Brachial Plexus
Introduction
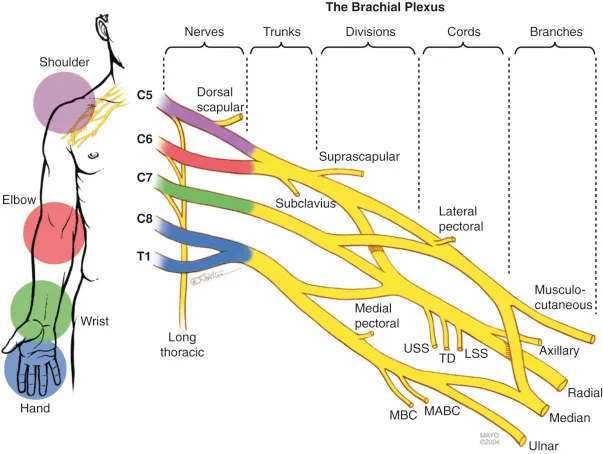
The brachial plexus is a network of nerves that originates from the spinal cord in the neck (C5 to T1 nerve roots) and extends through the shoulder to control muscle movements and sensation in the shoulder, arm, and hand. It is divided into five sections: roots, trunks, divisions, cords, and branches. Damage to the brachial plexus can result in weakness, numbness, or paralysis of the upper limb, depending on the severity and location of the injury.
The trunks are located between the anterior and middle scalene muscles in the neck’s posterior triangle. The brachial plexus and the axillary artery can be viewed as a sizable neurovascular bundle that supplies blood to the upper extremities via the axilla.
Structure
The brachial plexus is composed of five roots, three trunks, six divisions (three anterior and three posterior), three cords, and five branches. Along its length, the plexus has five “terminal” branches and many more “pre-terminal” or “collateral” branches, including the long thoracic nerve, the thoracodorsal nerve, and the subscapular nerve.
In cadaver dissections, the M or W shape formed by the musculocutaneous nerve, lateral cord, median nerve, medial cord, and ulnar nerve is frequently used to identify a portion of the brachial plexus.
Roots
Following their segmental supply to the neck muscles, the spinal nerves’ five roots are their five anterior principal rami. There are five distinct levels at which the brachial plexus emerges: C5, C6, C7, C8, and T1. The top trunk is formed by the merger of C5 and C6, the middle trunk is continually formed by C7, and the lower trunk is formed by the merger of C8 and T1. In certain situations, C4 or T2 are involved in prefixed or postfixed constructions.
The rhomboid muscles, which retract and rotate the scapula downward, are innervated by the dorsal scapular nerve, which originates in the superior trunk. The subclavius, a muscle involved in raising the first ribs during breathing, is innervated by the subclavian nerve, which has its origins in both C5 and C6.
The long thoracic nerve originates in C5, C6, and C7. The serratus anterior, which pulls the scapula laterally and is the primary mover in all pushing and reaching motions forward, is innervated by this nerve.
Trunks
These roots merge to form the trunks:
- “superior” or “upper” (C5-C6)
- “middle” (C7)
- “inferior” or “lower” (C8-T1)
Divisions
After that, each stem divides in half, creating six divisions:
- The lower, middle, and upper trunks’ posterior divisions
- When examining the body in its anatomical position, the anterior divisions are superficial to the posterior divisions.
Cords
The three cords or big fiber bundles are formed by the regrouping of these six divisions. The location of the cords about the axillary artery gives them their names.
- The three posterior divisions of the trunks (C5-C8, T1) combine to produce the posterior cord.
- The anterior divisions of the middle and upper trunks combine to create the lateral cord (C5-C7).
- The anterior division of the lower trunk is only continued by the medial cord (C8, T1).
Branches
The branches are listed below. While some branches originate directly from previous structures, the majority of branches originate from the cords.
The five “terminal branches” are on the left. These terminal branches include the ulnar, median, radial, axillary, and musculocutaneous nerves. Since both the median nerve and the musculocutaneous nerve originate in the lateral cord, they are intimately connected.
It has even been demonstrated that the musculocutaneous nerve branches out to the median nerve, strengthening their connection. Although they are extremely uncommon, a few variations in the branching pattern have been documented.
