Abnormal Gait
Introduction
Abnormal gait, more commonly known as a walking abnormality, happens whenever someone is unable to walk normally. An accident, underlying medical issues, or anomalies in the legs and feet could be reasons for this.
Walking appears to be a straightforward action. However, the body’s multiple systems, such as strength, coordination, and sensation, work together to allow a person to walk with a normal gait.
When one or more of these interconnected systems fails to function properly, it might cause an irregular gait or walking pattern.
What is Gait?
Gait refers to the pattern in which you walk. Walking requires muscle balance and coordination. Trauma or underlying health issues can result in an irregular gait. You may notice an irregular stride if you drag your toes, take large steps, or feel off balance while walking. While some gait disorders fade entirely on their own, several need persistent medical attention.
What is Abnormal Gait?
An abnormal gait is a visible variation in our normal walking rhythm. Each person has a natural walking style that is unique to them. However, various accidents and medical disorders can alter our normal walking rhythm. Anything that affects our brain, spinal cord, legs, or feet can alter our walking patterns.
An abnormal gait could be caused by any of these variables such as
- Disease
- Hereditary variables
- Trauma
- Deformities of the legs or feet
A few typical instances of an abnormal gait are:
- Limping.
- Dragging your toes.
- Shuffling your feet.
- Short steps.
- Difficulty bearing your body’s weight.
- Having trouble coordinating.
An abnormal gait is also known as ambulatory dysfunction. In certain cases, irregularities in gait resolve on their own. In other situations, an abnormal gait might not go away. Physical therapy can help in both situations by enhancing a person’s gait and easing any unpleasant symptoms.
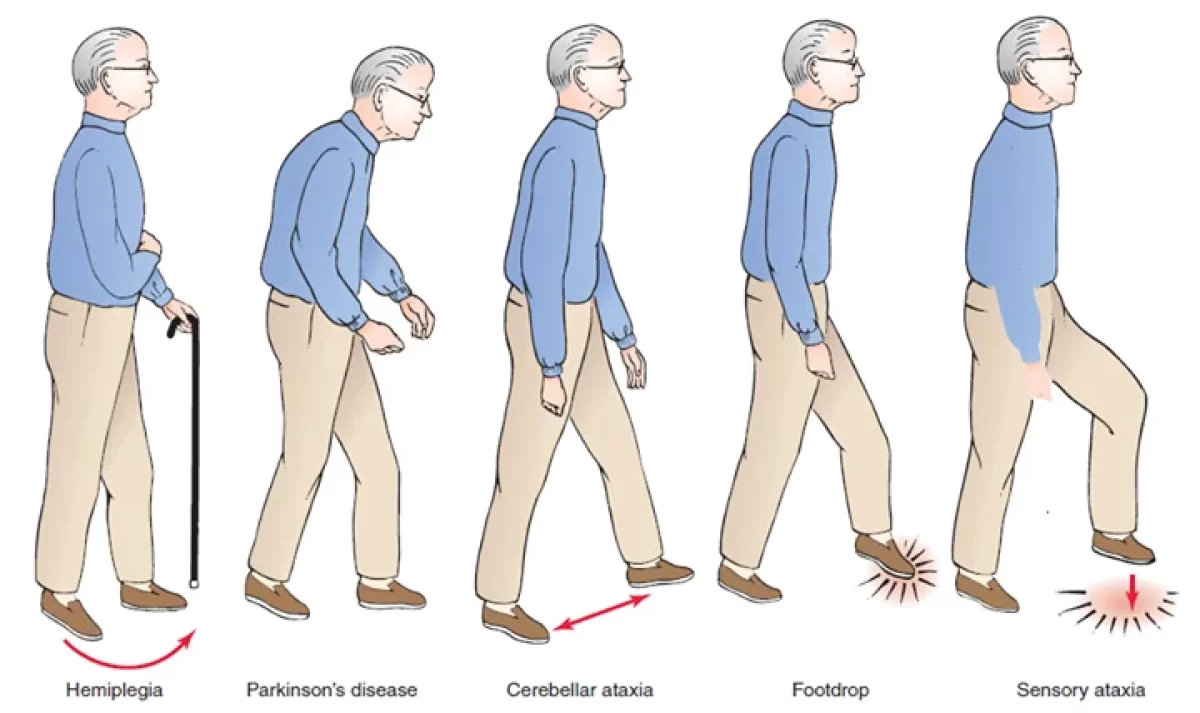
Types of Abnormal Gait
While there are many various kinds of irregularities in gait, the following are the most prevalent:
- Antalgic gait: The primary occurrence of antalgic gait is pain. It’s the most prevalent kind of irregular gait. You become limp as a result (avoid using your affected leg or foot when stepping).
