Sensory Ataxia
A Sensory Ataxia: What is it?
Sensory Ataxia is a type of ataxia caused by the loss of proprioceptive input—the body’s ability to sense its position in space—due to damage in the sensory pathways, especially the dorsal columns of the spinal cord or peripheral nerves.
Whenever a patient obtains a positive Romberg’s sign, it demonstrates that their coordination is nearly constant and that they can move, which sets sensory ataxia apart from cerebellar ataxia. Still, it significantly deteriorates when the eyes are closed.
People who have sensory ataxia frequently exhibit Romberg’s sign and pseudoathetosis. When putting off their garments over their heads or closing their eyes during a shower, they usually complain of losing their balance in the dark.
Causes of Sensory Ataxia:
The circuits that carry position and movement data to the brain are interfered with in sensory ataxia. There are numerous causes of these disruptions, which can be broadly divided into several categories:
Diabetic neuropathy: Elevated blood sugar levels progressively damage peripheral nerves, impairing their ability to convey sensory data, especially proprioception and vibration perception, and causing problems with balance and walking. Ataxia and sensory loss can result from neuronal damage caused by elevated blood sugar levels.
Reduced sensory input can result from nerve degeneration caused by long-term alcohol abuse.
Certain vitamin deficiencies, like B12 (cobalamin), can result in sensory ataxia and nerve degeneration.
Guillain-Barré Syndrome (GBS) is an acute autoimmune condition that impairs motor and sensory function by attacking peripheral nerves.
The sensory track’s myelin sheath may sustain damage from multiple sclerosis (MS). This demyelination of sensory pathways impacts the transmission of sensory data from the spinal cord to the brain, resulting in ataxia and diminished proprioception.
Stroke: Sensory ataxia may result from a stroke that damages the areas of the brain in charge of processing sensory data.
Spinal Cord Disorders: By harming the dorsal columns of the spinal cord, tabes dorsalis, a late-stage syphilis symptom, results in sensory ataxia. In syringomyelia, a fluid-filled cyst forms inside the spinal cord, harming the dorsal columns and preventing sensory signals from passing through, which causes ataxia and a lack of sensation.
Infections:
- The bacteria Borrelia burgdorferi are responsible for Lyme disease, which affects the neurological system and results in sensory ataxia.
- HIV/AIDS: Direct viral impacts or treatment-related side effects may result in sensory neuropathy.
- Systemic Lupus Erythematosus (SLE) may impact the neurological system, leading to sensory impairment.
- Trauma: Ataxia can result from spinal cord injuries that interfere with sensory pathways.
- Peripheral Nerve Injury: Ataxia and impaired sensory input can result from trauma to the peripheral nerves.
Metabolic disorders
- Toxins build up and kill neurons in uremic neuropathy, a chronic renal disease syndrome that affects sensory function.
- A genetic disorder called Wilson’s Disease results in copper accumulation in several tissues, including the neurological system, which can lead to sensory ataxia.
Toxins
- Peripheral neuropathy and sensory ataxia can be caused by exposure to heavy metals like lead or mercury.
- Certain drugs can damage sensory circuits and cause neurotoxic side effects.
Sensory Ataxia Symptoms and Signs:
Coordination and Balance Issues
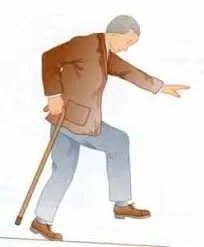
- Wide-based gait and trouble walking are signs of an irregular gait. The people may appear shaky or unsteady, especially if they are walking at night or with their eyes closed.
- Balance Issues: Having trouble staying balanced when standing or moving, particularly if proprioceptive perception is impaired.
Sensory disturbances
- Abnormal feelings include things like limb tingling or numbness.
- Sensation loss is the term used to describe a lessened feeling of touch, warmth, or vibration.
Impaired coordination
- Awkward Motions: Having trouble making exact motions, such as buttoning a blouse or picking up tiny objects. Awkward or careless actions might be seen.
- Difficulty with Fine Motor Skills
- Coordination Issues: Individuals who have poor proprioception may find it difficult to keep their balance and coordinate their motions.
Postural instability
- In the absence of visual guidance, proprioception issues include trouble determining the placement of limbs and body parts. It should be difficult to perform tasks like standing with your eyes closed if you have postural instability.
- Romberg Test Positive: This test has the patient stand with their eyes closed; proprioceptive dysfunction is indicated if they wobble or fall.
Dysmetria
- Incorrect Movement: When reaching for objects, a person who struggles to judge distance and range of motion may overshoot or undershoot.
Gait Abnormalities
- Misstepping, uneven steps, or a tendency to depart off course are characteristics of an ataxic, uncoordinated gait.
- Unsteady Gait: Having trouble walking and maintaining balance, particularly when there is little or no visual input (e.g., eyes closed).
Difficulty performing complex movements
- Coordination problems: Having trouble carrying out activities requiring complex or coordinated movements, such as playing an instrument or engaging in sports.
Associated Symptoms
- Muscle Weakness: Adjusting for decreased sensory input or disuse can lead to muscle weakness in certain situations.
- The object recognition issue: The inability to distinguish between objects only by touch is known as stereognosis.
- Depending on the underlying cause—diabetic neuropathy, nutritional deficiencies, or neurological issues—sensory ataxia symptoms and severity may be different. To diagnose sensory ataxia and identify its etiology, which will inform appropriate management and treatment, a comprehensive medical evaluation is necessary.
Types of Sensory Ataxia:
There are two types of sensory ataxia:
vestibular
proprioceptive.
Proprioceptive ataxia is a condition in which the body’s sense of joint position and movement is impaired. The opposite is true with vestibular ataxia, which is linked to inner ear and balance system issues.
Loss of proprioception, or the awareness of one’s own body’s position and movement, is a hallmark of proprioceptive sensory ataxia, which causes uncoordinated movements and balance issues.
