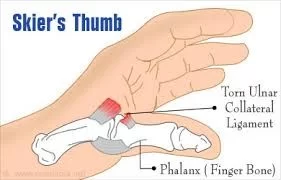
Skier’s Thumb (Ulnar Collateral Ligament Injury- Thumb)
Introduction:
Skier’s thumb is also known as “gamekeeper’s thumb,” which refers to a common injury to the thumb’s ulnar collateral ligament (UCL). Usually, it occurs by a rapid, strong, outward bending of the thumb, like when you fall while carrying a basketball or a ski pole.
The base of the thumb joint is stabilized by the UCL, and damage to this ligament can result in joint pain, edema, and instability. In extreme circumstances, the ligament might be injured, necessitating surgery. In order to treat a skier’s thumb, the thumb is usually immobilized with a cast or splint. Physical treatment may also be necessary to regain joint strength and mobility. A successful recovery and the avoidance of long-term consequences depend on early diagnosis and treatment.
Definition:
Injury to the thumb’s ulnar collateral ligament (UCL) (also known as the metacarpophalangeal joint, or MCPJ) increases the risk of chronic instability if left untreated. The lesion typically occurs when a skier’s thumb is forced to turn radially by the ski pole. An actual UCL rupture.
The skier’s thumb identified the cause as acute damage, despite the fact that the two terms are commonly used interchangeably. The thumb of the goalie is particularly cited as the cause of protracted UCL damage that was weakened by repeated strain. If not properly treated, chronic injury-induced UCL damage may still pose a serious risk of impairing mobility, pinch grip strength, and instability.
Clinical Relevant Anatomy:
Supported by a capsule and other soft tissue components, the thumb’s metacarpophalangeal joint is a diarthrodial joint that allows for unrestricted joint mobility. Both dynamic and static stability are displayed by the nearby soft tissue.
The following constructions provide passive stability:
- Proper collateral ligament
- Supplementary collateral ligament
- Volar plate
- Posterior capsule
From a location just posterior to the metacarpal head’s mid-axis to the palmar part’s proximal phalanx, the correct collateral ligament extends. It serves as the initial barrier against valgus stress with the metacarpophalangeal joint in the flexion direction and prevents palmar displacement of the proximal phalanx. In order to insert into the anterior plate, the complimentary collateral ligament distribution is palmary. Proximally, the appropriate collateral ligament is next to the accessory collateral ligament. The primary barriers against valgus stress with the metacarpophalangeal joint in the extension direction are the anterior plate and the supplementary collateral ligament.
The thumb’s intrinsic and extrinsic muscles are active stabilizers of valgus stress:
- Extensor pollicis brevis
- Extensor pollicis longus
- Flexor pollicis longus
- Adductor pollicis
- Flexor pollicis brevis
The deep insertion of the adductor mechanism extends to the palmar side of the proximal phalanx through the ulnar sesamoid of the metacarpophalangeal joint, whereas the superficial insertion is the extensor expansion through the adductor aponeurosis. The thumb’s MCPJ is traversed by two main supporting ligaments:
- Ulnar collateral ligament (UCL)
- Radial collateral ligament (RCL)
The UCL and RCL attach to the base of the proximal phalanx on their respective aspects, below the adductor aponeurosis, after emerging from the medial and lateral tubercles of the metacarpal condyles. Thumbs are kept from pointing too far away from the hand by the UCL.
Epidemiology:
It affects only about 200,000 patients annually in the USA and accounts for 86% of all thumb injuries. After knee trauma, the skier’s thumb is the second most common injury sustained while skiing and it affects males more often than women. The prevalence of this trauma during skiing varies from 7 percent to 32 percent of all skiing injuries, making it the most frequent upper limb injury suffered by skiers. Just 10 percent of the patients who were assessed using a skier’s thumb had this injury.
The most frequent cause of a skier’s thumb, which affects over 40% of patients, is a fall on the extended hand, typically from a bicycle or motorcycle (the thumb becomes stuck down the handlebars). An additional 30% of the causes are thought to be related to other sports, such as fighting or soccer. Hyperabduction trauma significantly causes a Salter-Harris III avulsion of the UCL insertion and invariably a genuine rupture of the UCL in children, who still have an adolescent skeleton.
