Acromioclavicular Joint
The acromioclavicular joint, frequently referred to as the AC joint, is an essential anatomical structure situated on the top of the shoulder where the lateral end of the clavicle (collarbone) articulates with the acromion process of the scapula.
This joint is critical to the stability and operation of the shoulder complex, allowing for a wide range of motion while preserving the structural integrity of the shoulder girdle.
The AC Joint, which joins the scapula and clavicle, is the major articulation that separates the upper extremities from the trunk.
Introduction
One of the four joints that form the shoulder complex is the AC joint, also known as the articulioclavicular joint. The primary articulation that interrupts the upper limbs from the trunk and connects the scapula to the clavicle is the AC Joint.
The AC Joint’s principal purpose is:
- To provide more thoracic rotational range for the scapula.
- To accommodate the thorax’s developing structure as the arm goes, allow for scapula alterations (tipping and internal/external rotation) outside of the original plane.
- The clavicle’s flexion and extension are accommodated by the upper limb by the joint.
Structure of Acromioclavicular Joint
The acromion process, which arises anteriorly from the scapula, establishes contact with the lateral clavicle to develop the diarthrodial acromioclavicular joint. It provides the scapula with an extra range of motion and facilitates arm movements like shoulder abduction and flexion since it connects the scapula to the thorax. It also makes it possible for the forces in the upper arm to be transmitted to the rest of the skeletal system.
Protecting the AC joint is a capsule that is surrounded by the synovial membrane. An intra-articular cartilaginous disk is situated in the interstitial area.
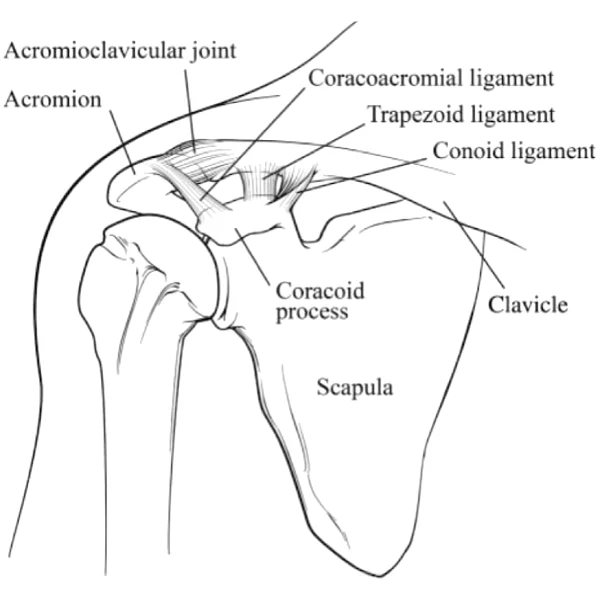
Stabilize the joint with three primary ligaments. The upper, lower, anterior, and posterior parts form the acromioclavicular ligament (AC). They insert on the distal clavicle’s underside posteromedially and posteriorly, respectively. Its primary goal is to keep things stable in a vertical direction. A robust triangle band called the coracoacromial ligament maintains vertical stability by joining the coracoid process to the acromion.
Anatomy of Acromioclavicular Joint
Articulating Surfaces
The articular facets’ varied configuration is the reason for their observed incongruence. In both orientations, they can be convex-concave, flat, or reversed (convex-concave). Different people have different articulating surface inclinations.
Three types of joints are related, and they have reaching surfaces given at angles between 16 and 36 degrees from vertical. The wear effects of shear forces were more likely to impact the joint as the surfaces approached verticality. The intra-articular movements of this joint are unpredictable due to its different articular structure.
Joint Capsule
A narrow capsule enclosing the AC Joint is lined with synovium material. The deltoid and trapezius attachments, which fortify the inferior and superior capsular ligaments even more, support the feeble capsule.
The acromioclavicular joint’s joint capsule surrounds its two articular surfaces. It has an internal synovial membrane lining and a loose layer of fibrous tissue on top.
Trapezius muscle fibers strengthen joint capsule posteriority.
Ligament of Acromioclavicular Joint

Three ligaments improve the joint, including the acromioclavicular ligament, which distributes to the scapular acromion and clavicle.