Vertigo and unsteadiness are signs of vestibular sensory ataxia, which is caused by a malfunction in the vestibular system, which regulates balance and spatial orientation.
Impaired visual input processing leads to visual sensory ataxia, which impairs balance and coordination because it is difficult to correctly interpret visual signals.
Disruptions in the sense of touch result in tactile sensory ataxia, which makes it difficult to coordinate movements and maintain balance in the absence of appropriate tactile feedback.
Pathophysiology of Sensory Ataxia:
Sensory Pathways and Functions
The brain receives proprioceptive (position sensation), tactile (touch), and vibratory impulses from the peripheral nervous system through the fasciculus cuneatus and gracilis in the spinal cord’s dorsal columns. Despite being primarily involved in motor control, damage to the corticospinal tract can occasionally have an indirect impact on sensory perception. The brain’s parietal lobe contains an area called the somatosensory cortex, which is responsible for processing sensory data from the brainstem and spinal cord.
Mechanisms for Sensory Ataxia:
Sensory Route Disruption: The transmission of sensory information is hampered by injury or degeneration to sensory routes, such as the dorsal columns or peripheral nerves. Numerous circumstances may cause this disruption, such as:
- Reduced sensory input from the limbs and other parts of the body results from peripheral neuropathy, which is caused by damage to peripheral nerves (for instance, from diabetes, alcohol abuse, or vitamin deficiencies).
- The inability to perceive one’s posture and motion is known as proprioception. Loss of proprioceptive input, which prevents the brain from correctly interpreting limb positions and movements, is a common feature of sensory ataxia. Lack of this feedback puts coordination and balance at risk.
- Inadequate Sensory Integration: The brain integrates sensory data from various sources, including vision, proprioception, and vestibular input, to coordinate movements and preserve balance. Impaired balance and coordination might arise from delays in the sensory system that disrupt its integration.
- Compensatory Mechanisms: To preserve balance and coordination when faced with sensory impairments, humans may depend more on their other senses, like eyesight. Ataxia may become apparent, though, if compensatory mechanisms malfunction due to significant sensory loss or irregular visual input.
Diagnosis:
Sensory ataxia is diagnosed by a comprehensive approach that involves a detailed medical history, neurological and physical tests, and several rounds of diagnostic testing. The goal is to limit the degree of sensory impairment and the underlying cause of sensory dysfunction. The diagnostic procedure is described as follows, with illustrations:
Medical History
- Find out when the symptoms started, how they developed, and whether there are any related complaints (such as pain or numbness).
- Health and Family Background: Examine any history of hereditary disorders, diabetes, vitamin deficiencies, or neurological issues.
- Take into account past medication use, alcohol use, exposure to toxins, and any recent infections.
Physical and Neurological Examination
Walk and balance evaluation: Conduct balance tests (such as the Romberg test, in which the patient stands with their eyes closed) and look for signs of unsteadiness in the patient’s gait.
Sensation analysis evaluates a range of emotions, including:
- Proprioception: To assess the patient’s capacity to detect limb position and move their limbs, ask them to point to a spot.
- Vibration Sense: Try your ability to sense vibrations using a tuning fork.
- Test your ability to detect light touch and temperature using a cotton wisp and warm or cold things.
- It is necessary to perform coordination tests.
Diagnostic tests
- MRI or CT scan: An MRI or CT scan may be done to look for signs of brain damage.
- Laboratory tests: Blood composition is impacted by some forms of ataxia.
- Vitamin Deficits: Check for deficiencies in B12, D3, C, and other important vitamins.
- Diabetes: Check hemoglobin and blood sugar levels.
- Immunological markers: Keep an eye out for indicators of autoimmune conditions, such as anti-nuclear antibodies linked to lupus.
- Urinalysis: This test checks for systemic or metabolic issues affecting nerve function.
- Genetic Testing: For inherited ataxias like Friedreich’s ataxia, genetic testing may be necessary.
Imaging studies
- To picture the brain and spinal cord, find lesions or structural abnormalities, and diagnose conditions like cancer and multiple sclerosis, magnetic resonance imaging, or MRI, is used.
- The computed tomography, or CT, scan is an alternative to magnetic resonance imaging (MRI) for detecting structural damage or abnormalities.
Electrophysiological Tests
- Nerve Conduction Studies (NCS): These tests help diagnose neuropathy by measuring the strength and speed of electrical signals that travel via peripheral nerves.
- Electromyography (EMG) detects anomalies in motor neurons and measures electrical muscle activity.
Cerebrospinal Fluid Analysis
Lumbar puncture: Examine the cerebrospinal fluid (CSF) following a lumbar puncture for signs of inflammation, infection, or demyelinating diseases like multiple sclerosis.
Customized tests
Sensory Motivated Potentials: To assess the health of the sensory system and monitor the electrical activity in the brain in response to sensory inputs.
Reference to Specialists
- For an extensive neurological evaluation and treatment, consult a neurologist.
- Endocrinologist
- Geneticist: To carry out genetic testing and offer guidance if hereditary ataxia is discovered.
Treatment of sensory ataxia:
You should think about using analgesics or neuropathic painkillers like gabapentin or amitriptyline if pain is a primary symptom.
Pain relievers: If you have moderate to severe pain, over-the-counter medications like ibuprofen and acetaminophen should help. For extreme pain, prescription medications such as opioids or some antidepressants may be utilized.
Medications for Neuropathic Pain: If neuropathic pain or nerve injury is the cause of the pain, gabapentin or pregabalin may be prescribed.
Localized pain relief can be achieved with topical analgesics or patches that include lidocaine or capsaicin.
Injection and Approaches:
- Steroid Injections: If you have joint or muscle issues, corticosteroid injections can help lower pain and inflammation.
- Nerve blocks are said to help with excruciating pain that is restricted to a certain body location.
- Heat and Cold Therapy: Ice packs or warm compresses can help reduce inflammation and pain.
- Massage therapy: A gentle massage should help to ease tense muscles and increase blood flow, which could lessen pain.
