to a substance that most people believe to be harmless, it might result in an allergic reaction. These substances are known as allergens, and they can include things like pollen, certain foods, pet dander, insect stings, and even some medications. The immune system attempts to fight off these chemicals because it believes they are dangerous attackers, such as bacteria or viruses, rather than ignoring them.
The symptoms of this response can differ depending on both the specific allergen and the person’s unique sensitivity. Mild side effects, including rashes, watery eyes, itching, or sneezing, may occur in certain persons. The response can become considerably more harmful in more severe situations and result in anaphylaxis.
Anaphylaxis is a severe, possibly fatal allergic response that might need rapid medical treatment and cause breathing difficulties and a decrease in blood pressure. Although allergies are prevalent and may impact people of all ages, each person may experience them differently in terms of severity and triggers.
What are Allergic Reactions?
Your body is protected from possible dangers by your immune system, which frequently serves as a personal bodyguard. Every day, it puts in much effort to protect you from dangerous substances like viruses, bacteria, and germs. To prevent illness, your immune system identifies and combats harmful substances that attempt to enter your body.
However, the immune system might become confused at times. In the case of allergies, it perceives something harmless as a threatening outsider, such as dust, pollen, pet dander, or certain foods. The immune system overreacts and attacks these items even if they aren’t dangerous. Sneezing, itching, a runny nose, and other allergy symptoms, as well as more severe issues like trouble breathing, are caused by this overreaction.
Your immune system isn’t malfunctioning when you have allergies; rather, it’s overworking itself and responding to things that aren’t dangerous.
Regretfully, even though this allergen isn’t dangerous, your immune system views it as such. It begins to get ready for what it believes to be a serious assault. Sensitization is the term for this early stage, during which your body is “preparing” to react should it come into contact with that allergen again.
Your immune system produces unique proteins known as antibodies to do this. Immunoglobulin E, or IgE antibodies, are the particular kind that is produced for allergies. Like little soldiers, these IgE antibodies have been taught to identify that particular allergen. They attach to certain cells in your body known as basophils and mast cells, which are components of your immunological defense system.
Your body remembers the allergen when it comes into contact with it again, such as pollen, peanuts, or pet dander. Your body’s unique defenses, known as IgE antibodies, detect the allergen rapidly.
These antibodies generate a warning signal after binding to the allergen.
Other immune cells then take over.
One of the most potent compounds they generate is histamine.
Histamine causes allergy symptoms like:
- Sneezing
- Itchy eyes
- Swelling
- Trouble breathing
This is your body trying to fight something it thinks is dangerous — even if it’s not.
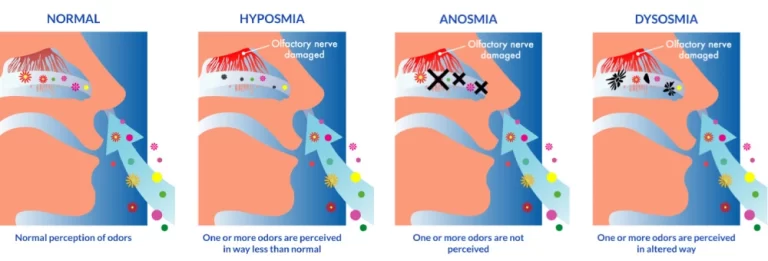
The Part Histamine Plays: The molecule responsible for allergic symptoms is histamine.
When discharged, it results in:
- Redness and swelling.
- Skin irritation
- Hives or swelling
- Frequent sneezing or a runny nose
- Breathing problems
- Your body is attempting to protect you, but it goes too far!
Types of Allergic Reactions
From minor symptoms to serious, life-threatening diseases, allergic responses can take many forms. Based on the immunological mechanism at play, these responses are divided into four kinds, which are commonly referred to as Type I through Type IV. Let’s examine every type in more detail:
Type I: IgE-Mediated Reactions, or Immediate Hypersensitivity
This kind of allergic reaction, also known as anaphylaxis or acute hypersensitivity, is the most prevalent and well-known. It happens quickly, typically within minutes after being exposed to the allergen, and involves the IgE antibody.
The mechanism
The immune system creates IgE antibodies that are specific to an allergen when a person becomes sensitive to it (due to previous exposure). These IgE antibodies attach to immune system-related white kinds of blood cells known as basophils and mast cells.
The allergen attaches itself to the mast cells’ or basophils’ IgE upon repeated exposure, triggering the release of histamine and other substances from the cells.
Blood vessel dilatation caused by histamine results in sensations including redness, swelling, and itching in the affected regions. Additional symptoms like mucus production and bronchoconstriction (difficulty breathing) can be caused by other substances.