Mechanism of Injury in Skier’s thumb:
It is important to note that this injury is not exclusive to skiers and can occur to anyone if the thumb experiences high valgus stress force during abduction and extension or a small amount of repetitive valgus stress force. Other sports, particularly those using a stick or ball, such as basketball or hockey, are also susceptible to this type of injury.
While a forced abduction action would injure the RCL, an acute UCL injury occurs concurrently with rapid, hyper-abduction and hyper-extension stress at the MCP joint. When it comes to skiing, the trauma usually occurs when someone lands on an extended hand while holding a ski pole, forcing the thumb to be abducted with extension. Known as a skier’s thumb, it can also occur during a handshake, rugby, basketball, football, handball, and soccer. Inappropriate treatment of the UCL injury may lead to arthritis, joint instability, pain, weakness, and persistent laxity in the MCPJ.
Pathophysiology:
Although the thumb’s anatomical function is complicated and outside the purview of this article, it is important to understand that the ulnar collateral ligament helps to stabilize the thumb at the metacarpophalangeal joint.
The thumb works in tandem with hand muscles, finger muscles, and ligamentous structures, such as the ulnar collateral ligament, to effectively grab and hold onto objects. One may see how severe hyperextension (or extreme abduction) might damage the ulnar collateral ligament by understanding this mechanism of thumb function.
There are three types of tears: partial, total, and chronic. The patient may experience pain and edema in the first metacarpophalangeal joint, as seen in other acute joint injuries. Additionally, laxity or instability may be observed at that joint.
Cause of Skier’s thumb:
Trauma is frequently identified as the main cause of a UCL injury. When the thumb is directly traumatized, it frequently twists or bends abruptly to the side or back. Imagine your hand exerting too much energy to bend your thumb in an unusual manner. That is the exact mechanism by which a UCL rupture occurs.
You have a higher chance of suffering a UCL injury if you are an athlete or frequently engage in high-impact sports like baseball, basketball, football, racquet sports, or snowboarding. Additionally, when the hand is attached to a ski pole, the thumb is especially susceptible to a UCL injury, as the term “skier’s thumb” implies.
In addition to high-impact sports like skiing, a fall onto an outstretched hand that causes the thumb to deviate away from the palm can also result in a thumb UCL injury.
- Excessive thumb abduction and hyperextension cause it.
- The distal connection of the proximal phalange is where the majority of UCL tears occur.
- Thumb hyperextension that causes trauma
- Usually connected to falls, especially when holding anything in the hand, like a ski pole.
- Chronic instability may result from injuries caused by overuse syndrome.
Symptoms of Skier’s thumb:
Pain on the ulnar side of the thumb’s MCPJ is the most common manifestation. Inflammation and bruises will be seen if the damage is resentful. Palpable soreness may be present, limiting the extent of injury to the thumb’s ulnar side when the UCL is injured. Patients in more chronic conditions typically report thumb instability when doing these ADLs, as well as pain and weakness in the pincer grip. A palpable lump that is situated close to the adductor aponeurosis is present in the Stener lesion example.
These signs and symptoms may appear minutes to hours after the injury-causing fall:
- In the webspace between the thumb and index digits, there is pain near the base of the thumb.
- Swelling in the thumb.
- Weak grasp between your thumb and index fingers or trouble holding an object.
- Sensitivity when your thumb’s index fingers are palpated.
- The skin around the thumb appears discolored, either blue or black.
- Pain in the thumb that gets worse when you move in practically every direction.
- The pain that comes from your thumb may be referred to as wrist ache.
Grades of thumb injuries:
The degree to which the ligament is pulled or injured away from the insertion determines the grade of thumb sprains. Below is a classification of UCL injury based on Hintermann et al.
Type-Injury Examination:
- I had a fracture that moved. Stable in flexion
- II Fracture displacement No special test
- III No fracture In flexion, stable (<30°) IV Not a fracture In flexion, unstable (>30°)
- V Volar plate avulsion fracture In flexion, stable.