- Gentle Stretching: Consistent stretching can help reduce muscle stiffness and increase flexibility, both of which may help lessen pain.
Physiotherapy Management:
Principles of Training
- It is recommended that exercises be done intentionally at the start of the training program and then naturally as it goes on.
- The workout routine needs to progress from easy to difficult.
- Every balance exercise involves using one’s eyes.
- Once proximal stabilization has been achieved, assess the combined movement of the descending sections.
- Compensation measures should be used in conjunction with supportive aids and equipment where needed.
- Together with treatment, a suitable at-home exercise regimen and sports should be implemented.
- For ataxia physiotherapy and rehabilitation to provide the supposed results, the treatment plans must be planned according to the patient’s preferences.
- Analysing the findings and using the proper measurement and evaluation methods will help achieve this.
- Measurement and assessment are used to follow the patient’s condition over time and analyze the treatment’s results, as well as to create a suitable treatment plan.
- Two of the most difficult parts of neurological rehabilitation applications are standardization issues in assessment and measurement, which are made considerably worse by ataxia.
- More scales, observational techniques, and computer systems developed to measure balance rather than incoordination are found in the literature.
- Even though they are simple to use and appropriate for clinical settings, scales and observational methods typically used to evaluate balance have limited capacity to produce reliable data, and the outcomes can change depending on the experiment.
- Even though computerized systems are quite reliable, they are expensive and need a lab setting to function. The use of balance assessment instruments by physiotherapists is common.
Methods of Balance Assessment
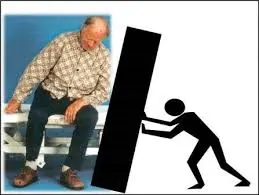
- External Perturbation Test – The objective of the push-and-release test for external perturbations is static balancing.
- The pull test, also known as the external perturbation test, aims to achieve static balance in a range of sensory contexts.
- The primary goal of the sensory integration test using computerized dynamic posturography is to assess both attached and fixed equilibrium.
- Both gait and functional dynamic balance are assessed using the five-times sit-to-stand test.
- Assessing walking skills and maintaining functional dynamic balance is done using the Time and Go Test.
- The goal of being able to stay upright and stable while executing tasks that call for self-movement is explained by the four-square-step test.
- Gait duration, step length, step breadth, and the tests mentioned above must be determined in between them. Self-perception measures like the Dizziness Handicap Inventory and the Activity Specific Balance Confidence Scale, and daily living measures like the Barthel Index and FIMTM, can be used by patients to help with assessment techniques.
- Just a small number of scales have been developed and evaluated for validity and reliability to evaluate both extremity ataxia and truncal ataxia.
Scales for sensory ataxia
Scale for evaluating and rating ataxia (SARA)
- The aim is to evaluate the severity of ataxia and how it affects day-to-day functioning.
- Among the elements are exercises for posture, walking, sitting, talking, and limb coordination.
- Score: Each action is assigned a numerical value between 0 and 40.
The International Cooperative Ataxia Rating Scale (ICARS)
- Assessing the degree of ataxia in several areas, such as speech, limb coordination, and movement, is the aim.
- Components: Consists of many subscales that assess limb motions, posture, and oculomotor function, among other aspects of ataxia.
- Scoring: Each subscale is evaluated independently, and the sum of the values indicates how severe the ataxia is.
Nine-hole peg test (NHPT)
- The objective is to assess individuals with a range of neurological diseases on their capacity to use their fingers, hands, and arms to complete a task.
- Components: Determines how long it takes to use both hands to place and remove Pins from a pegboard.
- Scoring: The amount of time needed to complete the task is noted; larger durations signify more challenges with fine motor abilities.
Upper extremity ataxia can be assessed using a computer graphics tablet.
Ataxia Scale of Scotland (AS-S):
The purpose of the Ataxia Scale is to evaluate the impact of ataxia on day-to-day functioning and quality of life.
Self-reported symptoms and functional limitations are among the components.
The genuine impact of ataxia on their attitude toward life is assessed via scoring.
Balance and Coordination Training:
Exercises for balance: to improve coordination, walking, and balancing.
- Static equilibrium exercises, such as standing on one leg or balancing on a foam cushion, could help you become more stable.
- Activities like walking on uneven ground or arriving while standing can help you develop dynamic equilibrium.
Coordination Exercises:
- Using tweezers, buttoning shirts, and handling small objects are examples of fine motor exercises that improve dexterity and hand-eye coordination.
- Gross motor activities are exercises that improve overall coordination by requiring large motions, like catching a ball or using resistance bands.
Static Balance Exercises
Single Leg Stance:
- Sustain your balance while balancing on one leg.
- Hang onto the wall for support if the patient is unable to stand on one leg. Elevate a single leg and distribute weight evenly across it. Hold yourself in the single-leg posture for 10 to 20 seconds. Restart after changing legs.
- Progress: Begin by performing the exercise without help and progressively increasing the hold time.
Tandem Stance:
- Put yourself in the tandem stance.
- With the sole of the anterior foot overlapping the toes of the posterior foot, place one foot forward and the other backward. Hold the tandem position for 10 to 20 seconds. Change your foot positioning and start over. Change your foot positioning and start over.
- Progression: Increase the duration gradually and try to finish the workout on your own.
Wide Stance:
- It is advisable to place your feet broader than your shoulders apart.
- Straight standing is the way to proceed. Ensure that your weight is distributed evenly. Sustain an upright stance for around 15-20 seconds.
- Progression: Reduce your stance gradually as your balance gets better, or for a harder test, close your eyes.
Heel-to-Toe Stand:
- Arrange the sole of one foot in front of the opposing sole’s toes to finish this. Your body should remain erect from heel to toe for 10 seconds.
- Progress: Try maintaining the posture on an inconvenient surface or for longer periods.
Dynamic Balance Exercises
Heel-to-Toe Walking:
- How to do it: Walk in a vertical line with your foot’s heel exactly on the other foot’s toes. Keep your path straight.
