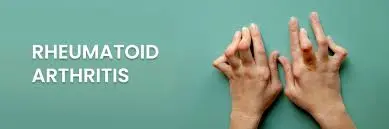
What Are the 4 Stages of Rheumatoid Arthritis
Introduction
One chronic autoimmune condition that typically impacts the bones and cartilage is rheumatoid arthritis (RA). It results in generalized inflammation. When RA occurs, the body’s immune system unintentionally targets the tissue lining the joints, known as the synovial membrane, resulting in stiffness, pain, and swelling. This inflammation can harm the joints over time, resulting in deformities and impaired function.
Multiple joints are typically affected simultaneously by rheumatoid arthritis, which frequently results in pain and inflammation throughout the body. This might result in deformity, chronic joint discomfort, and trouble walking.
The heart, lungs, eyes, and other systems throughout the body can all be affected by rheumatoid arthritis (RA), in addition to the joints.
“With rheumatoid arthritis (RA), the immune system gets confused and starts attacking the body’s healthy tissues, thinking they’re a threat.” This is in contrast to osteoarthritis.
Chronic Conditions:
A chronic disease, rheumatoid arthritis, can last for many years, possibly a lifetime.
The severity of symptoms can vary, with flare-ups (when the disease is more active) and remissions (when there are few or no symptoms).
Disorder of the System:
Blood arteries, nerves, the skin, eyes, lungs, and heart can all be affected by RA-related inflammation.
Autoimmune Conditions:
The main cause of rheumatoid arthritis is an immune system malfunction in which the body’s tissues are wrongly attacked by the immune system as though they were foreign intruders.
The immune system, which normally protects the body from external intruders like germs and viruses, wrongly targets itself.
The synovium is a healthy tissue found in the body.
Hormonal variables, environmental factors (such as smoking), and genetic predisposition are thought to be involved in this autoimmune response, while the exact reason is unclear.
Causes of RA
Rheumatoid arthritis (RA) has no established etiology, however, it is believed to be caused by a complicated interaction between a number of variables. It is a result of an association of environmental stimuli and an individual’s genetic composition rather than a single cause.
Genetic tendency:
HLA Genes: Some genes in the Human Leukocyte Antigen (HLA) complex, especially the HLA-DRB1 gene, have the strongest genetic association with RA.
Known as the “shared receptor,” some mutations of this gene are strongly linked to a higher chance of getting RA and perhaps more severe illness.
Other Genes: Although their combined influence is often less significant, a large number of other genes related to immune system function have also been discovered as possible risk factors in addition to HLA genes.
TRAF1/C5, PTPN22, STAT4, and several additional genes are among them.
Family History: Having a close relative with RA, such as a parent or sibling, increases a person’s risk of developing the condition and may suggest a hereditary component. Genetics alone is sufficient since if the first identical twin has RA, the other identical twin has a twelve to fifteen percent probability of developing it.
Environmental Aspects:
The chance of getting RA is greatly increased by smoking, especially heavy and prolonged smoking, especially in people with certain genetic markers like HLA-DR4. Additionally, it is linked to more severe illness and a worse prognosis.
Air pollution: It has been proposed that exposure to pollutants like dioxin and living next to a highway or in an urban area may be environmental factors that contribute to the development or severity of RA, potentially through interactions with genetic predispositions.
Pesticide Exposure: Research has indicated a connection between specific pesticide exposures and a higher risk of developing RA.
Hormonal Aspects:
Given that RA affects women two to three times as frequently as it does males, hormones may be involved.
Pregnancy may cause the condition to go into remission, and major hormonal changes during menopause or after childbirth may cause flare-ups.
The possible role of several hormones, such as prolactin, which increases inflammation, has been studied.
Additional Possible Elements:
Obesity: Being overweight or obese can exacerbate symptoms and is linked to an increased chance of getting RA.
Diet: More study is required, although some evidence points to a Mediterranean diet heavy in omega-3 fatty acids having a protective impact, whereas a diet high in red meat and Rheumatoid arthritis risk may be elevated by vitamin C and A deficiencies
Gut Microbiota: According to a study, the makeup of the bacteria in the gut may affect the immune system and contribute to autoimmune conditions like RA.