- Propulsive gait (also known as Parkinson’s disease gait): Individuals with Parkinson’s or Parkinson’s disease are affected by this type of walking. A stiff, squatted posture, together with a forward-bending head and neck, are variables of a propulsive gait. To keep your center of gravity stable, you often take quick, short steps (festinating gait).
- Scissors gait: The way your knees and thighs strike or cross one other while you walk gives the impression that you are cutting paper. You might move slowly and in little steps. Those who have been diagnosed with spastic cerebral palsy typically exhibit this walk pattern.
- Hemiplegic gait: Walking with one rigid leg is the result of a spastic gait, also known as hemiplegic gait. That leg drags or swings in a semicircular pattern as you lift it to walk (circumduction). People with multiple sclerosis, cerebral palsy, or hemiplegia frequently have this kind of walk.
- Steppage gait (neuropathic gait): This kind of gait results in a high step, where your leg is raised above the typical level by elevating your hip. When your foot falls, it could look unsteady. When you walk, your toes often point downward and scratch the earth. Steppage gait can be caused by muscle atrophy or damage to the peroneal nerve (such as from spinal stenosis or a herniated disc).
- Waddling gait: A waddling gait is an excessively upper-body-moving walk that appears to be a duck. Hip dislocation or progressive muscular degeneration that develops gradually from birth can be the cause of waddling.
- Crouching gait: When walking, a crouching gait can be described by the flexion of the hips, knees, and ankles. Walking can sometimes give the impression that you are going to stoop over. You might feel your toes drag. Having cerebral palsy is typical to cause this kind of gait.
- Ataxic gait: Cerebellar atrophy is the cause of this kind of gait. It results in crooked steps that impair your ability to walk heel to toe in a straight path. An ataxic gait may make you feel shaky.
- Shuffling gait: Walking with a shuffling gait involves not taking your feet off the ground entirely. It makes your feet feel heavy. If you have an injury that keeps your feet from rising off the ground when you walk, or if you feel unbalanced, you might shuffle.
- Lurching gait: Individuals with paralysis or weakening of the gluteus medius (the muscles that surround your hips and butt) sometimes have a lurching stride. It results in a lengthy, sluggish gait. You could move your upper body to the front or back to lessen the amount of weight bearing on the affected leg.
How frequent is Abnormal Gait?
Gait problems become more common as people age. Approximately 15% of people have developed an uneven gait by the time they are 60 years old. despite this, almost 80% of people over 85 have an abnormal gait. Children are less likely to develop a gait irregularity unless they have a medical condition or are injured.
What causes Abnormal Gait?
Gait abnormalities are irregular walking patterns that can be caused by a variety of factors, including injury, pain, an inner ear (balance) impairment, or nerve damage. There are numerous probable causes and contributing factors for gait abnormalities. The most common causes are:
- Joint pain.