- Progress: Extend the path and try starting an obstacle walk.
Bosu Ball stance:
- Perform these exercises to improve your balance.
- Place your feet shoulder-width apart and assume a stance on the baseball surface. Ten seconds should be spent in the Bosu ball stance.
- Progress: Extend the time or try closing your eyes while maintaining your balance on the Bosu ball.
Foam Pad Stand:
- Steps to follow: Lay out a foam pad on the ground. To begin, place your feet shoulder-width apart. Maintain equilibrium for a duration of fifteen to twenty seconds.
- Progress: Experiment with different foot locations on the foam pad and progressively extend the duration.
Static Balance With Visible and Sensory Challenges
Eyes Closed Stance:
- Directions: Assume a tandem or single-leg position. Shut your eyes and keep them closed for 10 seconds.
- Progress: Increase the hold time and try to complete the exercise on your own.
Head Movement Stance:
- Use the standing head exercises to verify your balance.
- Rules: Stand in tandem or on one leg. Turn your head slowly from side to side or up and down while maintaining your balance.
- Progression: Increase the duration and try out various head movements.
Functional Balance Exercises
Stepping Exercise
- Directions: Take intentional steps forward, backward, and sideways. Take advantage of a step or a low platform to make it more challenging.
- Progression: Increase the step’s height or make adjustments like stepping over obstacles.
Finger-to-Nose Test:
- Specifics: Increase your efficiency and hand-eye coordination.
- Put your index finger on the nasal part of your nose while holding out one arm in front of you. Change hands. Execute with control and gentleness.
- Progression: Increase speed gradually without sacrificing precision.
Buttoning Practice:
- Points: Improve your grip on daily tasks.
- Instructions: Try using a button board or buttoning and unbuttoning an article of clothing. Make sure to combine your thumb and fingertips.
- Progress: Use smaller buttons.
Coin Transfer:
- Procedures: Transfer coins across locations. To change the challenge, use different coin sizes.
Gross Motor Coordination Exercises
Ball Throw and Catch:
- Points: Improvement in timing and hand-eye coordination.
- With one hand, bring the ball and drop it against the wall next to you. Start with bigger balls and work your way down to smaller ones.
- Progression: For a more challenging activity, select a different ball size or increase the distance.
Heel to shin test
- The Heel-to-Shin Test: Place your heel on another knee while seated, then move it down your tibia to your ankle. Change legs.
- Progress: Increase the pace or perform the workout while standing.
Obstacle Course:
- Explanation: Gain dynamic equilibrium and problem-solving skills.
- Create a simple obstacle course using cones, cushions, and other household objects. You can navigate the course by walking, stepping over, or crawling under obstacles.
- Progressing: Incorporate timed assignments or increase the course’s level of difficulty.
Visual and Sensory Coordination Exercises
Target Practice:
- Description: Improves accuracy and visual-motor coordination.
- Establish a goal, attach a tape circle to the wall, and throw small items like cushions. Focus on accuracy and targeting.
- Progress: Use smaller targets or increase your distance from the target.
Tracing shapes:
- The explanation is to improve grip control and hand-eye balance.
- Create patterns or characters on paper with a pencil or your finger.
Functional Coordination Exercises
Cooking Tasks:
- A clarification: Make use of regular kitchen tasks to enhance coordination.
- Guidelines: Estimating supplies, combining, and cutting with a safe knife are all part of cooking chores. These tasks require hand motions.
- Progress: As your coordination improves, practice difficult dishes or tasks.
Household duties:
- Description: Make coordination exercises a part of your everyday routine.
- Daily tasks include things like sweeping, vacuuming, and putting away clothes.
- Pro-level refers to an elevated time frame.
Advanced Balance and Coordination Exercises
Balance Board Exercises:
- How to Do It: Perform lunges and squats while standing on a balancing board.
- Progress: Include close-eye balance or arm motions.
Usage of Visual and Vestibular Feedback
Gaze stabilization
- How to do it: To improve gaze stability and lessen vertigo, move your head or body while focusing on a stationary object.
- Progression: Change the visual goal or accelerate head movements.
Eye/Head Coordination:
- How to Do It: Keep your eyes on a goal and move your head. Alternate between different routes.
- Progress to: Involve head and eye movements at different speeds and angles.
Tips for Successful Practice
First security measure: Establish a secure environment to prevent falls. As needed, use protective gear and abuse supports.
To get the most out of your workouts, persistence is essential.
Make gradual progress: As your abilities advance, progressively increase the level of difficulty from simple exercises.
Seek advice from professionals: To tailor exercises to your needs and capabilities, consult with a physical or occupational therapist.
Helps avoid deconditioning and maintain or increase muscle strength.
By enhancing muscle strength, stability, and functional mobility, strength training may aid in the management of sensory ataxia. Strengthening muscles may improve joint support and overall stability, particularly when sensory input is diminished. A comprehensive guide on strength-training exercises for individuals with sensory ataxia can be found here.
Core Strengthening
Chair squats
- How to Do It: Take a straight stance in front of the chair.
- Maintaining your weight in the centre and your knees parallel to your toes, cautiously approach the chair as though you were going to sit down.
- Just over the seat, pause, then stand up again.
- Perform 10–20 repetitions.
Advancement: Increase the overall quantity of repetitions.
For an added challenge, hold on to resistance bands or lightweight dumbbells.
Chair yoga poses
- How to Do It: Use a chair for support when performing gentle yoga poses such as chair poses, sitting twists, or seated forward curves.
- Progress: Try out more difficult poses and longer holds.
Standing Side Leg Lifts
- How to Do It: For support, stand close to the wall.
- Keeping your body upright, push one leg towards the centre.
- Perform 10–15 repetitions for each leg.
Progress: Increase pressure by adding ankle weights.
Do twice as many reps.
You will be able to do the exercise without assistance as your balance improves.