Clavicle ligament’s superior crook This ligament, which is a quadrilateral band, connects the neighboring portion of the acromion’s top surface to the upper segment of the clavicle’s lateral end. The articulation’s upper region has been explored.
It is formed up of parallel fibers that cover around the aponeuroses of the Trapezius and Deltoideus. It comes into contact with the fibers beneath the disc when the articular disc is present.
This ligament, which covers the articulation’s underside, is a little thinner than the one before it and is joined to the surfaces of the two nearby bones.
The supraspinatus tendon below and, in some cases, the articular disc above are connected.
The acromion is located directly in front of the clavicle’s articular surface, and its broad base, which reaches the whole length of the coracoid process’ lateral border, joins it to it at its apex.
According to the acromion and coracoid process, this ligament builds a vault that protects the humeral head.
With a bursa in between, it is attached to the clavicle above, the Deltoideus below, and the Supraspinatus tendon below.
The tendons of the supraspinatus and infraspinatus form a thick lamina beneath the Deltoideus, continuing its lateral borders.
Two peripheral bands that join at the acromion and a thinner intermediate zone are sometimes used to characterize the ligament.
The intervening segment of the ligament is compromised when the Pectoralis minor partially penetrates the shoulder capsule rather than the coracoid process. This causes the Pectoralis minor to pass between these two bands.
Although it is not a member of the articulation of the acromioclavicular joint, it is commonly discussed as such since it serves as the most efficient means of maintaining clavicle-acromion contact.
The Trapezius muscle is attached to these ligaments in the back, and the Subclavius and Deltoideus muscles in the front.
Coracoclavicular Ligaments: The conoid and trapezoid ligaments are the components of the coracoclavicular ligaments, however, they do not connect the joint. For the AC Joint, this combined ligament serves as its main support. Due to their support of horizontal stability, these ligaments play a major role in preventing superior dislocation of the AC joint. Additionally, both parts restrict the scapula’s rotation. The coracoclavicular ligament’s primary function is to cause the clavicle’s longitudinal rotation, which is required for a complete range of motion while elevating the upper limb.
- The conoid ligament is the most significant fan-shaped portion of the coracoclavicular ligament. This ligament is more midway than the trapezoid ligament.
- The more laterally situated portion of the quadrilateral coracoclavicular ligament is called the trapezoid ligament.
The primary resistance against posterior translation and posterior axial rotation at the AC joint, which shields the joint capsule, is the acromioclavicular ligament.
Joint Disc
Individuals, sides of the same individual, and people of different ages all have different joint discs. The joint is a fibro-cartilaginous alliance throughout the first two years of life. Each articulating surface has a growing joint space, which can culminate in a remnant of meniscoid fibrocartilage inside the joint when the upper limb is being used.
Muscles around the Acromioclavicular Joint
The clavicle is associated with numerous muscles that relate to the head and upper limbs. These muscles include:
- Pectoralis Major (Clavicular Head)
- Sternocleidomastoid
- Deltoid
- Trapezius
The acromioclavicular joint’s muscles
When the scapula moves laterally and increases on the AC joint, the descending and transverse portions of the trapezius muscle pull the acromion, scapula spine, and lateral third of the clavicle superomedially.
The scapula will improve if the levator scapulae muscle relaxes simultaneously with the rotation.
The clavicle’s medial end descends on the sternoclavicular joint after these motions.
The serratus anterior can be firmly depressed if required by the pectoralis minor and inferior fibers. Following these movements, the clavicle’s sternal end is raised on the sternoclavicular joint.
The serratus anterior and pectoralis minor muscles primarily extend the scapula at the AC joint, whereas the rhomboid minor and major muscles and the trapezius muscle’s horizontal and ascent regions contract to retract it. The sternal end of the clavicle moves anteriorly during protraction and posteriorly during retraction on the sternoclavicular joint.
Blood Supply the Acromioclavicular Joint
The following is how the acromioclavicular joint’s vascular supply is acquired:
- After establishing the thyrocervical trunk, the subclavian artery supplies the suprascapular artery.
- Over time, the axillary artery changes into the thoracoacromial artery.