Supraclavicular branches
The C5 spinal nerve’s root is where the dorsal scapular nerve most frequently emerges. On rare occasions, it may originate from the brachial plexus’ superior trunk. The levator scapulae, rhomboid major, and rhomboid minor muscles are motorly innervated by the dorsal scapular nerve.
Suprascapular nerve
The suprascapular nerve, which emerges from the superior trunk, carries the C5 and C6 fibers. The suprascapular nerve provides sensory innervation to the glenohumeral and acromioclavicular joints, while the supraspinatus and infraspinatus muscles get motor innervation.
Long thoracic nerve
The long thoracic nerve is made up of the C5, C6, and C7 roots.
Subclavian nerve
This nerve originates from the superior trunk of the brachial plexus and contains the C5 and C6 spinal nerve fibers. The subclavius muscle is motorly innervated by the subclavian nerve.
Branches of the lateral cord
Two preterminal branches that arise from the lateral cord are the lateral pectoral nerve and the lateral root of the median nerve. Additionally, it produces the musculocutaneous nerve, one of the brachial plexus’s terminal branches.
Lateral pectoral nerves
The lateral pectoral nerves come from the lateral cord of the brachial plexus and carry the spinal nerve fibers C5, C6, and C7. Through their anastomoses with the medial pectoral nerves, the lateral nerves help innervate the pectoralis minor muscle.
The Lateral root of the median nerve
This little branch is one of the median nerve’s two roots. It rapidly combines to form the median nerve with the medial root, a branch of the medial cord.
The musculocutaneous nerve, a terminal branch of the lateral cord of the brachial plexus, carries the C5–C7 spinal nerve fibers. It is a mixed nerve that provides both motor and sensory function to the upper limb.
The musculocutaneous nerve’s motor fibers innervate the brachialis, coracobrachialis, and biceps brachii, which are the muscles in the anterior arm. The sensory fibers of the musculocutaneous nerve innervate the skin on the forearm’s lateral surface via the lateral cutaneous nerve.
Branches of the medial cord
The medial cord produces the medial pectoral nerve, medial brachial cutaneous nerve, medial antebrachial cutaneous nerve, the medial root of the median nerve, the ulnar nerve, and another terminal branch of the brachial plexus.
Medial pectoral nerves
The medial pectoral nerves come from the brachial plexus’s medial cord, which also houses fibers of the C8 and T1 spinal neurons. This nerve provides motor innervation to the pectoralis minor muscle and the lower sternocostal region of the pectoralis major muscle.
Medial brachial cutaneous nerve
The medial brachial cutaneous nerve sometimes referred to as the medial cutaneous nerve of the arm, is produced by the medial cord, which contains fibers from the C8 and T1 spinal neurons. This nerve provides sensory innervation to the inferior skin on the medial side of the arm.
Medial antebrachial cutaneous nerve
The medial antebrachial cutaneous nerve sometimes referred to as the medial cutaneous nerve of the forearm, is produced by the medial cord, which also contains T1 spinal nerve fibers. This nerve is sensory and innervates the skin of the arm covering the biceps brachii and the skin of the medial side of the forearm.
The Medial root of the median nerve
The medial root is one of the secondary origins of the median nerve. It joins the lateral root described above to produce the median nerve’s trunk.
Ulnar nerve
The ulnar nerve, the terminal branch of the brachial plexus’s medial cord, contains the C8 and T1 spinal nerve fibers. Like the median nerve, the ulnar nerve is a mixed nerve that innervates the hand and forearm both motorly and sensoryly.
The following receive motor supply from the ulnar nerve:
- The other forearm muscles—the medial ½ of the flexor digitorum profundus and the flexor carpi ulnaris muscle are not supplied by the median nerve.
- Every hand muscle, except the LOAF muscles (flexor pollicis brevis, abductor pollicis brevis, opponens pollicis, and lateral two lumbricals).
The following receive sensory input from the ulnar nerve:
- skin on the medial ½ of the palm’s anterior and posterior surfaces.
- the skin on the medial 1½ fingers’ anterior and posterior surfaces.
The following mnemonic is a simple method to recall the hand’s motor supply via the ulnar nerve.