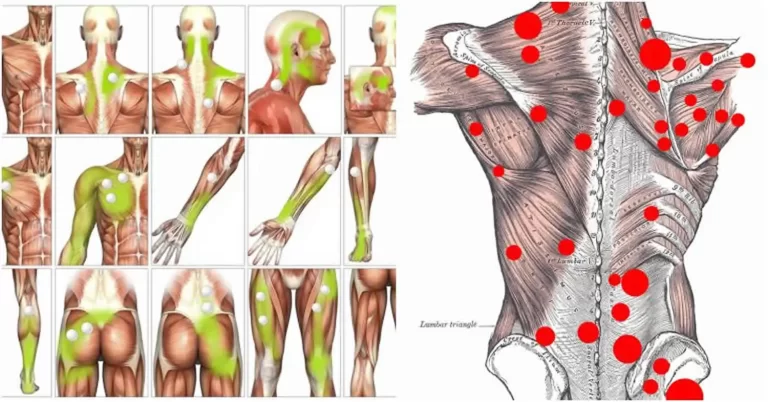
Symptoms of Rheumatoid Arthritis
Sore, stiff joints
You may feel pain and stiffness in multiple joints, often in your hands, wrists, or knees. This discomfort is usually more intense in the morning or after sitting still for a while, and it tends to last longer than half an hour.
Swollen and warm areas
“Your joints may become swollen, feel warm, and be sensitive or painful to touch.” These symptoms can come and go, or stick around during what’s known as a “flare.”
Constant fatigue
Even when you’re getting enough sleep, you could still feel worn out or fatigued.
General feeling of being unwell
Aside from joint discomfort, you might feel slightly feverish or just not like your usual self, almost like you’re coming down with something.
Pain on both sides of the body
RA often affects joints symmetrically. That means if one knee or wrist is inflamed, the same joint on the opposite side is likely to hurt too.
Limited range of motion
You might notice your joints aren’t moving as easily. Everyday tasks like gripping, stretching, or bending can become more difficult, especially during flare-ups.
Small bumps under the skin
Near the elbows or fingers. These are known as rheumatoid nodules.
Unexpected weight loss
Without changing your diet or activity level, you might start losing weight. This can happen because inflammation from RA affects your entire body.
Deformities
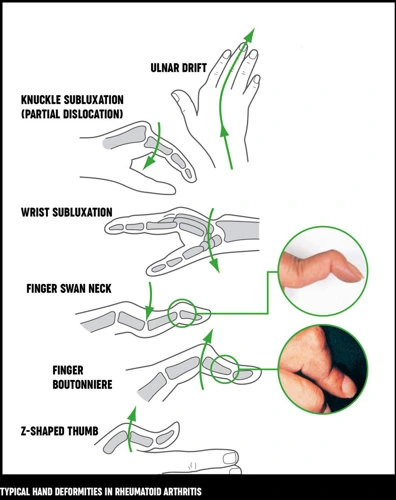
Deformity of the Swan Neck
The fingertip bends downward at the last joint (DIP), while the middle joint (PIP) bends upward more than usual, creating an abnormal positioning.
Why it occurs: The tendons that pull the finger become unbalanced, and the volar plate, which supports the finger joint, weakens.
Deformity of the Boutonnière
It appears as follows: The finger tip (DIP) bends up, and the middle joint (PIP) bends down.
Why it occurs: The tendon’s core portion on the rear of the finger becomes injured, making it unable to straighten the finger as it should.
Ulnar Drift, also known as Ulnar Deviation
What it looks like: Fingers wander away from the thumb and tilt toward the pinky side at the knuckles (MCP joints).
Why it occurs: Persistent inflammation weakens the tissues holding the joints together, as in rheumatoid arthritis.
Deformity of Z-Line (Z Thumb)
It appears like a “Z” because the thumb bends downward at the base (MCP joint), then back up at the tip (IP joint).
Hammer Toes
What it looks like: The toe’s tip (DIP) protrudes while the middle joint (PIP) bends downward.
What’s happening: The joints are being pulled into this strange form by the imbalanced muscles and tendons around the toe.