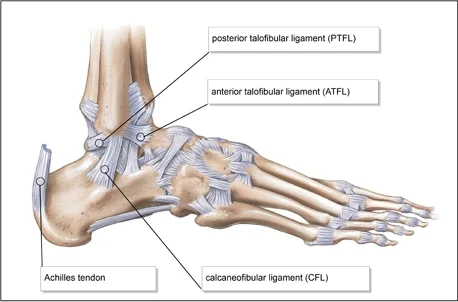
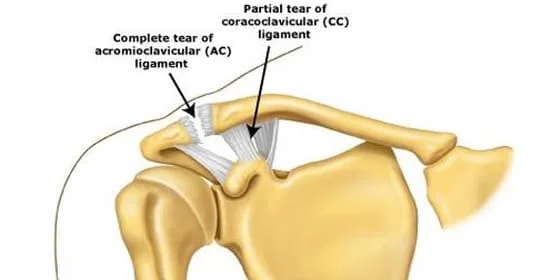
- A painful injury like a bone fracture or sprain.
- Foot issues may include sores, calluses, ingrown toenails, warts, and corns.
- Shoes that do not fit well.
- Inner ear problems.
- Nerve injury.
- Vision issues.
The following are some of the underlying health issues that may induce gait abnormalities:
- Parkinson’s disease (also known as parkinsonism).
- Multiple Sclerosis.
- Stroke.
- Arthritis.
- Cerebral palsy.
- Hemiplegia.
- Spinal stenosis and herniated disk.
Some irregular gaits have multiple causes.
What are the symptoms of Abnormal Gait?
The signs and symptoms of gait irregularities differ depending on the type of abnormality being experienced. Among the symptoms that are most frequently experienced are:
- Dragging or shuffling your steps.
- Feeling unbalanced while walking.
- Stiff joints or muscles in your legs and hips.
- Swaying from side to side with each step (waddle).
- Walking with your head and neck bent to the ground.
- Take higher-than-normal steps and drop your feet with each one.
- Take little steps.
- Walking causes pain.
What are the risk factors for Abnormal Gait?
- If you are over 60, you may have an increased risk of having gait problems.
- Have a condition that impairs your movement, joints, bones, muscles, brain, or spine.
- Have to suffer an injury.
What are the complications of Abnormal Gait?
The complications of gait disorders may include:
- Increased danger of falling or being injured.
- Muscular weakness.
- Sudden inability to walk.
- Pain.
- Reduced capacity for preserving independence.
How is Abnormal Gait diagnosed?
During a physical exam, healthcare providers can discover gait problems. They will take a comprehensive medical history, including:
- Evaluate your muscular strength, tone, and coordination.
- Check the length of your legs (for example, prosthetic hips might create varying leg lengths).
- Examine your eyesight and blood pressure.
- Examine your cervical and spine.
- Check your balance.
- Evaluate the walking joints’ range of motion.
A healthcare physician may do a variety of tests to learn more about the sort of gait impairment you have and what causes it. Imaging examinations, such as X-rays, and laboratory tests may be suggested.
How is Abnormal Gait treated?
Treatment for gait irregularities differs depending on the kind of gait and its etiology. Treatment options may include:
- Medications are used to treat underlying illnesses such as arthritis, Parkinson’s disease, and multiple sclerosis.
- Resting if you are injured.
- Physical treatment and strength exercises.
- Surgery, including hip and knee replacements.
- Using assistive mobility equipment such as a cane or walker.
- Adjusting footwear (wearing shoe lifts) or applying splints or braces.
If you have an abnormal gait, your healthcare practitioner will advise tips to prevent falls and accidents.
What part does physical therapy play in the case of Abnormal Gait?
Physical therapy is essential for controlling abnormal gaits and improving mobility. It includes a customized protocol of exercises and strategies meant to:
Goals of physical therapy
Increase muscle strength.
Increase flexibility.
Improve your balance and coordination.
Common physical treatment techniques for abnormal gait are:
- Strength training focuses on the muscles involved in walking and balance, which can help improve gait stability. Resistance bands, weight, or bodyweight exercises can help to improve the muscles that control gait.
- Stretching exercises may enable you to gain greater flexibility and release stiff muscles. Stretching tight muscles can increase the range of motion and decrease stiffness.