The hand’s HILA muscles are supplied by the ulnar nerve:
- The flexor digiti minimi brevis, abductor digiti minimi and opponens digiti minimi are hypothenar muscles.
- Interossei muscles (dorsal and palmar interossei)
- Medial two Lumbricals
- Adductor pollicis
Branches of the posterior cord
The posterior cord of the brachial plexus is the origin of the subscapular, thoracodorsal, and axillary nerves as well as the radial nerve, another terminal branch.
Subscapular nerves
These two nerves are usually the superior and inferior subscapular nerves. Both of these nerves originate in the posterior cord, which also houses the C5 spinal nerve fibers. While the superior subscapular nerve innervates the superior portion of the subscapularis muscle, the inferior subscapular nerve innervates the teres major muscle and the remaining subscapularis muscle.
Thoracodorsal nerve
The thoracodorsal nerve, which arises from the posterior cord of the brachial plexus, carries the fibers of C7 and C8. This nerve provides motor supply to the latissimus dorsi.
Axillary nerve
Fibers from the C5 and C6 spinal nerves are carried via the axillary nerve, one of the terminal branches of the posterior cord. This mixed nerve innervates the shoulder region, providing both motor and sensory data. The axillary nerve supplies the teres and deltoid muscles as well as the skin that covers the deltoid muscle.
Radial nerve
The radial nerve is the second terminal branch of the posterior cord of the brachial plexus, which contains spinal nerve fibers C5–T1. This mixed nerve provides motor and sensory innervation to the arm and forearm.
The following receive motor supply from the radial nerve:
- Every muscle in the arm’s posterior region (triceps brachii muscle).
- Extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digitorum, supinator, brachioradialis, and anconeus are all muscles in the posterior compartment of the forearm. Extensor indicis, pollicis brevis, and longus, extensor digiti minimi, abductor pollicis longus).
The following receive sensory input from the radial nerve:
- The skin covering the back of the arm.
- skin on the forearm’s posterior, central surface.
- skin on the hand’s dorsum, the lateral surface.
Median nerve
Two roots that emerge from the brachial plexus’s medial and lateral cords combine to generate the median nerve:
- The terminal branch of the lateral cord is the lateral root of the median nerve.
- A terminal branch of the medial cord is the medial root of the median nerve.
- The median nerve splits into its terminal branches in the hand after traveling the length of the upper limb. Several areas of the hand and forearm get motor and sensory innervation from this mixed nerve.
The following are motors supplied by the median nerve:
- Every muscle in the forearm’s anterior (flexor) compartment, except the medial ½ of the flexor digitorum profundus and the flexor carpi ulnaris.
- Except for the adductor pollicis, all thenar muscles (abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis).
- Two lateral lumbrical muscles.
The following receive sensory input from the median nerve:
- The skin of the palm’s lateral ½.
- The skin on the lateral 2½ fingers’ rear surface.
- The skin on the lateral 3½ fingers’ anterior surface.
The following mnemonic is a simple method to recall the hand’s motor supply via the median nerve.
The hand’s LOAF muscles are supplied by the median nerve:
- Lateral two lumbricals
- Opponens pollicis
- Abductor pollicis brevis
- Flexor pollicis brevis
Function
With two exceptions—the trapezius muscle, innervated by the spinal accessory nerve (CN XI), and a region of skin close to the axilla, innervated by the intercostobrachial nerve—the brachial plexus is in charge of the cutaneous and muscular innervation of the whole upper limb.
Embryology
Similar to those in the brachial plexus, motor nerve fibers sprout from cells in the developing spinal cord’s basal plate and reach the ventral nerve root. Neural crest cells are the origin of the sensory nerve fibers in the dorsal nerve root.
Eventually, the dorsal and ventral nerve roots will grow together to form a spinal nerve. Dorsal primary rami and ventral primary rami are the divisions of spinal nerves. Nerves will grow into the limb in both dermatomal and myotomal distributions as the limb bud grows.
Anatomical Importance
Contributions from C4 and T2 are among the most prevalent brachial plexus variations. These spinal cord levels may contribute in different ways. For instance, a branch from T2 may be huge, yet a branch from C4 may be small.