Differential Diagnosis:
Bony structures, tendons, neurological tissues, the auxiliary collateral ligament, and the adductor aponeurosis are among the various structures that may be impacted. One of the most prevalent complaints of injuries is pincer grasp weakness. The area of soreness, however, may determine them.
- Stener lesion: A sterner lesion occurs when the thumb is violently abducted, causing the distal ulnar collateral ligament to avulsion from the bone beneath the thumb’s proximal phalanx.
- Bennett or Rolando fracture: An intra-articular fracture luxation at the base of metacarpals I in the carpometacarpal joint is known as a Bennett or Rolando fracture.
- Avulsion fracture: Excessive abduction concussion in children, who still have an immature skeleton, typically results in a Salter-Harris III avulsion of the UCL insertion and, less frequently, in a complete rupture of the UCL.
- Wrist fracture.
- Dislocation of the first metacarpophalangeal joint.
- Lunate dislocation.
- Rheumatoid arthritis or osteoarthritis.
- Wrist sprain: this condition occurs when the wrist’s ligaments are stretched beyond their normal limits.
- Prolonged instability of the first MCP joint: If left untreated, damage to the two main assistive ligaments that cross the thumb’s metacarpophalangeal (MCP) joint can cause symptomatic joint fluctuation, including pain, weakness, and arthritis.
- Neuropraxia: Stiffness, edema, or traction can cause neuropraxia of the radial nerve.
Diagnosis of Skier’s thumb:
X-rays: To rule out any associated bone involvement, the thumb’s lateral and anterior X-ray films are evaluated. Twenty to thirty percent of UCL injuries are related to bone avulsion fractures. The location of the distal end of the UCL is typically indicated by the tip of an avulsed bone fragment. Avulsion fractures with displacement greater than 5 mm or any fracture involving at least 25% of the MCP joint surface are not indicated for surgical therapy backed by imaging. Even for diagnosis, thumb MCP joint stress X-ray films have been used.
MRI: With a sensitivity of 96% to 100% and a specificity of 95% to 100%, MRI might be considered the gold standard. Ultrasonography of the thumb is an additional option. Many people recommend it as the most effective method for identifying UCL trauma, especially in cases with chronic UCL injury.
Ultrasound: Because ultrasound (US) allows direct imaging of the entire UCL and surrounding structures, it is the best and most economical option for assessing UCL injuries. In about 90 percent of cases, it determines the UCL’s torn end. Before using a glove spica cast as part of conservative therapy, the US must make the diagnosis. For example, scar tissue may contradict a diagnosis or be used to treat chronic UCL injuries, and the ultrasound cannot be used more than a week after the initial impact since the torn ligament has shrunk. For detecting Stener lesions, the US has a sensitivity of 95.4% and a specificity of 80%.
Arthrography: The enlargement of the metacarpophalangeal joint with the insertion of direct distinction material is known as arthrography, and it is visualized by MRI (MR-arthrography) or X-ray. In practically all MCPJ sprains, stability testing (done with the joint in full flexion) and additional routine radiographs continue to be the cornerstones of decision-making, according to clinical and anatomical findings and the perception of trauma mechanics.
Physical Examination:
Regarding measuring the hand at rest and in flexion to detect deformity. After doing an active range of motion (AROM), passive range of motion (PROM), and resisted movement to assess tendon integrity, if manageable, examine the hand’s feeling. At the ulnar aspect of the base of the thumb, the clinical examination may occasionally reveal a hematoma and a sensitive swelling. Before UCL stress testing, radiography is performed to detect any fractures that are visible to the thumb’s proximal phalanx or first metacarpal.
X-rays and clinical examinations are sensitive methods for identifying UCL injuries. The thumb MCP joint stability is assessed using a stress test if there isn’t a shaft fracture associated with it; the steady endpoint is shown below:
- To prevent strain, the thumb’s proximal phalanges are supported by the metacarpal, which is stabilized with the aid of a second hand.
- It is possible to detect the steady endpoint by repeating the radial focus in the extended position while the proximal phalanges are in a 30-degree flexion.
