Autosomal Recessive Cerebellar Ataxia
Introduction:
The disorder known as autosomal recessive cerebellar ataxia type 1 (ARCA1) is characterised by developing mobility issues. Early to mid-adulthood is when the disorder’s signs and symptoms initially manifest. Dysarthria, a speech disability, ataxia, a balance and coordination problem, or both are among the disorder’s early signs. Additionally, they could struggle with movements that require them to judge scale or distance (dysmetria).
Dizziness, or unpredictable eye motions, and inability to use the eyes to monitor the movement of objects are further signs of ARCA1. Slowly worsening mobility issues frequently necessitate using a wheelchair, cane, or walker.
Alternative Terms for This Illness:
- ARCA1
- Autosomal recessive spinocerebellar ataxia
- Recessive ataxia of Beauce
Types:
Phenotypes are taken into account while classifying autosomal recessive ataxias.
Ataxias come in various forms:
- Congenital ataxias (developmental disorders)
- ataxias with metabolic disorders
- ataxias with a DNA repair defect
- degenerative ataxias
- ataxia associated with other features.
Cause:
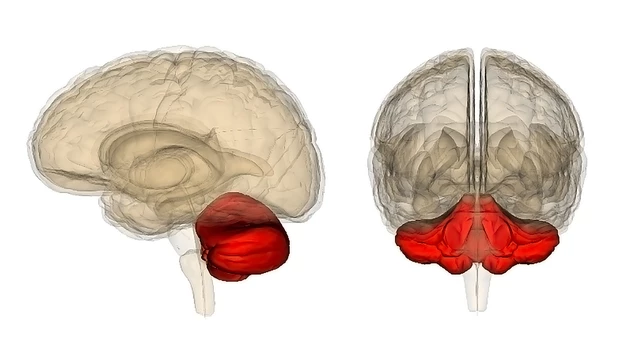
The ARCA1 gets passed by a mutation in the SYNE1 gene, which is required for the cerebellum’s Purkinje cells to synthesise the Syne-1 protein. Normal Purkinje cell functions are disrupted a,nd its ability to communicate with cerebellar neurones is compromised by deformed Syne-1 protein. It is yet unknown how the loss of cerebellar cells that contribute to ARCA1 is caused by compromised sysyn-1oteins.
Symptoms:
The majority of autosomal recessive cerebellar ataxia cases start early, typically around age 20. This kind of ataxia is characterised by several common symptoms, such as:
- Numerous falls as a result of inadequate balance.
- Poor hand-eye coordination.
- Kinetic or postural tremor of the trunk or limbs.
- dysarthria
- dysphasia
- vertigo
- diplopia
- lower extremity tendon reflexes
- dysmetria
- Minor abnormalities in ocular saccades
- attention defects
- impaired verbal working memory and visuospatial skills
- Normal life expectancy
Most often, autosomal recessive ataxias are associated with a loss of proprioception and vibration perception. Compared to autosomal dominant ataxias, autosomal recessive ataxias are more likely to have areflexia.
They also tend to be more involved in areas other than the neurological system. One possible cause of autosomal recessive cerebellar ataxia has been identified as mutations in the mitochondrial DNA polymerase (POLG) subunit.
Frequency:
Over 100 individuals have received an ARCA1 diagnosis. Initially identified in people from the Beauce and Bas-Saint-Laurent regions of Quebec, Canada, this condition has since spread to populations all over the world.
Diagnosis:
People who exhibit the early signs of recessive autosomal cerebellar ataxia and have an age of onset between the late teens and the late forties are diagnosed clinically. The tests mentioned below are conducted:
- Cerebellar atrophy is detected via MRI brain scanning.
- SYNE-1 sequence analysis using molecular genetic testing.
- Polyneuropathy electrophysiologic investigations.
- Neurological analysis.
Treatment:
- Physical therapy improves muscle strength and balance.
- occupational therapy
- Treatment of abetalipoproteinemia is recommended because it may help avoid vitamin E deficiency (1000 mg/day for babies and more than 5,000 mg/day for adults).
- Coenzyme Q10 deficiency can be treated with CoQ10 supplementation (300–600 mg/day).
Prognosis:
Most often, oculomotor signals appear between the ages of two and four. The onset of telangiectasias occurs between the ages of 2 and 8. The child typically requires a wheelchair by the time they are ten years old. Autosomal recessive cerebellar ataxia patients often live into their 20s, while some have lived into their 40s or 50s.
FAQs
Autosomal recessive cerebellar ataxia: what is it?
An explanation. The condition known as autosomal recessive cerebellar ataxia type 1 (ARCA1) is characterised by progressive mobility issues caused by atrophy (loss) of nerve cells in the cerebellum, the area of the brain responsible for movement coordination. Early to mid-adulthood is when the disorder’s signs and symptoms initially manifest.
How long does a person with autosomal recessive cerebellar ataxia expect to live?
Autosomal recessive cerebellar ataxia patients often live into their 20s, while some have lived into their 40s or 50s.
Are there any symptoms of autosomal dominant cerebellar ataxia?
Common symptoms include slurred speech and a loss of coordination, which is frequently observed when walking. The spinal cord and cerebellum are the main organs affected by ADCA. Events of impaired consciousness are among the signs and symptoms.
Which three conditions are autosomal recessive?
Tay-Sachs disease
Sickle cell anemia and
cystic fibrosis
Which autosomal recessive ataxia is the most prevalent?
The disease known as Friedreich’s is rather frequent. About half of all cases of genetic ataxia are of this kind, making it the most prevalent autosomal recessive ataxia.
How can one determine whether it is autosomal recessive?
Autosomal recessive pedigrees are frequently referred to as “skipping” generations and typically exhibit fewer afflicted individuals than pedigrees containing dominant features. Therefore, the ability of unaffected individuals to have affected kids is the primary characteristic that sets autosomal recessive traits apart from dominantly inherited characteristics.
Referances
- Wikipedia contributors. (2023, August 28). Autosomal recessive cerebellar ataxia type 1. Wikipedia. https://en.wikipedia.org/wiki/Autosomal_recessive_cerebellar_ataxia_type_1
- MedlinePlus Genetics. (2015). Autosomal recessive cerebellar ataxia type 1. MedlinePlus Genetics. https://medlineplus.gov/download/genetics/condition/autosomal-recessive-cerebellar-ataxia-type-1.pdf