Typical Triggers:
- Hay fever pollen
- Dust mites
- Dander from pets
- Food allergies (such as shellfish and peanuts)
- Stings from insects (wasps or bees)
- Drugs (such as penicillin)
Symptoms
Symptoms include urticaria, hives, or rashes; itching, especially in the skin, eyes, or throat; swelling (angioedema), especially around the lips, face, or throat; hay fever-related coughing, sneezing, and nasal congestion; and anaphylaxis, a severe allergic reaction that can cause shock, breathing difficulties, or even death.
Type II: Antibody-Mediated Reactions, or Cytotoxic Hypersensitivity
The hallmark of type II hypersensitivity is the immune system’s killing of cells it recognizes as alien, usually using IgG or IgM antibodies.
The mechanism
In response to antigens on the surface of either the body’s cells or foreign cells (such as transfused blood), the immune system generates antibodies (IgG or IgM).
By attaching themselves to the target cells, these antibodies designate them for destruction by immune cells, such as complement proteins or phagocytes. Inflammation and tissue damage may result from the death of these cells.
Typical Triggers:
- Reactions to blood transfusions (when the incorrect blood type is given)
- Autoimmune hemolytic anemia
- Reactions caused by drugs (such as thrombocytopenia from heparin or certain antibiotics)
- Graves’ disease is characterized by antibodies that attack thyroid cells.
Signs and symptoms
Red blood cell breakdown, or hemolysis, results in symptoms including fatigue, pallor, and dyspnea.
Jaundice, or skin yellowing, caused by liver damage, can harm organs if left untreated.
Type III: Hypersensitivity Mediated by the Immune Complex
Immune complexes identified as type III responses, or antigen-antibody complexes, collect in tissues and cause inflammation and injuries.
The mechanism
IgG and IgM antibodies interact with soluble antigens, forming immune complexes as part of the body’s defense response.
These complexes can accumulate in blood arteries, joints, or kidneys, causing inflammation and drawing white blood cells that might harm the tissues.
Inflammatory mediators are released when the immune complex deposition activates the complement system.
Typical Triggers:
- Systemic lupus erythematosus, or SLE, is a disease in which immune complexes build up across multiple organs.
- It is rheumatoid arthritis.
- Serum sickness (a response to antiserum and other medicines)
- The name for kidney damage that occurs after a streptococcal throat infection is post-streptococcal glomerulonephritis.
Signs and symptoms
- Swelling, joint discomfort, and rash (in diseases like lupus)
- Malfunctioning of the kidneys (as shown in glomerulonephritis)
- Vasculitis is an inflammation of the blood vessels that can result in ulcers or skin rashes.
Type IV: Cell-Mediated Delayed-Type Hypersensitivity
T cells, not antibodies, mediate type IV responses, which are delayed (taking hours to days to appear).
The mechanism
T-helper cells, particularly Th1 cells, are activated and release cytokines in response to an allergen encountered by someone with Type IV hypersensitivity.
Other immune cells, including macrophages, are drawn to and activated by these cytokines, resulting in tissue injury and inflammation at the exposure site.
T-cell activation and immune cell infiltration require time, which causes the reaction to be delayed.
Frequent Triggers:
- Dermatitis from contact (such as nickel or poison ivy)
- Skin tests for tuberculosis are examples of delayed hypersensitivity.
- Graft rejection, also known as transplant rejection
- Prolonged allergic responses (such as those caused by infections or certain drugs)
Signs:
swelling and soreness where the exposure occurred
Increase the size of the lymph nodes
A raised, hardened bump at the injection site may be the outcome of a TB test, indicating earlier exposure to TB.
Common Allergic Triggers
Many different things, such as food, environmental conditions, insect stings, drugs, and latex, can cause allergic responses. A thorough explanation of some of the typical allergy triggers is provided below:
Allergies to Food
Food allergies happen when certain proteins in meals are incorrectly seen by the immune system as dangerous, leading to an immunological reaction. Allergy responses are more prone to occur in certain foods than others.
Typical Food Allergens
Nuts: Particularly tree nuts like cashews, hazelnuts, walnuts, and almonds, as well as peanuts, which are beans. Among the most common are peanut allergies, which can result in serious side effects, including anaphylaxis.
Eggs: Although many overcome their egg allergy as they become older, they are frequent in youngsters. Egg white proteins are usually the source of the allergy, while some persons may also experience reactions to egg yolk proteins.
Milk: Casein and whey are two proteins that cause an allergy to cow’s milk, which is usually present in newborns and early childhood.