Claw Toes
What it looks like: The base of the toe (MTP joint) bulges while the middle (PIP) and tip (DIP) joints bend downward.
What’s happening: Usually caused by nerve or muscular problems that impair toe movement, it takes the form of a claw.
Subluxation or Dislocation of the MTP Joint
What it looks like: The toe curls and pops up, giving the appearance of a “cock-up.”
What’s happening: Chronic stress or inflammation causes the base of the toe (MTP) joint to fall out of alignment.
Pes Planus, or the flat foot
How it appears: The foot’s arch is either low or flat.
What’s happening: The arch cannot be adequately supported by weak or strained ligaments and tendons.
Importance of Knowing the Stages of RA
Understanding the normal phases enables patients to predict changes in their bodies throughout time. Better coping mechanisms and psychological preparedness are made possible by this.
Early Intervention: Patients are able to seek timely medical treatment when they recognize the early symptoms, which correspond to Stage 1. Early detection and therapy during the “window of opportunity” can minimize joint damage, considerably decrease the development of the disease, and in certain situations, even result in cure.
Self-Management That Works: Patients can adjust their self-care strategies, such as using heat or ice, exercising joint protection procedures, and striking a balance between activity and rest, by being aware of their present state.
Stages of Rheumatoid Arthritis
Stage 1: Early Stage of Rheumatoid Arthritis
What’s Happening Inside the Body:
In the early stage of RA, your immune system normally there to protect you from illness, mistakenly starts attacking your own body. It concentrates on the synovium, a small layer of tissue that covers your joints.
This attack causes the synovium to become inflamed (swollen and irritated). As this inflammation begins, it may not be obvious on the outside, but changes are starting to happen on the inside of your joints.
Common Symptoms to Watch For:
Joint Pain: A dull or aching pain in your joints, especially in smaller joints like your fingers, wrists, or toes.
Stiffness: Your joints may feel difficult to move or tight; this is frequently worse in the morning or after taking a nap.
Mild Swelling: You might see or feel a little puffiness around the affected joints.
At this point, you might not see any major damage or deformities in the joints, but the disease process has begun beneath the surface.
How It’s Diagnosed:
X-rays are used.
MRI (Magnetic Resonance Imaging) or ultrasound scans are more sensitive and can pick up early signs of inflammation, like swelling in the synovium or tiny amounts of fluid in the joint.
Blood tests may also show inflammation markers or autoantibodies that suggest RA is starting.
Stage 2: Moderate Stage Rheumatoid Arthritis (RA)
What’s Happening in the Body:
Your joints are becoming more inflamed at this time. I It’s not just affecting the soft tissue around the joints anymore — now it’s starting to damage the cartilage too.
When RA damages this cartilage, your bones can start to rub against each other, which makes movement painful and more difficult.
Symptoms You Might Notice
More Pain and Swelling: The joints may feel warmer, more tender, and look puffier than before.
Stiffness: particularly after a long period of sitting or in the morning. Now it might go on longer.
Everyday Tasks Become Harder: Things like opening jars, buttoning a shirt, or walking might start to feel more difficult.
How It’s Diagnosed:
Imaging Tests (like X-rays or MRIs): These might now show visible damage, such as:
Erosion of the bone near the joints.
Joint space reduces.
Lab Tests: Blood tests will likely still show high levels of inflammation, confirming that the disease is active.
Why This Stage Matters:
This is when real joint damage begins. If RA is not well controlled at this stage, the harm may be irreversible. For this reason, it’s crucial to:
Keep up with doctor visits
Take medications as prescribed
Consider lifestyle changes like diet, exercise, or physical therapy.
Stage 3: Severe Stage of Rheumatoid Arthritis
What’s Happening Inside the Body:
At this stage, the disease has progressed significantly. The immune system has been attacking the joints for a long time now. Earlier, it started with inflammation in the joint lining (called the synovium), then it damaged the cartilage, and now, the damage has gone even deeper.
The bones inside the joint are now being attacked and broken down.
The joint is no longer able to hold its normal shape and may become deformed or misaligned.
The surrounding muscles, tendons, and ligaments may also become weak or stretched.
This stage is more serious because the structure of the joint is permanently changed.