The amounts found in a particular nerve can differ even with the normal levels involved in the brachial plexus’ development (see Netter picture). Variations in dermatomal distribution or dominant innervation to muscles may result from this.
Examination
Using an MRI scanner with a higher magnetic strength, such as 1.5 T or more, can adequately image the brachial plexus. MRI is preferred over other imaging modalities for imaging the brachial plexus because of its multiplanar capability and the tissue contrast difference between the brachial plexus and adjacent vessels.
Plain X-rays cannot evaluate the brachial plexuses, but CT and ultrasound scanning can view the plexuses to some extent. Although axial pictures provide insight into the nerve roots, coronal and sagittal planes are the best for imaging the plexuses.
To obtain more information and assess the anatomy more thoroughly, innovative sequences such as MR Myelolography, Fiesta 3D, and T2 cube are employed in addition to the standard sequences, which typically use T1 WI and T2 WI pictures in different planes for imaging.
Clinical Importance
Erb’s palsy is damage to the higher roots of the brachial plexus, often C5–6. The most frequent cause of it is a stretching injury sustained during a challenging vaginal delivery.
Nerves affected – Most impacted are the peripheral nerves that come from the C5–6 roots. This encompasses the axillary, suprascapular, musculocutaneous, and subclavial nerves.
Muscles affected – biceps brachii, brachialis, coracobrachialis, deltoid, teres minor, supraspinatus, infraspinatus, and subclavius.
Motor functions affected – shoulder flexion, shoulder abduction, shoulder lateral rotation, and forearm supination.
Sensory functions affected – feeling along the upper limb’s lateral side (C5-6 dermatomes).
The unopposed activity of the pectoralis major causes the affected limb to hang limply and rotate medially. The removal of the biceps brachii causes the forearm to pronate. Because the wrist flexors have a normal tone in comparison to the weak wrist extensors, the wrist is weakly flexed. This posture, referred to as the “waiter’s tip,” is typical of Erb’s palsy.
Klumpke’s palsy
Klumpke’s palsy is characterized by damage to the lower roots (C8-T1) of the brachial plexus. Although it is far less prevalent than Erb’s palsy, it is likewise most frequently linked to a challenging vaginal delivery.
Nerves affected – The ulnar and median nerves, which are peripheral nerves originating from the T1 root, are most impacted.
Muscles affected – the intrinsic hand muscles
Sensory functions affected – feeling throughout the upper limb’s medial side (C8-T1 dermatomes).
The primary feature of Klumpke’s palsy is the clawed hand. This results in paralysis of the lumbrical muscles, which normally stretch the interphalangeal joints (IPJs) and flex the metacarpophalangeal joints (MCPJs). When paralyzed, the fingers flex at the IPJs and lengthen at the MCPJs, giving the appearance of claws.
Injury
Different arm portions’ feeling or mobility may be impacted by brachial plexus injury. Pushing the shoulder down and pulling the head up can injure the nerves by stretching or tearing them. Malpositioning-related injuries typically impact the brachial plexus nerves instead of other peripheral nerve groups.
There are very few methods to prevent such injuries since the brachial plexus nerves are so sensitive to posture. Newborns and victims of auto accidents are the most frequent groups to sustain brachial plexus injuries.
Stretching, illnesses, and wounds to the axilla or lateral cervical area (posterior triangle) of the neck can all result in injuries. The symptoms might range from anesthesia to total paralysis, depending on where the lesion occurred. One way to determine the extent of paralysis is to test the patient’s range of motion and compare it to their usual side.
A hard landing where the shoulder widely separates from the neck (as in motorcycle accidents or falling from a tree) is a common cause of brachial plexus injuries. These strains have the potential to avulse the spinal cord’s roots or tear the brachial plexus’ upper sections. Excessive neck stretching after delivery frequently results in damage to the upper brachial plexus in infants.
Research has indicated a correlation between a newborn’s weight and brachial plexus injuries; nevertheless, at most birth weights, a significant number of cesarean deliveries are required to avoid a single harm.
The deltoid, biceps, brachialis, and brachioradialis are among the muscles supplied by C5 and C6 that become paralyzed in cases of upper brachial plexus injury. Such injuries also frequently result in a loss of sensation in the lateral portion of the upper limb.