- A tear of the specific UCL and consequently a tear of the adjunct section of the UCL is indicated by a divergence of 15 degrees between the affected and alternative sides in flexion, or by a divergence of more than 35 degrees.
- The absence of a hard-end feel during inspection is a more reliable criterion for clinically diagnosing a total rupture of the UCL, whereas the presence of reduced sensation implies a complete UCL tear.
- A ligamentous bulge will be detected by the tester if there is a stener lesion.
Stress tests can be painful, and in order to do the test without causing tension in the surrounding muscles, the tester may need to administer local anesthesia. To put it simply, in cases of chronic UCL injuries, we can detect laxity or instability of the thumb MCP joint.
“Local anesthetic incursion enhanced the accuracy of assessment of ulnar collateral ligament injuries,” according to a study by Cooper and colleagues. Illustrated how, after an average of one week following the initial trauma, Oberst anesthesia in which 1-2 milliliters of lidocaine are administered into the MCP joint raises the clinical accuracy from 28% to 98%.
When a patient has an injury to the ulnar collateral ligament, they usually complain of pain that is restricted to the first metacarpophalangeal joint. Concomitant swelling around or at the base of the thumb may be seen. Usually, there is a history of trauma or falls that resulted in hyperextension or excessive thumb abduction. Acute presentations may occur shortly after the injury, or if the injury is more persistent, the patient may not show up for a while. Pain and sometimes weakness may be experienced in both cases, particularly when trying to grab objects, especially with a pincer grasp.
Making this diagnosis can be particularly aided by the physical examination. Any laxity or total breakdown of the ulnar collateral ligament can be identified with the use of a valgus stress test, which involves abducting the thumb at its base. Establishing a baseline to indicate the extent of the tear or injury can be aided by comparison with the thumb that is unaffected. There will be more laxity or movement on valgus stress tests when there are partial tears present. A complete tear with complete instability at the thumb base would be indicated by the absence of an endpoint during such testing. Asking the patient to flex the first metacarpophalangeal to 45 degrees is one way to aid in isolating the ulnar collateral ligament during testing.
According to orthopedic research, any laxity on abduction or valgus stress testing that is greater than 15 to 20 degrees is considered to be indicative of ulnar collateral ligament damage. The thumb that is unaffected should be used as a comparison. Additionally, it is very suggestive of an ulnar collateral ligament tear if the degree of laxity exceeds 30 degrees. Although the orthopedic literature describes this, the physician can find it challenging to measure the degree of ulnar collateral ligament laxity in the real-world clinical setting.
Evaluation:
When there is acute damage to the ulnar collateral ligament, imaging is usually not beneficial. Plain films of the thumb, especially of the thumb base (proximal phalanx), can help rule out bone anomalies or fractures. Along the medial (ulnar) portion of the thumb’s proximal phalanx, the ulnar collateral ligament inserts. Therefore, in the context of ulnar collateral ligament injury, an avulsion fracture may be seen. Plain X-ray imaging, however, is typically unrevealing in fact, it may be normal in these patients.
Laxity of the first metacarpophalangeal joint can be evaluated in real-time at the bedside using ultrasound. A skilled technician can examine tiny structures like the ulnar collateral ligament in detail by using the hockey stick probe. Similar to the physical examination, both thumbs can undergo ultrasound imaging to compare the two and create a baseline on the unaffected side.
Acute magnetic resonance imaging can be difficult to obtain. This method, however, offers the highest sensitivity and specificity (almost 100%) for identifying injuries to the ulnar collateral ligament, including ruptures or tears.
Treatment of Skier’s thumb:
Medical methods or conservative treatment for a UCL injury depend on the following factors, which are primarily present:
- Timing of presentation (acute or chronic)
- Grade (severity of injury)
- Displacement (Stener lesion), and distinguishing between displaced and non-displaced UCL injuries are essential for therapy.
- Trauma site (peripheral or mid-substance) concussions of large tissues, such as the volar plate, anterior plate, or bone, occur together or in association. Aspect connected to the patient (demands of the workplace, etc.)
The following describes the suggested care of UCL injuries based on Hintermann’s classification:
- Cast immobilization is required for approximately four weeks for type I injuries.