Wheat: Unlike gluten intolerance or celiac disease, wheat allergies can result in symptoms that range from minor skin responses to anaphylaxis.
Soy: Infants are more likely to be allergic to soybeans and soy products, which can cause symptoms including rashes, constipation, or anaphylaxis.
Fish: Although fish allergies are often lifelong, they can still result in responses to fish (such as salmon, tuna, and cod).
Symptoms
- lip, tongue, or throat swelling.
- Rashes or hives
- Vomiting, diarrhea, or nausea
- Breathing difficulties or wheezing
- itching in the tongue
Allergies to the Environment
Environmental allergens are compounds that can cause allergic responses that are found in the air or the surrounding environment. While some of these allergies can exist all year round, others are frequently seasonal.
Pollen is one of the most prevalent environmental allergens, particularly during the spring and fall seasons. Triggers include pollen from grass.
Pet Dander: Allergy responses can be triggered by proteins present in the skin flakes, saliva, and urine of pets, particularly dogs and cats. Allergies to pets may persist throughout the year if the animal is housed.
Microscopic organisms known as dust mites live in dust, bedding, and carpets. Their excrement is extremely allergenic and can trigger allergic reactions, especially during the winter when humans spend more time indoors.
Mold Spores: Mold grows best in moist conditions, and breathing in its spores can trigger allergic responses. Pollen from grass, plants (like ragweed), and trees (including oak, birch, and cedar) are common triggers.
- Sneezing, runny, or stuffy nose
- Itchy throat, nose, or eyes
- Wheezing or coughing
- Rashes on the skin, such as eczema
The attacks of insects
Some people may experience mild to severe allergic responses to insect stings. An allergic response is more likely to occur in people who have previously been harmed.
Common Allergy-Inducing Insects:
Bees: Bumblebees and honeybees can sting repeatedly, injecting poison into the skin.
Wasps: Wasps are frequently more aggressive and can sting several times.
Hornets: Wasps’ larger relatives, hornets may sting and produce severe responses.
Fire Ants: When they sting, they inject a poisonous bite which can trigger an allergic reaction, particularly in people who have already had sensitivity.
Symptoms
- pain, swelling
- redness, rash, or hives
- Breathing difficulties, pressure in the chest, or throat swelling (anaphylaxis symptoms)
- Vomiting or feeling sick
Allergies to Medication
Some people may experience allergic reactions when using certain drugs. The allergy may be caused by the medication itself or one of its ingredients.
Typical Drugs That Induce Allergies
Antibiotics like penicillin and others: These drugs are among the most likely to trigger allergic responses, which can range from minor skin rashes to life-threatening anaphylaxis.
Non-steroidal anti-inflammatory medicines (NSAIDs): Some people may experience adverse responses to medications such as aspirin or ibuprofen.
Sulfa medications: Some people may experience adverse responses to medications such as sulfonamide antibiotics.
Drugs used for anesthesia: Some people have allergies to either local or general anesthetics used in operations.
Symptoms
- hives or a rash
- swelling of the throat, face, or lips
- Breathlessness or wheezing
- Fever (sometimes)
Allergy to Latex
When a person’s immune system responds to proteins in natural rubber latex, latex allergies can result. Exposure to latex-containing items, including gloves, balloons, or medical equipment, can cause this.
Latex gloves, particularly in medical environments
Balloons or rubber bands
Condoms are composed of latex
Medical equipment such as stethoscopes, catheters, and other tubes
Symptoms of Allergic Reactions
Skin Reactions
The skin is often the first place where allergy symptoms show up, especially in food, medication, and contact allergies.
Common Skin Symptoms:
Hives (Urticaria): Urticaria, or hives, are itchy, elevated welts that can develop anywhere on the body. They vary in size and may appear either red or match the skin tone.
Eczema (Atopic Dermatitis): Chronic, itchy, inflamed patches of skin. Frequently observed in those who have asthma or other allergies.
Angioedema refers to swelling that occurs in the deeper layers of the skin, often impacting areas such as the eyelids, lips, hands, feet, or throat. It may appear on its own or in combination with hives, and can sometimes lead to serious complications if the throat is involved.
Itching or Redness: Especially in cases of contact dermatitis or insect stings.
Respiratory Problems
Breathing can be affected by allergens that are inhaled (such as mold, pollen, or pet dander) or that cause systemic reactions (such as food or drug allergies). Frequent respiratory issues often present as a runny nose and bouts of sneezing, hallmark indicators of allergic rhinitis, commonly referred to as hay fever.
Another typical symptom is nasal congestion, where the nasal passages become inflamed, swollen, or obstructed. Additionally, individuals may experience coughing or wheezing, which can signal irritation or constriction in the airways. This is caused by constricted airways and is frequently misdiagnosed as asthma.