Planks:

The way to perform it is to lie down on your face and then raise your body straight up onto your toes and forearms.
Advance to: Increase the hold duration or try using side planks for variation.
Plank (modified):
- How to Do It: Start in a modified plank position, keeping your body upright from head to knees by bending your legs and placing your forearms on the floor.
- Hold that modified plank for ten to fifteen seconds.
- Focus on maintaining the hip level and using the abdominal muscles.
Progression: Increase the holding time gradually.
Seated Knee Extension

- How to Do It: Instruct the person experiencing pain to sit with the sole of the chair on the base of a suitable chair.
- With one leg extended in front of your face and the other on the floor, maintain this position.
- Hold off on sinking the leg for a few seconds.
- Perform ten to twenty elongations on every leg.
Advancement: Add small ankle weights.
For sitting knee extension, increase the number of repetitions or rest periods.
Bird Dog

- How to Do It: Keep your posture camel-like.
- After a few seconds of waiting, go back to where you were before.
- On the other side, repeat.
- Perform 10–20 repetitions on each side.
Progression: Increase the number of repetitions or hold time.
Bridging

- To perform, lie back on the mat with your hips semi-flexed in a V, knees bent, sole touching the floor, and your back supported.
- Elevate your hips from the ground, squeeze your glutes, and activate your core muscles.
Advancement: Increase the hold duration.
Tips for Core Strengthening:
- Starting rhythmically: Start with fewer repetitions and increase the number of reps as your power increases.
- Use Assistance as Needed: Use support, like a chair or a wall, to maintain stability and balance while working out.
- Focus on the Record: Use an appropriate technique to prevent injury and increase the efficacy.
- Warmed-Up and Cool-Down: Before commencing any exercise, warm up and cool down to avoid injury and enhance flexibility.
- Integrate Breathing: Effective breathing will strengthen the abdominal muscles and improve performance in general.
- Activity for the regimen: Include abdominal strengthening exercises in your daily routine, ideally two to three times a week.
Lower Body Strengthening Workouts
Since these activities enhance stability, balance, gait, and functional movement, they are essential for people with sensory ataxia. Strength training for your lower body will improve your gait, make it less likely that you will slip and fall, and give you more control over your motions. This is a summary of lower-body workouts created especially for those who have sensory ataxia.
The chair stands
- How to Do It: Tell the patient to take a seat in a chair that has the sole facing the floor.
- To stand erect, utilise your legs, bend your upper body, and narrow your front.
- Once again, take a seat gently and carefully.
- Complete 7–10 repeats.
Progress: Boost the overall quantity of repetitions.
The wall sits

- How to do it: Take a straight stance and turn your back to the wall.
- Reach your thighs about level with the floor by performing a squat-like action.
- Give the wall ten seconds to sit.
- Gradually go back to the beginning position.
Progress: Extend the holding period.
Use light weights when performing the workout.
Seated Ball Presses
Method: While seated, place a little ball at the exact center of both knees.
For a few seconds, swipe the ball and hold it in this position.
Calm down and start over.
Squeeze for 15 to 30 seconds.
Progress: Make the squeeze last as long as possible.
Make use of a bigger, stronger ball.
Steps up
- How to Approach It: Positioned directly before a staircase.
- Use a proper stride pattern when climbing the stairs, such as walking on your toes.
- One foot at a time, descend.
- Do ten to twenty reps for each leg.
Progress: Pick a platform or elevated step.
Add weights for an additional challenge.
Calf raises

- How to do it: Hold the therapist’s finger for stability while maintaining an upright posture with your feet hip-distance apart.
- Start with your toes and foot, and accelerate from there.
- Lower yourself gradually.
- Perform 10 to 20 repetitions.
Advancement: Walk while bearing weight on your ankle.
Increase your total movement and walk on uneven surfaces.
High knees
- How to Approach It: Stand with your feet hip-distance apart and, if needed, grasp a solid surface for balance.
- Raise one knee as high as you can, then lower it and raise the other.
- Perform 10–20 repetitions for each leg.
Progress: For further strength resistance, use pounds.
Dynamic lunges

- How to Do It: Move your hips far apart, place one foot ahead in a lunge position, and descend your hips until your knees flex at a 90-degree angle.
Progress: To build resistance, add little weights. Increase reps on your own.
Leg Presses: While seated, apply pressure with a leg press machine.
Upper Body Strengthening
Strengthening the upper extremities quickly improves hand strength and all functional activities.
Functional Arm Raises
- The steps are as follows: keep your feet hip-distance apart, hold a tiny weight in each hand, and push your hands in the manner the therapist instructs.
- Fundamentally, extend the arms at shoulder level in front of the face.
- Lower your arms back down gradually.
- Perform eight to ten repetitions.
Sitting Shoulder Press
- How to Do It: Point your footsole toward the floor while sitting in a study chair.
- Theraband should be held palm-front at the humeral level.
- Hold the weight for a short while.
- Return the weights to shoulder height.
- Perform eight to ten repetitions.
Progress: Increase the dumbbells’ weight.
Adjust the resistance level for more balance.
Bent-Over Rows
- Method: Hold a dumbbell in one hand with the wrist facing inward.
- Make sure your back is straight.
- At the same time, extend the shoulders and move the weights.
- Lower the weights once again.
- Do fifteen repetitions.
Progress: Increase the dumbbells’ weight.
Perform the exercise while seated to increase stability.
Chest Press

- The way to do it is to lie with your wrists facing forward and hold the barbell at chest height.
- The weights should be pushed until the arms are fully extended.
- Bring the weights down to your chest.
- Perform ten repetitions.
Progress: Increase the dumbbells’ weight.
Try the exercise with a resistance band for the counted mixture.
Seated Rows
- How to Do It: Take a seat in a study chair with your sole resting on the base.
- Using both hands, grasp the cable handle.
- With the elbows close to the torso providing resistance, stretch the resistance band as close to the body as you can.
- Return to your starting point gradually.