Symptoms You Might Notice:
Severe Joint Pain: The pain may be constant and can affect your ability to move or even rest comfortably.
Loss of Joint Function: You might not be able to bend, grip, or use your joints the way you used to. Daily activities like opening jars, writing, or walking might become difficult.
Visible Deformities: Fingers, wrists, or toes may begin to look crooked or twisted due to the joint being pushed out of alignment.
Weak Muscles: Because the joint isn’t being used as much, or because of the damage, the muscles around it may shrink or weaken.
How It’s Diagnosed:
X-rays, MRIs, or ultrasounds will now clearly show bone erosion (wearing away of bone), joint space narrowing, and deformities.
A doctor might also notice signs of joint instability, where the joint feels loose or wobbly.
Muscle weakness around the affected joints might be found during a physical exam.
Important Note: Even though the damage is more advanced at this stage, there are still treatments available that can help manage pain, protect remaining joint function, and improve quality of life.
Stage 4: End-Stage Rheumatoid Arthritis – What It Means
What’s Happening in the Body?
At this final stage of rheumatoid arthritis, the disease has caused severe damage to the joints. There may be severe degeneration of both the joint surfaces and the cushioning cartilage, leaving minimal structural support. In some cases, the bones in a joint might fuse, which makes the joint stiff and unable to move at all. This stage is often irreversible, meaning the damage has reached a point where it can’t be undone.
Symptoms You Might Experience
Severe, constant pain in the joints – even at rest.
Major loss of movement – joints may no longer bend, straighten, or move at all.
Swelling and stiffness will increase.
Joint abnormalities that are visible: fingers or other joints may seem malformed or twisted in strange ways.
Muscle weakness due to reduced use of the limbs.
Extreme fatigue and low energy, often from dealing with chronic pain.
Possible disability, making it difficult to do everyday activities like walking, dressing, or cooking.
What Does Diagnosis Look Like at This Stage?
Physicians usually use imaging tests like X-rays, MRIs, or ultrasounds to confirm end-stage RA. These pictures will display:
- Severe joint destruction
- Loss of joint space
- Possible joint fusion
- Signs of bone erosion
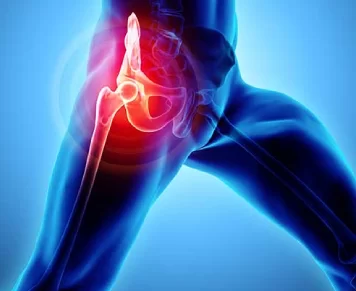
At this stage, many people require mobility aids like canes, walkers, or wheelchairs. In advanced cases, joint replacement procedures, such as total hip or knee arthroplasty, may be required to alleviate pain and regain functional mobility.
What Can Be Done?
Even though joint damage at this stage is permanent, there are still ways to improve quality of life, such as:
Pain management, including medications or nerve blocks.
Assistive devices to help with daily tasks.
Surgical interventions, such as arthroplasty or arthrodesis, may be considered depending on the extent of joint deterioration.
Support systems, such as home care or occupational therapy.
If you or someone you know is facing this stage of RA, it’s important to work closely with a rheumatologist, pain specialist, and physical therapist to create a care plan that focuses on comfort, mobility, and independence.
Risk Factors
Family history and genetics
Human leukocyte antigen (HLA) gene variants, particularly those involving the HLA-DR4 gene, put people at higher risk.
Family history: Your risks are much increased if you have a close relative with RA.
Women are two to three times more likely than men to have gender-related RA, most likely as a result of hormonal effects on the immune system.
Although aging RA may occur at any age, it often appears first between the ages of 30 and 60.
One of the biggest environmental risk factors for RA is smoking cigarettes, particularly for people who have a genetic link to the disease.
Being overweight
Particularly in women under 55, excess body fat elevates the risk of RA and causes inflammation in the body.
Exposures to the Environment
Mineral oils, asbestos, and silica dust—all of which are frequently found in specific occupations—can raise the risk of RA. Pesticide exposure and air pollution could also be factors.
Infections
Although this connection isn’t entirely established, some bacterial or viral infections may cause RA in those who are genetically susceptible.