- Cast immobilization is required for approximately three weeks for Type III and Type V injuries.
- Surgery is required for types II and IV injuries.
Medical Treatment:
R-I-C-E therapy—rest, ice, compression, and elevation can be used to treat ulnar collateral ligament injuries acutely, much like it is for the majority of musculoskeletal injuries. Using a thumb spica splint also helps immobilize the affected area.
The patient should be referred immediately to an orthopedic or hand specialist if they have a bone injury, such as an avulsion fracture in the context of an ulnar collateral ligament injury. Similarly, an immediate referral to a hand surgeon is necessary if the physical examination reveals considerable laxity (more than 15 to 20 degrees relative to the unaffected thumb or greater than 30 degrees outright).
Partial tears may be treated with splinting immobilization, but it is still wise to have a hand surgeon evaluate the patient. Three weeks is the usually suggested immobilization period. Physical therapy and rehabilitation can then be applied to these nonsurgically treated conditions. After this period, patients who continue to have pain or weakness should be referred for surgery.
According to the majority of published research, patients who have surgery after suffering total ulnar collateral ligament tears recover effectively and experience few serious aftereffects. According to one study on sports-related injuries, there was a 10.3% postoperative complication rate and an overall 98.1% successful return to play following surgery without a discernible decline in performance. For full tears, early surgical intervention is typically necessary to avoid the formation of the Stener lesion, as a consequence. Surgery is advised as the final course of treatment since the ligament cannot recover properly due to this changed anatomy.
Patients with degenerative MCP joint disease are effectively treated conservatively for incomplete UCL traumas, such as ligament strains, complete tears, low-demand patients, and inadequate operative nominees.
There are also disagreements over how to treat a bony skier’s thumb without surgery. Nonetheless, the profession shows that this injury can be treated conservatively without raising any concerns as long as the MCP joint remains stable during testing and there is no segment displacement. For individuals who have:
The Metacarpophalangeal joint straightens with a valgus laxity of less than 30 degrees.
Less than 15 degrees of separation between the sides, and an X-ray shows no signs of an avulsion fracture.
Immobilization:
Depending on the level of laxity during the early evaluation, from 10 days to 6 weeks. The following recommendations, which the investigator was persuaded to make after four to six weeks and up to twelve weeks, depend on the extent of the lesion:
- A thumb spica cast for short arms
- With a thermoplastic splint, the patient can begin using their interphalangeal joint.
- A removable thumb spica orthosis that is hand-based. To prevent any unnecessary stiffness, the IP joint remains free while the MCP joint is immobilized.
- By keeping the thumb from experiencing radial stress, wearing a splint will give the ligament time to heal.
- The MCPJ in mild flexion with a small ulnar deviation is the ideal orientation for splint respect retention because it brings the torn ligament segments closer together and aids in healing; the interphalangeal joints shouldn’t be immobilized in the cast.
Surgical Treatment:
Prolonged lesions become significantly more difficult to repair with increased duration after damage because the remaining tissue becomes less robust to provide enough support to the joint. Operative treatment depends on an early detection of the traumas. Operative consideration is excluded if the trauma is grade 1 or 2 and radiographs show volar subluxation, a present unstable joint, a Stener lesion, or a displaced avulsion fracture. Numerous repair techniques exist, and they can be divided into two categories: dynamic and static.
Dynamic Static:
- Extensor indicis proprius tendon transfer
- Extensor pollicis brevis tendon transfer
- Adductor pollicis brevis tendon transfer
Dynamic methods are more likely to loosen over time, typically preserving improved MCP joint mobility.
Static:
- Figure-of-eight grafting
- Parallel configuration graft
- Triangular configuration with proximal apex graft
- Triangular configuration with distal apex graft
- Tendon graft weaves
- Hybrid technique
- Free tendon graft
The ideal treatment method is still up for debate, and there are many different types of static procedures. Many managers produce favorable results, which leads to a lot of disagreements.