Gastrointestinal symptoms include:
Nausea and vomiting, which usually happen shortly after exposure to the allergen; stomach cramps or pain, which are frequently severe and cannot be relieved by standard remedies; diarrhea, which may accompany other GI symptoms or occur on its own; and bloating or gas, which are less common but can happen with food sensitivities.
Signs of Cardiovascular Disease
The cardiovascular system may be impacted by anaphylaxis and other more severe allergic responses.
Typical cardiovascular symptoms include hypotension, or low blood pressure, which can result in lightheadedness, fainting, or disorientation.
An irregular or fast pulse is frequently a compensatory reaction to a decline in blood pressure.
Fatigue or a feeling of lightheadedness can result from insufficient blood flow to the brain, leading to reduced oxygen and nutrient delivery, which impairs normal brain function.
Shock: A potentially deadly illness that needs to be treated right away.
Diagnosis
When a person develops an allergy, their body interprets innocent substances like dust, pollen, or specific foods as dangerous. Doctors utilize a range of diagnostic methods to identify the underlying triggers behind these symptoms. Two commonly used approaches for identifying allergies include undergoing allergy tests and keeping a detailed symptom diary. These methods help pinpoint specific triggers by tracking exposure and corresponding reactions over time.
Prick Test for Allergies
One of the simplest and most popular ways to check for allergies is with this test. Here’s how it works: A doctor applies little droplets of different probable allergens (such as pollen, pet dander, or food extracts) on your skin, generally on the forearm or back.
A tiny needle is then used to lightly prick the skin beneath each drop. After around 15–20 minutes, the doctor examines to see whether your skin responds (such as getting red or puffy).
If a lump or hive emerges where a specific material was tested, it typically signifies you’re allergic to that thing.
Blood Examinations
In cases when a skin test is not possible, your physician could recommend a blood test.
For certain allergens, the lab measures the amount of IgE, a kind of antibody your body produces after an allergic reaction. You may be allergic to a substance if your IgE levels are high for it.
Maintaining a Symptom Record
Allergy testing doesn’t always provide definitive results. That’s when a symptom journal might be really helpful.
How to keep one is as follows.
Write down everything you consume or come into contact with throughout the day, such as meals, pets, pollen levels, new soaps, etc. Make a note of the day and time when you have symptoms such as breathing difficulties, rashes, stomach problems, or sneezing.
Keep track of where you are (for example, outside, at a friend’s house, close to animals, etc.). Add details about your everyday schedule, such as the medications you take or the amount of sleep you get.
Treatment
There are numerous ways to treat allergies, depending on how mild or severe the symptoms are. Here are the most popular treatments:
Antihistamines, which come in a variety of forms, including pills, liquids, nasal sprays, and eye drops, are among the most widely used allergy medications. They help prevent the effects of histamine, a chemical your body releases during an allergic reaction, and they reduce symptoms like sneezing, itching, a runny nose, and watery eyes. Many of these medications are available over the counter and are effective for mild allergies like hay fever or pet allergies.
Corticosteroids can be taken as nasal sprays, creams, inhalers, eye drops, or even pills (for more severe allergies). Nasal sprays like fluticasone (Flonase) are excellent for treating stuffy noses from dust or pollen allergies, and creams can be used for itchy, allergic skin rashes like eczema. Corticosteroids reduce inflammation, which is the swelling and irritation caused by an allergic reaction.
EpiPen (Epinephrine Injector) An EpiPen is used in emergencies for a severe allergic reaction, called anaphylaxis. Breathing difficulties, edema, a reduction in blood pressure, or even death may result from anaphylaxis. An EpiPen gives a quick dose of epinephrine, which helps reverse these symptoms right away. People who are allergic to things like peanuts, bee stings, or shellfish often carry one with them all the time—just in case.
Immunotherapy for Allergy Shots
To treat this for a longer period, immunotherapy is used, which is also called allergy injections. Injections contain very small quantities of the specific allergen that triggers your allergic reaction.
Your body becomes less sensitive as it adapts to it.
Over several years, you gradually transition from receiving numerous injections (often once a week) to once a month. Strategies for Avoiding Allergic Reactions
Avoidance advice according to the kind of allergy.
Examining labels and making your house allergy-proof. Keeping emergency prescription drugs on hand.
How to Prevent Allergic Reactions
Avoiding the items that cause your allergy is the key to preventing allergic responses. Even though this might be difficult, there are wise things you can do to keep yourself comfortable and secure.
Avoidance Advice (According to the Type of Allergen)
The first step is identifying your particular allergy. After that, you can stay as far away from that allergy as you can.