Hormonal Elements
Hormone changes, such as those that occur during pregnancy or menopause, may have an impact on the development of RA.
Studies have shown different links between nursing and the use of oral contraceptives.
Nutrition and Digestive Health
Risk may be increased by diets heavy in processed foods, sweets, and red meat. Autoimmune diseases are believed to be prevented by a healthy gut microbiota, but an imbalance may make people susceptible.
Social and Economic Standing
A higher risk is associated with lower income and education levels, maybe as a result of increased exposure to risk factors like smoking or less access to healthcare.
Treatment of Rheumatoid Arthritis (RA) According to Its Stages
Stage 1: Early RA (Mild Symptoms)
Inflammation is beginning inside the joints, even though there may not be any joint injury yet.
Ibuprofen is one example of a non-steroidal anti-inflammatory medicine (NSAID), which is used to alleviate pain and swelling.
Corticosteroids at low doses can be used to rapidly reduce inflammation.
Methotrexate and other DMARDs (illness-modifying Anti-Rheumatic Drugs) are typically begun early to halt the course of the illness before damage is done.
Lifestyle modifications include healthful nutrition, regular low-impact activity, and giving up smoking.
Stage 2: Moderate RA (Inflammation Progresses)
Treatment: Keep taking DMARDs or modify them (for example, by switching to stronger ones or combining medications).
The introduction of biologic treatments is possible. These are specialized drugs that target certain immune system components, such as etanercept, adalimumab, or infliximab.
Start physiotherapy treatment, which can help you maintain your joint mobility and muscle strength
Pain management: For flare-ups, injections or temporary steroids may be used.
Stage 3: Severe RA (Joint Damage Begins)
Treatment options include JAK inhibitors like tofacitinib or baricitinib, or aggressive biologic therapy.
Combination therapy: Several of biologics and DMARDs may be used concurrently.
Short doses of corticosteroids for flare-ups.
Assistive devices: To protect joints, use braces, splints, or ergonomic gadgets.
Treatment options include JAK inhibitors like tofacitinib or baricitinib, or aggressive biologic therapy.
Combination therapy: many biologics and DMARDs may be used concurrently.
Short doses of corticosteroids for flare-ups.
Assistive devices: To protect joints, use braces, splints, or ergonomic gadgets.
Stage 4: End-Stage RA (Advanced Joint Destruction)
Joint replacement, tendon repair, or joint fusion surgery may be required.
Managing pain becomes the primary focus.
Continue physiotherapy treatment
ongoing prescription drugs to manage any remaining inflammation and stop any recurrence
Mental and emotional support: At this point, anxiety and depression are common.
FAQs
Are all four phases experienced by all people with RA?
Not always. Many people can delay or halt the course of their disease and may never reach the latter stage with early diagnosis and adequate therapy.
Is it possible to reverse the phases of RA?
Early therapy can stop or slow the course of joint injury, but damage from later stages cannot be undone.
At each stage, what part does therapy play?
Early stage: Drugs can reduce inflammation and stop harm.
Stages ranging from moderate to severe: medication, physical therapy, or surgery may be required.
End stage: Priorities include pain management, mobility support, and joint replacements if required.
How can I slow down RA’s progression?
Start therapy as soon as possible.
Continue taking your prescription drugs as directed.
Keep up a healthy way of living
Don’t smoke.
Attend your doctor’s visits on time.
Does RA have an impact on other body parts?
Systemic problems can result from RA’s effects on the skin, blood vessels, heart, lungs, and eyes.
References
- Rheumatoid arthritis – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
- & S. Z. K. (2023, June 13). Exercise Tutorial: Cross-Body Shoulder Stretch. Your House Fitness. https://www.yourhousefitness.com/blog/exercise-tutorial-cross-body-shoulder-stretch
- Barhum, L. (2023, December 1). Rheumatoid arthritis: From beginning symptoms to treatment. Verywell Health. https://www.verywellhealth.com/rheumatoid-arthritis-8404495
- Stasko, N. (2024, March 10). What are the 4 stages of rheumatoid arthritis? Harley Street Specialist Hospital. https://hssh.health/blog/what-are-the-4-stages-of-rheumatoid-arthritis/