- Perform ten repetitions.
Progress: Increase the band’s resistivity.
Do the exercise while standing for an added challenge.
Front Raises
- The method is to sit with both feet hip-distance apart from other people.
- Carry the dumbbells up straight towards the centre of your face.
- Reduce the weights gradually.
- Perform ten repetitions.
Progress: Increase the dumbbells’ weight.
Go through the exercise slowly and steadily.
Wall Push-ups

- How to Do It: Place your feet shoulder-width apart and face a wall.
- It is necessary to place the hands on the wall at the shoulder’s humeral head.
- Maintaining an upright posture against the wall while bending the elbows.
- Perform ten repetitions.
Advancement: Start from the pro level or switch to an anticlockwise method.
Increase the number of reps.
Arm Circles
- How to Approach It: Arms extended to the sides, stand hip-spaced and apart.
- Make small, forward-moving circles with your fingertips.
- After twenty to thirty seconds, switch to circles in the opposite direction.
- Finish two or three rounds.
Progress: Enhance the time of the program or the diameter of the circle.
Occupational therapy:
Occupational therapy (OT) can be very beneficial for those with sensory ataxia. Despite the restrictions caused by sensory ataxia, occupational therapy seeks to help people increase their ability to perform daily tasks and enhance their general quality of life. Occupational therapy can be tailored to address sensory ataxia in the following ways.
Assessment and Goal Setting:
Initial Evaluation:
Functional Assessment: Identifies how sensory ataxia interferes with everyday activities such as dressing, cooking, and maintaining personal hygiene.
Assessment of Sensory and Motor Abilities: Identifies the areas of balance, coordination, and fine motor skills where sensory and motor deficiencies are most noticeable.
Target Setting: Collaborate to create realistic and achievable goals based on the evaluation’s findings.
Follow-Up Assessments: Plan frequent follow-up evaluations to see whether improvements were effective and implement any required adjustments.
Compensating for sensory deficiencies through the use of adaptive instruments or approaches.
Adaptive Equipment:
Assistive devices are tools that make everyday tasks easier, including button hooks, adaptive dressing aids, or ergonomic utensils.
Environmental Changes: Ideas for home upgrades include installing grab bars, using non-slip matting, or altering the lighting to improve visibility.
Task Modification:
Task division: To make challenging projects easier to do, break them up into smaller, easier-to-manage pieces.
Energy conservation: Instruct students in techniques like pacing and pausing that can lessen fatigue and prevent overexertion.
Sensory Integration Therapy:
Sensory Stimulation:
- Sensory Input: Techniques to improve sensory integration and awareness, such as using sensory balls or coated objects.
- Activities that help regulate sensory input and enhance the processing of sensory information are known as sensory modulation.
Sensory and Motor Activities:
- Activities that incorporate movement and sensory input, such as swinging or rocking, are known as movement-based activities.
Work and leisure activities:
Vocational Training: Support in modifying work-related activities or settings to account for motor impairments.
Leisure Activities: Support for engaging in procedures and activities that enhance interpersonal relationships and general well-being.
Safety modifications
Fall Prevention:
- Remove fall-down hazards by keeping all areas clear of electrical wires, loose carpets, and clutter. Use non-slip backing to secure loose carpeting.
- Install non-slip flooring in high-risk locations, such as restrooms and kitchens. Consider utilising non-slip mats or carpets.
- Threshold Ramps: Use thresholds or ramps to provide seamless transitions between floor levels and avoid tripping.
Grab bars and handrails:
- To improve stability and balance, install sturdy handrails on both sides of corridors and stairwells.
Lighting:
- Enough Lighting: Make sure that every area is well-lit, especially the corridors and stairs. Use non-reflective, brighter lighting to improve vision.
Accessibility Modifications
Bathroom Improvements:
- Raised Toilet Seat: To make sitting and standing easier, choose a commode with armrests or a raised toilet seat.
- Lever-handled knobs are more comfortable to use than standard knobs.
- Kitchen modifications: Raise or lower the kitchen to make room for wheelchairs or seated users. Ensure that necessary materials are easily accessible.
Living Areas:
- Furniture should be arranged to provide for clear, unobstructed pathways. If at all Possible, choose furnishings with rounded edges and avoid sharp ones.
- Furniture with Height Adjustment: Take into account tables or chairs with height adjustments for ease of use.
Mobility Enhancements
Assistive devices:
- Walking Aids: To enhance balance and mobility, use walkers, canes, or mobility scooters as necessary.
- Elevated Furniture: Select furniture with higher chairs to make sitting and standing easier.
Automated System:
- Use smart home appliances that let you operate door locks, lights, and thermostats with your voice to simplify everyday chores.
- Automatic Doors: For a comfortable entrance, invest in automatic door openers.
Sensory Modifications
Visual Aids :
- Opposing Colours: To promote spatial orientation and in-depth perception, use opposing colors on floors, walls, and furniture.
- Big Print Labels: To identify important items or locations, use legible, huge prints or letters.
Auditory Aids:
- Visual Warnings: For smoke detectors and doorbells, use visual alert systems (such as flashing lights) instead of auditory alarms.
- More Phones: To improve the discussion, get phones with better sound.
Cognitive and Functional Support
Routine and Memory Aids:
- Visual Plans: To enhance organization and memory, use visual plans or reminders for daily tasks.
- Labelling and Markings: Properly label cabinets, drawers, and rooms to aid with organisation and navigation.
Adaptable Technology:
- Voice-Controlled Devices: To do everyday tasks like setting reminders and turning on lights, use voice-activated technologies.
- Applications for tablets or smartphones: Make use of apps designed for managing everyday tasks, business, and reminders.
Emergency Preparedness
- Plan for Emergencies: Keep an emergency contact list in a convenient place.
- Put together a first aid kit and prescribed drugs.
Safe Evacuation:
- Route Accuracy: Verify that each exit is clear and accessible.
- Get emergency alert systems to notify family members in case of an emergency, such as a fall.