Allergies to Food
Check food labels carefully for allergies such as dairy, shellfish, nuts, or wheat.
When dining at eateries, inquire about the ingredients.
Steer clear of cross-contamination by not using the same knife for jam and peanut butter.
Inform people about your allergy, particularly at school or social gatherings.
Allergies to Pollen
During days with high pollen levels, stay indoors and monitor the pollen forecast.
Use air conditioning with clean filters and keep windows closed.
Allergies to Dust Mites
Cover pillows and mattresses with dust mite-proof materials.
Every week, wash bedding in hot water.
If at all possible, take out the heavy curtains and rugs.
Allergies to Mold
Maintain a dry and well-ventilated house.
In moist spaces like bathrooms or basements, use dehumidifiers.
Quickly remove mold from windows, walls, and showers.
Allergies to Insect Stings
Avoid the sweet-smelling fragrances and flowering plants outside.
Avoid wearing clothing with bright colors, and wear shoes when you’re outside.
Avoid drinking from open bottles or cans as they may harbor insects.
How to Read Labels and Make Your Home Allergy-Proof
- Always look for allergy warnings such as “made in a facility with tree nuts” or “contains peanuts.”
- Recognize hidden substances, such as “albumin” for eggs or “casein” for dairy.
- Protecting Your Home from Allergies
Make use of HEPA filters in both your air purifier and vacuum. - Keep surfaces clean regularly, particularly in kitchens and bedrooms.
When to see a doctor?
- In order to contact emergency services, dial 911 or the local number. As soon as you have any breathing difficulties
- Your throat is swollen or feels constricted.
- Your lips, tongue, or cheeks swell up rapidly.
- You feel faint, lightheaded, or lightheaded.
- Your heart beats quickly.
- You are experiencing a severe allergic reaction, particularly if you have already had anaphylaxis.
- Consult a physician right away if you:
- Have a persistent rash, hives, or swelling
- Feel nauseous, throw up, or have stomachaches after consuming specific meals.
- Observe fresh or worsening symptoms of allergies
- Get a test for that, as you are not aware of the causes.
- Do you need guidance on how to handle recognized allergies or a prescription for an EpiPen
Conclusion
How we respond to unforeseen circumstances may be greatly impacted by our awareness and readiness. Learning and preparing in advance can help us stay safe and composed in the event of a natural disaster, a domestic issue, or even a disruption in our regular schedule. Being aware of your surroundings include keeping up with current events. Being prepared include having a strategy and the necessary equipment on hand.
Discuss emergency preparations with your loved ones, prepare a few necessities, and remain informed from reliable sources. When it counts most, these little steps can help you feel more at ease and have a significant impact.
FAQs
How does an intolerance vary from an allergy?
The immune system is impacted by allergies, which can be dangerous. An intolerance that affects digestion, such as lactose intolerance, is usually less problematic.
What signs of an allergic response are common?
Sneezing, itching, rashes, swelling, hives, runny nose, watery eyes, nausea, or trouble breathing are some of the mild to severe symptoms.
Anaphylaxis: What is it?
A severe, sometimes fatal allergic response, anaphylaxis, can result in breathing difficulties, swelling, a reduction in blood pressure, and unconsciousness. It has to be treated by a doctor right now.
What is a skin prick test?
Tiny quantities of allergens are applied to your skin as part of a diagnostic test to look for signs of an allergic reaction, such as swelling or redness.
Which drugs are used to treat allergies?
Immunotherapy may aid in long-term maintenance, and common treatments include decongestants, corticosteroids, antihistamines, and epinephrine for emergencies.
Is it possible to treat allergies?
Although the majority of allergies cannot be cured, they can be successfully controlled with medicine, avoidance, and occasionally allergy injections or oral immunotherapy.
What needs to be included in an emergency pack for allergies?
Add medical identification, an emergency action plan, antihistamines, and an EpiPen. Keep asthma inhalers on hand as well, if recommended.
References
- Allergies. (2025, April 4). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8610-allergies
- Burke, D. (2023, April 21). What is an allergic reaction? Healthline. https://www.healthline.com/health/allergies/allergic-reaction
- Felman, A. (2023, April 25). Everything you need to know about allergies. https://www.medicalnewstoday.com/articles/264419#diagnosis
- Website, N. (2024, November 25). Allergies. https://www.nhs.uk/conditions/allergies/
- Allarakha, S., MD, & D, D. J. P. (2022, March 4). What are the 4 types of allergic reactions? symptoms. MedicineNet. https://www.medicinenet.com/what_are_the_four_types_of_allergic_reactions/article.htm