Although much less often, an inferior brachial plexus injury can happen when someone grabs something to break a fall or when a baby’s upper limb is twisted too much during birth. In this situation, the hand’s short muscles would be impacted, making it unable to make a full fist.
The following considerations must be made by the doctor during clinical examination to distinguish between preganglionic and postganglionic injuries. Preganglionic injuries result in ipsilateral Horner’s syndrome, loss of function of muscles supplied by branches arising directly from roots, pain in an otherwise insensate hand, loss of sensation above the level of the clavicle, and elevation of the ipsilateral diaphragm due to phrenic nerve palsy and winging of the scapula due to long thoracic nerve palsy.
The neurological condition known as acute brachial plexus neuritis is typified by the development of intense shoulder pain. Compression of the cords can also result in erythema, paresthesia, numbness, weakness, and discomfort that travels down the arm. People who undertake jobs above their head and have extended hyperabduction of the arm are likely to get this type of injury.
Penetrating wounds
The majority of penetration wounds are more difficult to heal and need to be treated right away. A serious knife wound to the brachial plexus, for instance, may cause damage or even sever the nerve. Action potentials required to innervate the particular muscle or muscles that the nerve innervates may be inhibited, depending on the location of the cut.
Injuries during birth
When an infant’s anterior shoulder cannot pass below the pubic symphysis without mechanical assistance during head delivery, brachial plexus damage may result. The baby’s shoulder may expand as a result of this manipulation, causing varied degrees of brachial plexus damage. Shoulder dystocia is the name given to this kind of damage. Obstetric brachial plexus palsy (OBPP), or true brachial plexus damage, can result from shoulder dystocia.
The United Kingdom and the Republic of Ireland have a lower incidence of OBPP (0.42 per 1000 births) than the United States, which has 1.5 cases per 1000 births. Although there are no recognized risk factors for OBPP, a newborn’s risk of developing OBPP is increased by a factor of 100 if they have shoulder dystocia.
Larger babies are more likely to sustain nerve damage, which has been linked to birth weight. However, delivery techniques also have a role. Doctors must be able to deliver a newborn with precise and gentle movements to reduce the likelihood of harming the kid, even though this is extremely difficult to prevent during live birth.
Tumors
Malignant peripheral nerve sheath tumors, neurofibromas, and schwannomas are among the malignancies that can develop in the brachial plexus.
FAQs
What are the five brachial plexuses?
Finally, the brachial plexus gives rise to five main terminal branches that are responsible for most of the motor and sensory innervation of the upper limb, and they include the musculocutaneous, axillary, radial, median and ulnar nerves.
What is a dermatome?
Dermatomes are parts of your body’s skin that depend on particular spinal nerve connections. Dermatomes are comparable to maps in this regard. Because of this relationship, dermatomes can assist a medical professional in identifying and diagnosing disorders or issues that impact your spine, spinal cord, or spinal nerves.
How do you test for brachial plexus?
The classic test is a wall-press test. The patient may not be able to raise their arm when they have BPI. The examiner should support the patient’s arm with one hand while asking them to push forward as though they were opening a door. The examiner should simultaneously hold the scapula’s lower pole in a different hand.
What nerve is in the bicep?
After exiting the axilla, the musculocutaneous nerve quickly descends into the coracobrachialis muscle fibers. The musculocutaneous nerve descends between the brachialis and biceps brachii muscles in the anterior compartment of the arm, supplying them with blood.
What are the myotomes?
A myotome is ‘a collection of muscles innervated by a single spinal nerve root’. They are clinically valuable because they can establish whether the spinal cord has been damaged and at what degree.
References
- TeachMeAnatomy. (2025a, February 10). The brachial Plexus – Sections – Branches – TeachMeAnatomy. https://teachmeanatomy.info/upper-limb/nerves/brachial-plexus/
- Wikipedia contributors. (2024f, December 29). Brachial plexus. Wikipedia. https://en.wikipedia.org/wiki/Brachial_plexus
- Brachial plexus. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/brachial-plexus
- Brachial plexus. (2023, August 14). StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK531473/


One Comment