Communication Strategies
Speech clarity and articulation:
- Practice articulation strategies, such as repeating words, sounds, and sentences, to improve your speech clarity and pronunciation.
- Rate of Speech: To increase intelligibility and reduce the likelihood of slurred or incorrect speech, teach patients to speak more slowly.
- Breath Support: Develop your breath support and control skills to enhance speech articulation and voice quality.
Alternative Communication Methods:
- Augmentative and Alternative Communication (AAC): For people who struggle with verbal communication, find AAC tools or systems like tablets, communication boards, or speech-generating gadgets.
- Picture Exchange Tools: To increase expressiveness and comprehension, use picture-based communication tools.
Voice and Fluency
- Voice Treatment: To improve issues like hoarseness or weakness, practice voice exercises that will boost the voice’s volume, pitch, and overall performance.
- Smoothness Training: Make use of strategies to control speech fluency, like speaking more slowly or using rhythmic patterns to lessen stuttering.
- Swallowing Therapy: Interventions for dysphagic individuals that improve swallowing ability and reduce aspiration.
- Oral Motor activities: You can improve the muscles used in swallowing by engaging in activities that target the lips, tongue, and jaw.
- Swallowing Techniques: Teach techniques including the chin tuck, effortful swallow, and double swallow to increase the safety and effectiveness of swallowing.
Dietary changes:
- Texture Improvements: Vary the textures of foods and beverages to lessen the risk of aspiration and accommodate swallowing issues.
- Guide safe eating practices, such as chewing food completely and consuming it in smaller portions.
Cognitive exercises:
- Memory and Attention Training: Make use of activities like memory recall and focus-building exercises to enhance executive function, memory, and concentration.
- Problem-Solving Activities: Take part in tasks like project scheduling and arrangement that promote organizing and problem-solving skills.
Functional Interaction Training:
- Daily Conversation Tasks: To improve functional communication skills, practice common place interaction scenarios, including making phone calls or participating in social events.
- For those who have trouble speaking, there exist communication aids.
Compensatory strategies
Visual aids and reminders:
- Visual Aids: Printed reminders, schedules, and signals can help with memory and organisation.
- Communication boards or software can help to increase expressive language and improve communication.
Family and Caregiver Training
Education
- Communication Strategies: Help with speech therapy activities and instruct family members and carers on how to use AAC devices.
- Swallowing Safety: Educate carers on safe swallowing practices and how to spot signs of aspiration or trouble swallowing.
Assistance and Engagement:
Participation in Therapy: Encourage family members and caretakers to attend therapy sessions to gain a better understanding of the person’s needs and how to best assist them.
Psychological Support
- Counseling: Offering patients psychological help while they cope with how sensory ataxia affects their quality of life.
- Social Services: Helping people access community services, benefits, and resources.
Cognitive Behavioral Therapy (CBT):
- Pain Management Techniques: Cognitive behavioural therapy (CBT) can assist individuals in developing coping mechanisms and addressing the psychological or emotional aspects of their chronic pain.
- Stress Reduction: Stress can exacerbate pain, but it can be managed with the use of mindfulness and relaxation techniques.
Support categories:
Social Support: Attending support groups for individuals with chronic pain or sensory ataxia can offer both practical pain-management advice and emotional support.
Lifestyle adjustments
- Anti-Inflammatory Diet: Eat foods high in omega-3 fatty acids, whole grains, fruits, and vegetables that have anti-inflammatory properties.
- Hydration: Maintaining proper hydration can help reduce discomfort and enhance general health.
Sleep hygiene:
- Good Sleep: You can better control your pain and feel better all around if you get enough restorative sleep.
Supporting Care
- Helpful devices: Movement helps people use wheelchairs, walkers, or canes to increase mobility and prevent falls.
- Magnifiers and modified keyboards for people with visual or fine motor impairments are examples of sensory aids.
- Disease treatment, including comprehending the disease and its progression and effectively treating symptoms, is the main focus of patient and family education.
- Establishing a connection with support groups to receive both practical and emotional assistance.
Periodic Monitoring and Follow-up
- Continuous Evaluation: Arrange frequent check-ups with medical professionals to assess the progression of the condition, modify treatment plans, and address any emerging symptoms.
- To provide comprehensive management, neurologists, physical therapists, occupational therapists, and other clinicians work together to provide multidisciplinary care.
What are some ways to prevent sensory ataxia?
Here are a few avoidable reasons why people develop sensory ataxia. Many of the causes, however, are unavoidable because they happen in Unexpected ways. Furthermore, it’s not always possible to reduce the likelihood of suffering from this symptom.
The factors listed below are frequently to blame for sensory ataxia, although they are not always avoidable:
- Alcohol intoxication: Moderate or no alcohol consumption can help prevent ataxia.
- Head injuries and severe migraines: Safety equipment, like helmets, might lessen the risk of ataxia brought on by head damage.
- Prescription and over-the-counter medications, including those for epilepsy and depression. If a medication is causing your ataxia, you should consult your doctor before stopping it. Because stopping some drugs suddenly can have harmful side effects, it is recommended to consult your doctor before doing so.
- Getting enough sleep is a key tactic to avoid ataxia.
- Ataxia is one of the several problems that can arise from huffing. Because misusing inhalants like these can be fatal, it is advised to avoid using them or to stop using them right away.
- Reaching a healthy weight and staying there. Stroke is among the illnesses that are linked to physical fitness and weight and that impact brain circulation. Maintaining your physical health can occasionally prevent, or at least postpone, the occurrence of circumstances that ought to result in these problems.
- You must wear protective gear and adhere to safety protocols if you must work near hazardous items.
- Vitamin deficiencies and nutritional problems (e.g., low levels of vitamin B12).
How long might a person with sensory ataxia expect to live?
Your lifespan won’t be impacted by many ataxia causes, particularly those that are transient, treatable, or reversible.