A better result can still be obtained after three to four weeks, as long as the procedure was performed on time (delaying surgery reduces the choice of outcome). Immobilization is necessary for approximately six weeks, after which a fresh radiograph is taken and physical therapy can begin. For complete outcomes, the hand can be used again after the pain has subsided and the range of motion has begun to improve. This typically takes about three months. The majority of patients with deteriorated results have a delayed display. Complications are rare when repairs are made properly.
There is insufficient information available regarding the likelihood of the recurrence of this type of damage. Furthermore, no studies have yet been established to examine if surgical intervention is indeed better than non-operative treatment.
Follow up:
Following a surgical fix or a period of immobilization in a cast, the patient will be seen by the operative surgeon. A second examination of the patient’s thumb will be performed. The physician will decide whether the patient needs to continue immobilizing the thumb or whether physical therapy is necessary to restore movement.
Physical Therapy Treatment:
The treatment of a skier’s thumb varies based on the extent of the damage, including partial and total ruptures. Conservative management is used for incomplete ruptures. To maintain unnecessary stiffness, the IP joint is left free while the MCP joint is immobilized. Usually, a navicular cast or brace is recommended. Elevating the body above the level of the heart when in a supine position and applying cold compresses as necessary can help control swelling.
Enhancing function and minimizing the duration of functional recovery are the main goals of rehabilitation; the suggested treatment offers prospective benefits in the treatment of this frequent acute hand injury.
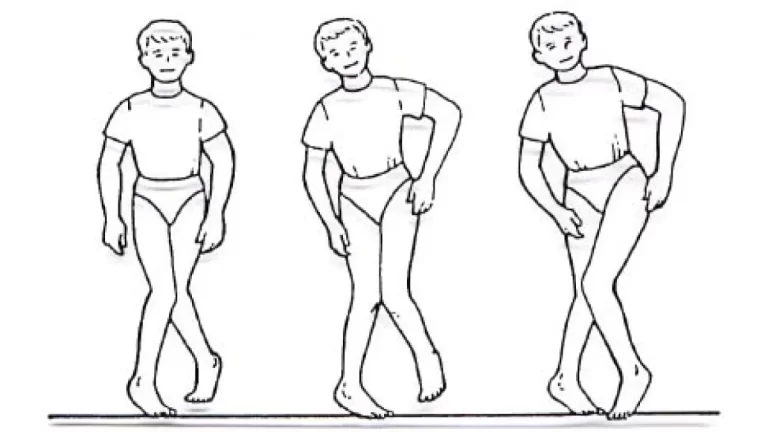
Exercise therapy:
Once the immobility phase is over, the therapy can finally begin. The patient will most likely perform exercises that help strengthen and extend the joint to regain full thumb function. The patient must begin hand rehabilitation under supervision while they are immobilized. After around four weeks, the patient can begin slowly and gently flexion and extension range of motion exercises, continuing to wear the splint in between therapy sessions.
It is possible to begin advanced strengthening exercises after 8 weeks; however, full activity is not allowed until 12 weeks. Pinching and gripping should not start until 10–12 weeks and should progress as tolerated; it usually takes a week or so to accept forceful gripping exercises.
Thumb active range of motion:
- Move your thumb as far away from your palm as you can while keeping your palm plane on a table or other surface. Take five seconds to grasp this location, then return it to the starting point. Then make a handshaking motion with your hand resting on the table.
- Stretch your thumb as far away from your palm as you can.
- Hold on for five seconds.
- Take your thumb and palm side by side and move them toward your little finger.
- For five seconds, maintain this posture. 15 times, repeat this entire sequence. Perform two sets of fifteen.
Wrist range of motion:
- Flexion: Bend your wrist forward slightly. Hold for five seconds. Perform two sets of fifteen.
- Extension: Bend your wrist back slightly. For five seconds, maintain this posture. Perform two sets of fifteen.
- Side to side: Shake your hands by lightly moving your wrist from side to side. Hold in each direction for 5 seconds. Perform two sets of fifteen.
- Thumb strengthening involves using your thumb and each of your fingers, one at a time, to pick up small objects, such as coins, paper clips, and pens. Spend five to ten minutes performing this exercise.
- Finger spring: Put a large rubber band around the outside of your thumb and fingers to create a finger spring. To enlarge the rubber band, open your digit. Perform two sets of fifteen reps.
