Abducens Nerve
Introduction
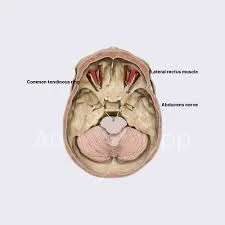
The abducens nerve, also known as the abducent nerve, controls the movement of the lateral rectus muscle, allowing your eye to rotate away from the centre of your body and look left or right. The 6th cranial nerve (CN VI) functions as the abducens. This nerve only has a motor function and not a sensory function.
According to categorising, the abducens nerve is considered extraocular, or “outside of the eye.” It moves the muscles surrounding the eyeball rather than the actual eye, just like the oculomotor nerve and the trochlear nerve.
Anatomical Course of Abducens Nerve
The abducens nerve emerges from the abducens nucleus in the pons of the brainstem. It exits the brainstem where the medulla and pons meet.
It then enters the subarachnoid space, piercing the dura mater and travelling through Dorello’s canal.
The abducens nerve leaves Dorello’s canal at the tip of the petrous temporal bone and enters the cavernous sinus, which is a dural venous sinus. It passes through the cavernous sinus and into the bony orbit via the superior orbital fissure.
Within the bony orbit, the abducens nerve innervates the lateral rectus muscle.
Embryology
The abducens nerve develops embryologically from derivatives of the somatic efferent column of the embryonic pons’ basal plates.
Muscles
The abducens nerve innervates the parallel lateral rectus muscle and partially the contralateral medial rectus muscle (at the nucleus, via the medial longitudinal fasciculus).
Function of Abducens nerve
The abducens nerve is purely a motor nerve, with no sensory function. The extraocular muscle of the eye that regulates the abduction of the eyes on the same (ipsilateral) side is innervated by it. This muscle is the lateral rectus.
The abducens nerve is also involved in the contralateral rectus muscle’s innervation via the longitudinal fasciculus, allowing both eyes to move laterally in a coordinated manner.
The Abducens nerve palsy
The Abducens nerve palsy affects the lateral rectus muscle, which impairs eye abduction. When the patient looks straight ahead, the eye may become slightly adducted. The palsy may be caused by a nerve infarction, Wernicke encephalopathy, trauma, infection, or increased intracranial pressure, or it could be idiopathic. To determine the cause, an MRI is required, as well as a lumbar puncture and vasculitis evaluation.
Causes of Abducens nerve
The abducens nerve extends further through the skull than any other cranial nerve. This makes it vulnerable to injury at several points. Damage to this nerve is known as abducens nerve palsy or sixth cranial nerve palsy.
Abducens injury is frequently the result of downward stress on the brainstem. Other causes are:
- Trauma
- Aneurysm
- Ischemia (lack of blood flow)
- Infection
- Inflammation resulting from an injury or illness
- Stroke
- Metabolic disease (also known as Wernicke disease)
- Demyelinating lesions.
- Carcinomatous meningitis.
- Basal skull fracture
- Damage to the orbit (eye socket).
- Surgery and other medical procedures can cause damage.
- particularly involving the cavernous sinus.
Poor blood sugar control in diabetics, as well as certain cavernous sinus problems, are major risk factors for abducens nerve palsy. (fortunately, nerves other than the abducens are likely to be affected by cavernous sinus issues and diabetic neuropathy.)
In many cases, possibly up to 30%, the cause is never determined.
Symptoms
The symptoms of 6th cranial nerve palsy include binocular horizontal diplopia when looking to the side of the paretic eye. Because the medial rectus muscle’s tonic action is unopposed, the eye is slightly adducted when the patient looks directly ahead. The eye abducts slowly, and even when abducted fully, the lateral sclera is exposed. With complete paralysis, the eye cannot move beyond the midline.
Palsy caused by a cavernous sinus lesion can cause severe headaches, chemosis (conjunctival edoema), anaesthesia in the distribution of the 1st and 2nd divisions of the 5th cranial nerve, and paralysis of the 3rd, 4th, and 6th branches. Both sides may be affected, albeit unevenly.
Assessment
The abducens nerve is examined alongside the oculomotor and trochlear nerves by testing eye movements. The patient is told to keep their head still and follow a point with their eyes—usually the tip of a pen. The target is moved in a ‘H-shape’, and the patient is asked to report any blurred vision or diplopia (double vision).
Treatment
A person should consult a specialist to determine the underlying cause of the abducens nerve palsy. For example, to rule out a central cause, such as a brain mass or stroke. The treatment and management of abducens nerve palsy differs for children and adults.