- Balance exercises can help people retain their balance and avoid falls. Standing on one leg, walking in tandem, and using a balancing board can all help you improve your balance. Gait training can help people learn to better coordinate their movements.
- Physical therapists can teach people how to use assistive devices effectively, such as canes or walkers.
Physical therapists may educate patients on ideal walking skills and support gadgets. The physiotherapy treatment plan will be designed for abnormal gait. For example, individuals with Parkinson’s disease may focus on exercises to enhance balance and coordination, whereas stroke patients may focus on strengthening afflicted muscles and restoring gait symmetry.
Are there any side effects of the treatment?
Before starting therapy, discuss the potential side effects with your healthcare professional. You may have discomfort, edema, or scars following surgery. You may also have adverse effects that are specific to the medication prescribed by your practitioner.
Prognosis
- Certain changes in your gait, particularly after an injury, are transitory and disappear as your body heals. Some people might need constant care for the remaining period of their life.
- The primary goal of the program is fall prevention. You run a higher risk of injury if your gait is abnormal. Your healthcare provider will offer you tips on how to reduce your risk of injury if you have an irregular gait.
- A cane or walker are example of aided mobility equipment that many individuals find useful. These tools help you become more adept at solo navigation. They may also boost your confidence if you struggle to remain upright on your feet by themselves.
- See your doctor, occupational therapist, or care team about at-home options if you struggle to accomplish everyday tasks because of a mobility-impairing condition.
Is it possible to prevent Abnormal Gait?
Abnormalities in gait resulting from underlying medical conditions cannot be prevented. There are various strategies to lower your danger of getting hurt:
- Using safety gear whether participating in sports or doing your job.
- Paying attention to your body, stopping activities, or taking pauses when you start to feel sore.
- Relaxing following an injury to avoid causing more harm or worsening the injury
- Utilizing appropriate form, building muscle, and improving flexibility to prepare for demanding exercises.
- Getting your vision examined periodically.
Summary
Gait abnormalities are prevalent and worsen as you age. Some gait irregularities are caused by an underlying health problem that can be treated to improve or resolve. Others may need lifetime care. Additional aches and pains associated with their walking pattern may be experienced by someone with an unstable gait.
Some reasons for aberrant gait are temporary and easily treated, but others might last a lifetime. If you have a gait irregularity, you may be more likely to have an injury or fall. Take precautions and seek counsel from a healthcare provider. Physical therapy and other therapies can assist to improve or cure an abnormal gait. People should seek medical advice and treatment as needed to manage their medical disorders.
FAQs
What defines an abnormal gait?
Your walking pattern is called your gait. An abnormal gait may also be caused by a trauma or underlying medical condition. If you feel unstable, drag your toes, or take huge steps when walking, you may have an abnormal gait.
What is considered a normal gait?
Due to improved stability and limb length, mature gait features reciprocal arm-swing and heel striking with increased velocity, cadence, step length, single-limb stance time, and the ratio of pelvic span should widen your ankles when you have both feet on the flat surface.
What is meant by the phrase “walking gait”?
One of the most basic aspects of human mobility is gait or the way one walks or runs. Variations in gait can point to underlying health issues in several medical specialties. Any divergence from a person’s regular gait or way of walking is referred to as a gait disturbance.
How are gait abnormalities treated?
Your doctor can create a plan to treat your gait problems once they have determined the cause of it. Numerous gait abnormalities can be corrected with drugs or surgery.
What are the different types of gait?
Spastic gait.
scissors gait.
Steppage gait.
Waddling gait.
Propulsion gait.
References:
- Patel, D. (2023, December 13). Abnormal Gait – Types, Symptoms, Treatment, Exercise – Mobile. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/abnormal-gait/
- Gait Disorders and Abnormalities. (2024, May 2). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21092-gait-disorders
- Gait Abnormalities. (n.d.). Stanford Medicine 25. https://stanfordmedicine25.stanford.edu/the25/gait.html
- Fletcher, J. (2017, December 31). What is abnormal gait? https://www.medicalnewstoday.com/articles/320481