The main arteries have been accompanied by venous drainage.
Innervation
Lateral pectoral and suspensory nerves encourage the acromioclavicular joint. Despite the fact that the lateral pectoral nerve opens in the lateral cord, the suprascapular nerves get involved in the upper trunk of the brachial tract.
Function
The AC Joint’s primary function is to improve the scapula’s range of motion in the thorax. Permit scapular alterations (tipping and internal/external rotation) beyond the scapular’s initial plane so that it can track the thorax’s evolving shape following arm movement.
The AC Joint’s primary function is to improve the rotational mobility of the scapula on the thorax. Allow for scapular modifications (tipping and internal/external rotation) outside of the scapular’s initial plane to be able to follow the changing form of the thorax after arm movement.
Forces from the upper extremities can travel through the joint and onto the clavicle. The Scapulothoracic Joint is normally moved by combining the sternoclavicular and acromioclavicular movements. This movement consists of:
The scapula rotates about 30 degrees up and down with the acromion throughout flexion and abduction, and a further thirty degrees up and down with the acromion at adduction and extension.
Movement of the exterior and interior surfaces around a nearly vertical axis. The scapula rotates inward at the AC level during protraction and externally during retraction according to the form of the postero-lateral thorax.
The AC’s dome-shaped thorax is embraced by the scapula through anterior tilting during elevation and posterior tilting during depression.
Movements
This articulation is meant to facilitate scapular movements that are necessary to realign the glenohumeral joint.
Since both the acromioclavicular and sternoclavicular joints share the clavicle as a bone, their movements are closely connected. The primary goal of the AC joint is to increase the range of motion (ROM) inside the pectoral girdle, specifically from the point where the sternoclavicular joint gets to its own maximal RoM.
- Retraction and protraction
- The entire angular range is elevated by 15° in the depression.
- (Total motion range: 30°) Rotation from the middle to the outside
Conversely, the acromion moves in a sagittal plane, elevating and depressing. In contrast with depression, which has to be limited by contact between the inferior surface of the clavicle and the coracoid process of the scapula, elevation remains by tension in both reaches of the coracoclavicular ligament.
The ability to fully elevate the flexed arm makes it essential for coordinating shoulder motions with pectoral girdle movements. The coracoclavicular ligament limits mobility in both directions.
The acromioclavicular joint’s capsular pattern suggests pain at extreme ranges of movement, particularly when the arm is fully extended and horizontally adducted. Biaxial auxiliary movements, as well as protraction-retraction and elevation-depression of the clavicle’s lateral end, are made possible by the joint.
Variation
The size and shape of the joint varied significantly among the 100 shoulders connected to US veterans, according to an X-ray study. The articular surfaces differed significantly in size and form. Their separation is provided in certain individuals by a meniscus that is attached to the superior acromioclavicular ligament.
This meniscus can resemble a disk that divides the joint in half or a fibrocartilage blade that juts out nearly halfway into the joint. In some joints, the joint is simply a fibrous tissue pad attached to the outside of the clavicle; there is no articular cavity present.
Clinical significance
Injury a separated shoulder
Dislocation, referred to as shoulder separation or AC separation, is one of the most common harms to the AC joint. This should not be confused with “shoulder dislocation,” also known as a glenohumeral joint dislocation.
People who swim, ride horses, mountain bike, bike, snow ski, or skateboard should be aware of the possibility of acromioclavicular joint dislocation. In contact sports like ice hockey, football, rugby, Judo, and Aussie rules, it is very prevalent. Often referred to as a FOOSH (Fall On Outstretched Hand) injury, a fall onto the apex of the shoulder is the most common mechanism of harm. The grade is determined by the amount that the acromion separates from the clavicle when weight is placed on the arm.
Grade I is defined by a considerable amount of joint dislocation and a heavily strained or partially torn AC ligament. The standard spacing is 4 mm. Complete AC joint tears, partial coracoclavicular ligament disruptions, and partial dislocations of the AC joint are classified as grade II injuries. The AC gap is greater than 5 mm.