- Grip strengthening: Strengthen your grip by continuing to squeeze a soft ball while counting for five seconds. Do two sets of fifteen reps.
- Wrist flexion: Hold a light bottle or the hammer handle in your hand palm up. Raise your wrists. Reduce the burden gradually and go back to where you were. Perform two sets of fifteen. The load of the can or cargo you are keeping is added gradually and step by step.
- Wrist extension: With your palm facing down, hold a soup can or striker handle in your hand. Bend your wrist up slowly. Reduce the load gradually to its starting position. Perform two sets of fifteen. Gradually increase the weight of the things you are maintaining.
Post-surgical treatment:
After the procedure, the physical therapy’s substance is the same as that of the conservative management, anyway:
- The immobilization period is typically six weeks.
- Radiography control following immobilization A splint is often worn for four to six weeks after surgery. Faster and more precise functional results were obtained from the operated joint’s contiguous post-operative mobility. As a result, it is recommended to use a functional splint and to begin moving within the limits of pain as soon as possible. It usually takes three to four months for athletes whose injuries require surgery to return to competition.
- According to Derkash’s written report, less than 5% of patients experience stiffness and a weakened tweezer grip when taking into account pain, stability, muscular power (tweezer grip), and functionality in ADL. In 99 percent of the cases, the pain was either nonexistent or very little. Ninety-six percent of individuals who had treatment expressed satisfaction with the procedure’s results. The results were less successful when a secondary operation was necessary. The hand can be fully used again once the pain has subsided and the range of motion has fully recovered. This usually takes about three months.
Complications of Skier’s thumb:
It is anticipated that the adductor aponeurosis, also known as a Stener lesion, may interrupt the distal end if there is injury to the UCL. Although difficult to identify, a Stener lesion results in poor healing and frequently requires surgery. A ruptured UCL can cause joint instability and pinch grip weakness if treatment is not received.
Prevention of Skier’s Thumb:
Avoiding pole dragging and deep pole plants, teaching good pole technique for powder skiing, and reducing the size of baskets from the typical 4-inch diameter to 2.5 inches are all preventive measures. The pole length should be two inches less than what the skier is advised to wear.
Although skiers may be less likely to sustain injuries if they are taught to throw the pole in the event of a fall, strapless poles do not lower the risk.
Wearing a correctly made ski glove, which not only inhibits excessive thumb movement but also has a mechanism for ejecting the ski pole, can further lower the chance of damage.
Prognosis:
Despite the lengthy period of immobilization, partial tears of the ulnar collateral ligament typically heal successfully when treated with splinting alone. In the case of full ulnar collateral ligament tears, surgery can usually be carried out without any difficulties, as was covered in the treatment and management section above. Chronic alterations in the metacarpophalangeal joint space can be seen in those who get Stener lesions or who don’t receive treatment.
Conclusion:
Thumb metacarpophalangeal joint ulnar collateral ligament injuries are frequent. The preferred imaging technique for evaluating patients with unclear results and detecting ligament damage that needs to be repaired surgically, including the frequently seen Stener lesion, is magnetic resonance imaging (MRI).
The usefulness of MRI in the management of patients with complete UCL tears is further shown by the fact that some hand surgeons now use it to categorize patients.
FAQs
How much time does it take for the thumb ligament to heal?
Post on Pinterest: A sprain may occur from damage to the ligaments. In as little as two weeks, minor sprains can heal. It may take six to twelve weeks or more for more serious sprains. See a doctor if you have thumb pain, especially if it persists for more than a few days.
How may a skier’s thumb be taped?
Self-taping instructions for non-professionals
On the inside of the thumb joint, apply the tape without straining. Next, gently draw the tape over the thumb’s palm side toward the hand’s side, and then over the thumb’s back toward the hand’s back.
Have you recovered completely from your UCL tear?
In the event of a minor sprain or partial tear, the ulnar collateral ligament can mend without surgery. Physical therapy, rest, and medical attention can aid in the healing of minor injuries. But for more serious injuries to fully heal, surgical reconstruction is necessary.
Does my skier’s thumb require surgery?