Treatment for Children
In children, treatment focuses on retraining the eye to allow proper movement. That can be carried out in a variety of methods, which include:
- Patching one eye at a time and periodically alternating helps prevent a “lazy eye” on the unaffected side.
- Prism therapy can prevent double vision.
- Botox injections
- If the other treatments fail, surgery
Treatment in adults
The most common first-line treatment for abducens nerve palsy in adults is to wait and see. Most cases resolve themselves.
When that does not happen, the treatment is determined by the cause of the palsy. Treatment can include:
Steroids to reduce inflammation.
Surgery or a lumbar puncture to alleviate pressure
treatments are similar to those for children, except for alternate patching.
Summary
The abducens nerve, also known as the abducent nerve, controls the movement of the lateral rectus muscle, allowing the eye to rotate away from the centre of the body and look left or right. It is classified as an extraocular nerve and has a motor function, not a sensory function. The abducens nerve innervates the parallel lateral rectus muscle and partially the contralateral medial rectus muscle.
Abducens nerve palsy impacts the lateral rectus muscle, which limits eye abduction. It may be caused by nerve infarction, Wernicke encephalopathy, trauma, infection, or increased intracranial pressure. Damage to the nerve is known as abducens nerve palsy or sixth cranial nerve palsy.
Causes of abducens nerve palsy include downward stress on the brainstem, trauma, aneurysm, ischemia, infection, inflammation, stroke, metabolic disease, demyelinating lesions, carcinomatous meningitis, basal skull fracture, or damage to the orbit. Poor blood sugar control in diabetics and certain cavernous sinus problems are major risk factors for abducens nerve palsy.
The 6th cranial nerve palsy shows as anesthesia in the distribution of the 1st and 2nd divisions of the 5th cranial nerve, paralysis of the 3rd, 4th, and 6th branches, chemosis, headaches, and binocular horizontal diplopia when looking to the side of the paretic eye.
Treatment for abducens nerve palsy varies for children and adults. In children, treatment focuses on retraining the eye to allow proper movement, while in adults, the most common first-line treatment is waiting and seeing.
FAQs
What is another term for the abducens nerve?
Cranial nerve six (CN VI), also known as the abducens nerve, is one of the nerves that control the eye’s extraocular motor functions, alongside the oculomotor nerve (CN III) and the trochlear nerve (CN IV).
Which muscle is controlled by the abducens nerve?
The lateral rectus muscle, one of the extraocular muscles in charge of outward gaze, is moved by the abducens nerve, also referred to as the sixth cranial nerve, cranial nerve VI, or simply CN VI. This nerve is present in humans and other animals. It’s a somatic efferent nerve.
What causes injury to the abducens nerve?
Potential causes include:
Injury (particularly if a skull fracture exists)
Stroke.
Infection (e.g., Lyme disease or virus)
Brain tumour.
Nerve inflammation, such as that caused by a vaccine.
Multiple Sclerosis.
Increased pressure within the brain (for example, from meningitis)
What exactly causes the abducens nerve to be weak?
Patients with abducens nerve palsy frequently exhibit binocular horizontal diplopia, which is double vision when viewing objects side by side. This is due to a significant weakness in the ipsilateral lateral rectus muscle, which prevents abduction on the affected side.
What is unique about the abducens nerve?
The abducens nerve, also known as the abducent nerve, controls the movement of the lateral rectus muscle, allowing your eye to rotate away from the centre of your body and look left or right.
References:
- Nguyen, V., Reddy, V., & Varacallo, M. (2022, November 21). Neuroanatomy, Cranial Nerve 6 (Abducens). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430711/
- The Abducens Nerve (CN VI) – Course – Motor – TeachMeAnatomy. (2019, March 13). TeachMeAnatomy. https://teachmeanatomy.info/head/cranial-nerves/abducens-nerve/
- Abducens Nerve. (n.d.). Physiopedia. https://www.physio-pedia.com/Abducens_Nerve
- Dellwo, A. (2023, October 16). The Anatomy of the Abducens Nerve. Verywell Health. https://www.verywellhealth.com/abducens-nerve-anatomy-4783613
- Rubin, M. (2024, March 18). Sixth Cranial Nerve (Abducens Nerve) Palsy. MSD Manual Consumer Version. https://www.msdmanuals.com/en-in/home/brain,-spinal-cord,-and-nerve-disorders/cranial-nerve-disorders/sixth-cranial-nerve-abducens-nerve-palsy


One Comment