On the other hand, some ataxia reasons may significantly affect your life. Some can make it harder for you to live your life on your own, shorten your life expectancy, or keep you from enjoying certain hobbies. Your healthcare provider is the best individual to determine whether sensory ataxia may impact your endurance and quality of life.
Risk Factors of Sensory Ataxia:
Conditions that impact the sensory nerves, such as diabetes, vitamin deficiencies, and alcohol addiction, are risk factors for sensory ataxia. Neurological problems like multiple sclerosis, autoimmune diseases, and some drugs are additional factors. Sensory ataxia can also develop as a result of age and genetic causes. To avoid difficulties, these risk factors must be identified early and managed.
Diabetes mellitus damages the nerves in the lower limbs, which raises the risk of sensory ataxia.
The harmful effects of chronic alcohol misuse on peripheral nerves make it an established risk factor for sensory ataxia.
A lack of vitamin B12 can cause sensory ataxia because it damages the neurons that control coordination and proprioception.
Sensory ataxia is a side effect of some medications, including antiretrovirals and chemotherapeutic treatments.
By targeting the neurons responsible for balance and coordination, autoimmune diseases such as multiple sclerosis can make people more susceptible to sensory ataxia.
Conclusion
In summary, sensory ataxia results in problems with balance and coordination, particularly when there is insufficient or no visual information. Numerous things, such as neurological disorders, spinal cord issues, and peripheral neuropathy, might contribute to it. Addressing the underlying cause, improving sensory input through rehabilitation, and altering the surroundings to increase function and safety are typically the main goals of management.
FAQs
How does sensory ataxia progress?
Gene defects that result in abnormal proteins are the cause of hereditary ataxia. These result in ataxia by harming nerve cells. As the condition progresses, muscles become less responsive to orders from the brain. This eventually impairs balance and coordination.
Is there a cure for sensory ataxia?
Therapy is typically used to treat your symptoms, but in certain cases, it may also be able to address the root cause of the issue to improve it or prevent it from getting worse.
Does sensory ataxia qualify as a disability?
If you have been diagnosed with ataxia of any kind, you may qualify for Social Security disability benefits.
What is harmed in a person with sensory ataxia?
A kind of ataxia known as sensory ataxia (SA) results from damage to the somatosensory neurones that disrupts sensory feedback signals. It is characterized by poor coordination and postural instability, which worsen when visual cues are removed.
Is there a family history of sensory ataxia?
This mode of inheritance is called autosomal dominant when a person with genetic ataxia receives a dominant gene from one parent. They may also have inherited a recessive gene from both parents in the event of an autosomal recessive inheritance pattern.
Does a patient with sensory ataxia lose their balance when they close their eyes?
When putting off their garments over their heads or closing their eyes during a shower, they usually complain of losing their balance in the dark.
Which drugs cause ataxia in the senses?
Benzodiazepines are the most frequently reported adverse effects in children with epilepsy. Most of the time, ataxia is moderate and treatable. Elderly people may also experience benzodiazepine ataxia.
Does ataxia affect speech?
The problems that affect speech, balance, and coordination are caused by sensory ataxia. While ataxia can affect any part of the body, speaking, walking, and balancing are common challenges for those who have it.
What is the process for sensory ataxia?
Sensory ataxia may result from injury to the thalamus or parietal lobe, which interprets afferent information, or to the dorsal columns of the spinal cord, which transmit proprioception.
Will sensory ataxia cause damage to the nerves?
As the name suggests, ataxia neuropathy spectrum disorder is typified by problems with balance and coordination (ataxia) and abnormalities in nerve function (neuropathy). Neuropathy can be divided into three categories: mixed, sensory, and motor.
How are tests for sensory ataxia conducted?
Blood tests. Imaging studies. A brain MRI could help identify the possible causes.
Does stress cause sensory ataxia?
It may not be as widely recognized that stress can also affect motor function. Ataxia, a severe loss of coordination, and dystonia are temporary symptoms experienced by patients with EA2.
Does sensory ataxia occur in episodes?
Walking, mobility, and balance are all impacted by episodic ataxia, a genetic condition. These issues arise when the start and finish of episodes are distinct. Medical practitioners can help you manage your symptoms with medication and physical therapy, even though there is currently no recognized cure for episodic ataxia.
Which foods are best avoided by those who have sensory ataxia?
Avoid processed meats that contain chemicals and preservatives. Above all, drink six to eight 8-ounce glasses of liquids each day and stay away from sugar-filled and diet cold drinks, as well as fruit drinks that include sugar or artificial sweeteners.
Can someone with sensory ataxia fully recover?
There is no known treatment for hereditary ataxia. Therapies, however, can help manage symptoms. The underlying reasons for ataxia, such as a stroke, low vitamin levels, or exposure to dangerous substances or medications, are the focus of treatment.
References
- Wikipedia contributors. (2022, June 5). Sensory ataxia. Wikipedia. https://en.wikipedia.org/wiki/Sensory_ataxia
- Sensory ataxia: Signs, causes, and treatment. (n.d.). https://www.medicoverhospitals.in/diseases/sensory-ataxia/
- Mandaliya, D. (2024, October 25). Sensory Ataxia – Cause, symptoms, treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/sensory-ataxia/#Physiotherapy_Management
- Sensory ataxia (Concept Id: C0240991) – MedGen – NCBI. (n.d.). https://www.ncbi.nlm.nih.gov/medgen/66020
- Chhetri, S. K., Gow, D., Shaunak, S., & Varma, A. (2014). Clinical assessment of the sensory ataxias: diagnostic algorithm with illustrative cases. Practical Neurology, 14(4), 242–251. https://doi.org/10.1136/practneurol-2013-000764
- Donnelly, K. (2010). Sensory Ataxia. In Springer eBooks (pp. 2258–2259). https://doi.org/10.1007/978-0-387-79948-3_782
- Mj, S. (2015, April 21). Sensory ataxia [Slide show]. SlideShare. https://www.slideshare.net/slideshow/sensory-ataxia/47234261