Understanding Skier’s Surgical Repair
Your injury could not heal properly on its own if your ligament is badly injured or stretched, or if there are injuries to the surrounding bone and tissues as well. You might require surgery. This can aid in the ligament’s healing and allow your thumb to move and function fully again.
How much time does it take for a skier’s thumb to recover?
It can be required to use screws or pins if a fracture also happens. It will take about three months to fully heal. Gamekeeper’s Thumb may occur if this injury is neglected and the ligament does not heal.
Which brace is better for thumb injuries caused by the UCL?
Thumb stress can be decreased, the UCL can recover, and other injuries can be avoided by wearing a comfortable, long-lasting splint like the ThumSaver MP, Fix Comfort Thumb Brace, or 3pp Ez FIT Thumb Spica Splint.
For how long does it take to heal from a UCL thumb tear?
The severity of this injury determines the suggested course of treatment. STABLE INJURIES: Although partial ligament tears may cause pain, the joint is nonetheless stable. Usually, the injury heals in 4 weeks, and by 6–8 weeks, typical function returns.
The thumb’s ulnar collateral ligament is located where?
The thumb’s ulnar collateral ligament is situated at the metacarpal-phalangeal joint, which is where the hand and finger bones connect, on the pinky side of the thumb. It enhances hand strength and grip while stabilizing the thumb’s base. Most injuries have a traumatic origin.
When someone has skier’s thumb, which ligament is impacted?
This is a damage to the metacarpo-phalangeal joint’s ulnar collateral ligament. The thumb is supported by this robust ligament while pinching or gripping, and damage to it may result in chronic thumb instability that impairs function.
How is a ruptured thumb ulnar collateral ligament treated?
Partial tears may be treated with splinting immobilization, but it is still wise to have a hand surgeon evaluate the patient. Three weeks is the usual suggested immobilization period. Physical therapy and rehabilitation can then be applied to these nonsurgically treated diseases.
How can a skier’s thumb be healed?
RICE stands for rest, ice, compression, and elevation. When treating a thumb injury, RICE can be helpful.
NSAIDs, or non-steroidal anti-inflammatory medications.
prescription medications for pain relief.
immobilization using a brace, cast, or splint
Physical therapy.
Operation.
What is the recovery time for skiers’ thumbs?
As you recover, your helper will give you instructions on how to begin thumb exercises to restore strength and range of motion. After your injury, this could happen as soon as three weeks or as long as eight weeks. Resuming an activity after suffering a sprain causes it to gradually worsen. Take a break from using your thumb set if it starts to pain.
What are the symptoms and clinical signs of a skier’s thumb?
Symptoms include pain in the web area between the thumb and index finger near the base of the thumb.
There is edema surrounding your thumb.
weakness or difficulty grasping between your thumb and index fingers.
Palpable tenderness at the thumb’s index digit side.
skin discoloration over the thumb.
Is the thumb of a skier permanent?
The ligament cannot heal properly since it has been completely injured and forced out of its original anchoring position. In order to restore the ligament to its original anatomical location, surgery is required. Other than that, there may be a lifelong loss of pinch strength and thumb stability.
How can a skier’s thumb be strengthened?
Place your hand and forearm on a level surface. The thumb you’re using needs to point upward.
Hold your thumb steady with your other hand just below the joint nearest your thumbnail.
Bring your thumb’s tip down. After that, straighten it.
Do this eight to twelve times.
Do this workout multiple times each day.
References
- Physiotherapist, D. (2023, April 29). Skier’s thumb (Ulnar collateral ligament injury of the thumb). Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/skiers-thumb/
- Mohseni, M., Sina, R. E., & Graham, C. (2024, February 1). Ulnar collateral ligament injury (Gamekeeper’s thumb). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482383/
- Wikipedia contributors. (2024, May 19). Ulnar collateral ligament injury of the thumb. Wikipedia. https://en.wikipedia.org/wiki/Ulnar_collateral_ligament_injury_of_the_thumb
- Skier’s thumb | The British Society for Surgery of the Hand. (n.d.). https://www.bssh.ac.uk/patients/conditions/32/skiers_thumb