Despite the possibility that they will need physical treatment, grades I and II never need surgery and recover on their own. In plain film, the superior aspect of the acromion will be positioned over the inferior side of the clavicle. A coracoclavicular ligament disruption and joint capsule tears, to variable degrees depending on the severity of the AC joint disruption, can also be seen on an MRI scan, which can be used to evaluate this. The joint will be quite sore and swollen upon examination. Around 16 to 20 weeks after the separation, shoulder function should return to normal. Nevertheless, there will be a noticeable lump and other anatomic abnormalities in the shoulder due to the clavicle dislocation.
Grades IV through VI are collarbone displacement issues on a “standard” dislocation that almost always requires surgery. Dynamic ultrasound is crucial for the diagnosis of small (grade I) dislocations since they can appear as normal joints in static images. When searching for low-grade injuries, a damaged ligament might be used to increase diagnostic confidence as it heals.
Osteoarthritis
Osteoarthritis is common in the acromioclavicular joint. As a degenerative disorder that often coexists with subacromial impingement, it can be pushed on by a prior injury (secondary osteoarthritis) or develop throughout time.
FAQs
Which two bones make up the joint between the acromioclavicle?
The clavicle, or collar bone, and the acromion, or shoulder cap, establish up the acromioclavicular joint.
What are the AC joint’s four bands?
These structures prevent the clavicle from rotating posteriorly and support vertical stability at low displacement levels. Commonly known as capsular thickenings or AC ligaments, these four structures are the superior, anterior, inferior, and posterior ligaments.
Which three ligaments are there in the acromioclavicular joint?
The acromion and lateral clavicle are separated by the acromioclavicular ligament, which runs horizontally.
The conoid ligament covers vertically from the scapula’s coracoid process to the clavicle’s conoid tubercle.
The trapezoid ligament connects the clavicle’s trapezoid line to the scapula’s coracoid process.
Which is the acromioclavicular joint’s structural type?
The AC joint can glide only in normal physiological circumstances given that it is a plane-type synovial joint. It provides the scapula with an extra range of motion and facilitates arm movements like shoulder abduction and flexion since it connects the scapula to the thorax.
The acromioclavicular joint is also known by what name?
Anatomically, the acromioclavicular joint (AC joint) is located in the upper part of the shoulder. This is where the acromion, the component of the scapula which creates up the shoulder’s highest point, joins the clavicle. This synovial joint is planar.
How does one define type 4 acromioclavicular joint?
When the clavicle is substantially displaced posteriorly, a grade 4 AC separation happens. The term “significant” posterior displacement describes it. Since the definition of grade separation is based solely on the clinician’s judgment, it lacks any measurable distance.
What is the AC joint’s primary stabilizer?
The AC joint is exposed through an incision executed across the upper part of the shoulder, and any diseased tissue is excised. The coracoid process is recognized during tissue analysis. The collarbone decreases by injecting a graft through a hole depressed into the clavicle, above the coracoid process.
What does an AC joint’s Type 3 separation mean?
There is no tear to the coracoclavicular ligaments, however, the acromioclavicular ligament is entirely ripped—grade III: A total joint dissociation. The acromioclavicular and coracoclavicular ligaments are torn, as is the capsule surrounding the joint.
What role does the acromioclavicular joint play primarily?
One of the main functions of the joint in raising the arm is to allow the scapula to continue rotating laterally after about 100 degrees of abduction, at which point the sternoclavicular joint ligaments limit the range of motion of the sternoclavicle.
Which muscles are connected to the AC joint?
The deltoid, trapezius, and pectoralis major are also essential clavicle attachments. The trapezius muscle connects to the clavicle’s posterior region, and the deltoid muscle inserts into its anterior region. The anterior surface of the medial two-thirds receives the pectoralis major insert.
Reference
- Tadvi, D. (2023, December 13). Acromioclavicular Joint – Anatomy, Structure, Function. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/acromioclavicular-joint/
- Wong, M., & Kiel, J. (2023, July 24). Anatomy, Shoulder and Upper Limb, Acromioclavicular Joint. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499858/
- Wikipedia contributors. (2024b, August 17). Acromioclavicular joint. Wikipedia. https://en.wikipedia.org/wiki/Acromioclavicular_joint
- https://www.physio-pedia.com/Acromioclavicular_Joint